Stroke Helpline
Monday to Friday: 9 am to 5 pm
Saturday: 10 am to 1 pm
Sunday: Closed
Supporter Relations
Saturday: Closed
- Professionals

Going on holiday after stroke
Holidays are an important part of life, and this guide can help you with holiday planning if you have a health condition or disability after a stroke.
The information on this page can be accessed in other formats:
- Download our PDF and large print Word document Holidays and stroke.
- Order your printed copy from our shop.
- Request a braille copy by emailing [email protected].
On this page:
Can I still go on holiday after a stroke? Types of holiday Flying after a stroke Do I need travel insurance? Travelling with medication
Can I still go on holiday after a stroke?
If you're thinking about getting away, there are various holiday options to choose from with different levels of support.
If a stroke has left you with mobility problems, you may prefer to book with a specialist travel agency that can arrange care and equipment for you. Some holiday packages also include an organised programme of activities, such as sports and outdoor activities or visits to local attractions, while others only offer accommodation so that you can do your own thing.
Coronavirus (COVID-19) and holidays
We know that holidays and travel may be affected by changing social distancing rules for some time. You need to check on the latest rules about your journey and destination before travelling.
If you are more vulnerable due to a health condition, you will need to follow the advice you are given to reduce your risk of infection.
Air travel after a stroke
People often ask whether it is safe to fly after a stroke. There is no hard and fast answer to this. Most airlines will not carry someone within days of a stroke, but the rules vary between airlines and countries.
In the weeks after a stroke you are at the highest risk of another stroke. So the most important thing is to get individual advice from your hospital or GP about the likely risks of travelling.
In the UK, the Civil Aviation Authority suggests waiting 10 days after a stroke before a flight. But if your condition is stable you may be able to fly after three days.
Each airline will have its own rules on flying with medical conditions, so you need to check with the airline before flying. You may be asked to provide a doctor's note or certificate.
Immediately after a stroke, you may need to attend check-ups and have medical treatment. The full effects of a stroke may take time to emerge. You might need help with these effects, and you might need to attend therapy sessions. So it's really important to get medical advice about your own situation before you travel.
If you have a stroke caused by a clot (ischaemic stroke) you will be given medication to reduce the risk of blood clots. This needs to be taken regularly to be effective. So you need to plan carefully before travelling to make sure you have the right medications with you, and that you take them at the right times.
Carry medication in both your hold bag and hand baggage, in case any of your luggage gets lost.
If you have a stroke while on holiday, you might need to take a flight to get back home. If you have medical insurance, your insurance company should give you help and advice on medical treatment and getting back home. You can also contact the local British Consulate, which can offer advice and practical support.
Travel and blood circulation
During a flight, the air pressure inside an aeroplane cabin is lower than it is on the ground. So when you fly, you have a bit less oxygen in your blood than normal. This may affect certain people with a heart problem or breathing condition, so ask your GP if this applies to you.
On a long flight, you are likely to be inactive for a period of time which makes you more likely to develop a deep vein thrombosis (DVT). A DVT is a blood clot in a vein, often in the leg.
The best way to reduce the risk of a DVT on any long journey is to drink plenty of water, and stay active. Simple exercises like flexing your ankles or walking around will improve your blood flow. Do this regularly during the journey.
If you have had a DVT in the past, and you don't take anti-coagulation medication, ask your GP for advice before a long journey.
Some travellers wear compression stockings during a flight. However, you should not wear these if you have peripheral artery disease (PAD). This condition reduces blood flow in your legs, so wearing the stockings can reduce blood flow too much. Ask your GP or pharmacist for individual advice.
Getting around the airport
All European airports should have facilities to help you move through the airport and get on and off the plane if you have reduced mobility. Airline crew are not able to provide personal care, and the airline may insist that you travel with a companion if you are unable to eat, understand safety briefings or reach emergency exits without help.
Most airlines will carry two items of mobility equipment for free. This should be in addition to your baggage allowance. If you have a wheelchair, it will be stored in the hold. You should tell your airline, travel agent or tour operator before you travel if you're taking a battery-powered wheelchair or mobility aid.
Contact the airline to discuss your requirements, and any additional help you will need on the flight, at least 48 hours in advance.
Do I need travel insurance?
It is important to have travel insurance, especially if you are going abroad.
Make sure you declare that you've had a stroke when arranging your insurance and check that you are fully covered. Many policies will exclude conditions that you had before you took out the policy (known as pre-existing medical conditions). This varies between policies, but it could mean that you would have to pay for any costs relating to these conditions. There are specialist travel insurers that provide cover for pre-existing conditions.
Specialist insurance from All Clear
The Stroke Association has a partnership with specialist medical travel insurer AllClear Travel, which provides comprehensive cover to stroke survivors. Find out more at our travel insurance page .
Global Health Insurance Card (GHIC)
The Global Health Insurance Card (GHIC) replaces the European Health Insurance Card (EHIC) for most people. Despite the name, it allows you to receive state-provided healthcare only in European countries. Treatment is at the local cost, or sometimes for free. It will cover your treatment until you return to the UK. It also covers the treatment of pre-existing medical conditions.
It won't cover certain costs, including the cost of returning you to the UK, so you still need to get private travel insurance as well.
How to apply
Visit the Global Health Insurance Card page on Gov.uk for full details of eligibility and a link to the free application page. A GHIC is free of charge. If you are charged a fee while applying online, leave the site, go to the NHS GHIC page .
European emergency number: 112
Dial 112 from anywhere in the UK or Europe to be connected to local emergency services.
Travelling with medication
If you carry medication or medical equipment such as syringes in your hand luggage, you should bring documentation like a doctor's letter. You should also carry a copy of your prescription. As well as helping you avoid any problems at airline security and customs, this will be useful if you need medical help while you're away.
Make sure you take enough medication with you in case you are unexpectedly delayed. If you are travelling across time zones, ask your pharmacist for advice about timing your medication.
It may be possible to take oxygen cylinders on board a plane. You need to contact the airline about this before you book.
Liquid medication
Current rules on liquids in hand luggage say that you can only take containers of up to 100ml. However, you can carry liquid medication of more than 100ml in hand luggage, as long as you have a doctors letter. Airport staff may need to open the containers to screen the liquids at the security point. For more information about this, contact the airline.
Check before you fly
Always contact the airline or travel company if you have any questions about health conditions or support for disabled travellers. There may be restrictions on taking medications into some countries or specific health advice on travel in a particular area.
Check beforehand with the embassy of the country you're travelling to, or check the government's foreign travel advice.
Related pages
Useful links.

Information Line: 0345 1307172
Travel insurance after a stroke, please note this article was created to promote our affiliate partnership with medical travel compared.

We regularly get asked about travel insurance. As stroke survivors ourselves we know how difficult it can be to find affordable insurance that covers you for the right things should you fall ill whilst on holiday.
We answer some of the common questions about travel insurance after a stroke below.
Can I get travel insurance after a stroke? Life after a stroke can feel very different to how it did before, but that doesn’t have to stop you doing what you love. While recovery is unique for every stroke survivor, the opportunity to get away from it all on a holiday or trip to another country can provide some much-needed relaxation and enjoyment (just make sure you have the all clear from your doctor before you travel).
The good news? You can get travel insurance that’s designed specifically for people who have had strokes. It’s just a case of finding the right cover for you, which is where Medical Travel Compared can help.
How to find the right cover We know that strokes come on suddenly and often without warning. So when you have a history of strokes or mini-strokes (TIA), it’s important you know that if one should happen while you’re away, you can get the medical help and support you need.
Without the right travel insurance policy in place, you could find yourself financially out of pocket due to expensive medical bills – not something you want to be worrying about in the lead up to – or during – your getaway.
Medical Travel Compared can save you time and hassle searching for travel insurance on lots of different sites, by helping you compare relevant policies from over 40 leading insurers – all in one place. All they’ll need are a few details about your medical history and past strokes, so they can find the right cover options for you.
What will be covered? This will vary depending on the insurance provider, but you can usually expect to be covered for:
- Emergency medical expenses
- Repatriation
- Cancellation and curtailment
- Loss of medicine (including if it’s stolen)
How much will it cost? The cost of travel insurance for stroke survivors will vary depending on your medical history and the severity of any long-lasting symptoms you have. Generally speaking, if it’s been three months since your last stroke and your condition is stable, your premiums should be relatively low.
Find Out More
For every travel insurance policy bought via this page, Different Strokes will receive a donation. This will not affect the price you pay, so benefits stroke survivors through accessing appropriate travel insurance while earning important funds for Different Strokes.

My Neuro Survey
Everyone deserves access to the right care, treatment and support at the right time, no matter who you are or where you live. But too often this isn’t the case.
Please share your experiences and help improve services for everyone affected by neurological conditions now.

Celebrate Jim’s Birthday as he Raises Funds for Different Strokes
Jim has been an invaluable part of our community for over 17 years, bringing hope and support to many stroke survivors. This year, as he approaches his 70th birthday on July 26th, Jim is marking this milestone with a series of incredible fundraising challenges to support his local group.

Join Our Webinar: Understanding PFO Closures – Insights from Stroke Survivors
Join us to gain valuable insights from stroke survivors about their PFO closure procedures

Join us and meet other stroke survivors this September!
Join us at one of our “Living Beyond Stroke: Community and Connection” conferences, where we celebrate life after stroke and the importance of community.

Sovereign Health Care £2,500 Grant
We’re absolutely thrilled to share the wonderful news that Different Strokes has been awarded a generous grant of £2,500 to bolster our regional efforts in West Yorkshire.

Share your experience of post-stroke fatigue to help others
Different Strokes is looking to recruit volunteers for taking part in research in partnership with the Universities of Birmingham and Cambridge. This would involve being filmed talking about your experiences of post-stroke fatigue.
GET IN TOUCH
Information : 0345 1307172 Admin Line : 01908 317618
Email Us Different Strokes 9 Canon Harne tt Court Wolverton Mill Milton Keynes MK12 5NF

NEWS AND EVENTS
Reclaiming lives after stroke.
Telephone Hours
Opening hours.
- Mon-Fri: 8:30am - 8pm
- Sat: 9am - 5:30pm
- Sun: 10am - 5pm
- 28th August: 9am - 5pm
Stroke Travel Insurance
Travel Insurance for Stroke
If you are thinking of travelling abroad or within the UK following a stroke or transient ischaemic attack (TIA or mini-stroke), then let this AllClear guide to specialist medical travel insurance help you through the process. At AllClear we are committed to giving high-quality service to our customers, and our tailored, comprehensive travel insurance policies are especially designed to cover pre-existing medical conditions such as a stroke.
Regardless of your age we can provide 5-star cover for you and your travelling party. As long as the FCDO or the WHO are not advising against travelling to your chosen destination then we can get you covered.
AllClear Comprehensive Travel Insurance for Stroke or TIA (Mini-Stroke)
Each year in the UK, 100,000 people suffer from a stroke or TIA according to Stroke Association – that’s around one stroke every 5 minutes! And with over 1.2million stroke survivors in the UK, it’s vital that we can supply you with the kind of medical insurance cover that you need.
Following a stroke we understand that you might be hesitant to travel, so there’s a few things you might want to check before making your decision:
- You haven’t been advised not to travel by a medical professional
- Think about the destination you’re travelling to and if it is suitable for you regarding physical exertion etc
- If you feel that your destination is suitable and that you are confident to travel then you’ll need to have a suitable medical travel insurance policy in place before you leave the UK that will take care of any costs for emergency medical treatment abroad. That’s where AllClear can provide you with the added satisfaction of knowing that you have a 5-star comprehensive insurance policy in place that will protect you financially should you require any emergency treatment while away
If the worst happens while away abroad it’s bad enough that you are far from home, family and friends, so you don’t want the added pressure and worry about paying the costs of any emergency medical treatment you might require as a result of your stroke or TIA.
Medical expenses abroad can accumulate and be significantly costly. They can leave you or your loved ones with a life-changing debt to pay. Should you require medical transport back to the UK, this alone can be tens of thousands of pounds.
Our AllClear policies can cover you for emergency medical expenses, including repatriation, up to an unlimited amount. We can offer you cover for cancellation as well as personal property and a whole host of additional, optional extras to enhance and personalise your policy to suit your specific needs.
Do you need Travel Insurance for Stroke or TIA
With so many different things to consider and arrange when booking a holiday, it’s so easy to forget why we need travel insurance . Following a stroke, even if you go on holiday in the UK, you should have a medical travel insurance policy in place to protect you from things like cancellation or curtailment costs that might occur.
Should you or a travelling companion require medical transport repatriation back to your local area then this may not be covered by the NHS. When travelling outside of the UK it is simply essential to have medical travel insurance following a stroke/ TIA . If you have any other pre-existing medical conditions then they should also be covered by your insurance provider.
At AllClear, our insurance policies will cover up to unlimited costs of any emergency medical expenses. A study by The Independent found that a claim is made every minute by UK residents abroad . A comprehensive AllClear medical travel insurance policy can give you the cover you need to feel safe and secure within your travels following a stroke or TIA.
One policy for the Whole Family following a Stroke
Our 5-star rated AllClear policies are designed to cover singles, couples, families or even large groups. You don’t need to have separate policies if you are travelling with loved ones or friends. Let AllClear make it simple and easy and give all of your party the same policy, regardless of individual age or pre-existing medical conditions.
Get everyone covered in one place at the same time with a comprehensive medical travel insurance policy from AllClear.
How much will your Travel Insurance for Stroke or Mini-Stroke cost?
Your travel insurance policy premium will be based on any pre-existing medical conditions that you declare to start with. Then the cost of specific medical treatment in the country you are going to as well as the length of time you will be away for will also be contributing factors.
Any optional extras that you add to your policy to enhance it will also affect the final premium.
What if Your Stroke or TIA Was Many Years Ago?
If you still take any kind of prescribed medication as a result of having a stroke or transient ischaemic attack (TIA or mini-stroke) then you will still need to declare it on your insurance policy, no matter how long ago it was. This is so we can see that you are taking medication following the stroke and that may affect any treatment you receive while you’re away which can alter the costs.
Be sure to read our guide on travelling after a stroke .
Should You Talk to Your GP Before You Travel?
You may want to speak to your GP or medical practitioner if you are planning to travel following a stroke or mini-stroke. The air pressure inside of a plane is lower than we breathe on the ground level, which results in less oxygen being carried in your bloodstream. So let your doctor know you’ll be flying – in case you need any oxygen to be provided during your flight.
After a stroke, you’re at greater risk of developing a clot in the leg during a flight. Make sure you keep active on a flight to prevent clots, including standing up every 30 minutes or taking a walk along the plane.
In addition, it may be worth buying compression socks to wear during your flight. Consider booking seats with extra leg-room to make your journey as comfortable as possible. Or even arrange priority boarding. The aim is to make your trip as stress-free as possible.
All Clear Enhanced Cover and Optional Extras
At AllClear we have lots of ways to design your policy to suit your individual needs. Should you be going on a cruise or a skiing holiday, then we can offer you the specific cover you’ll require. Make sure you let us know of any specialist activities you are thinking of doing and we will let you know what cover you will need.
With a number of our optional extras available such as gadget cover , we are sure you will find the right policy with AllClear.
Cruise Holidays following a Stroke
If you are thinking of going on a cruise holiday following a stroke then it’s important that you have the correct and adequate cover in place before you travel. Should you require a medical helicopter to transport you to the nearest medical vicinity then you’ll need to ensure that your policy will cover that specific expense.
Add AllClear cruise insurance to your policy and travel safely and securely.
Golf Holidays following a Stroke
Thinking of going on a golf holiday following a stroke or TIA? We at AllClear have specialist golf travel insurance to give you that extra protection you will need. Add golf cover to your policy and enjoy a few rounds with 5-star insurance to cover your whole game.
Covid-19 and Stroke
Following a stroke or TIA, patients are more likely to contract pneumonia as a complication following a positive COVID-19 Coronavirus test result, according to Stroke Association . This means that we need to be extra cautious following a stroke/ TIA (mini stroke) Before we can offer you travel insurance we must have a few things checked:-
Are you fit to travel?
As long as you haven’t been advised not to travel by a medical professional then we are happy to give you a quote.
Are any Travel Restrictions in Place?
Providing that there are no current travel restrictions in place by the FCDO or the WHO then we are happy to offer you cover!
Does having a Stroke or Mini-Stroke Limit your Travel Ability?
Following a stroke you may find it more difficult to get travel insurance from your usual provider. That’s why you’ll need a specialist medical travel insurance provider to give you the cover you need. Wirth a medical specialist insurance provider like AllClear we will be able to offer you comprehensive medical travel insurance with a whole host of benefits so you can still enjoy your much-loved holidays away.
At AllClear we can offer you single trip cover with a maximum duration limit of 365 days or an annual multi trip policy, which will cover any amount of holidays you choose to go on during a 12 month period. We believe everyone deserves the right to travel following a stroke or mini-stroke.
What Should a Travel Insurance Policy for a Stroke or TIA Cover?
You’ll need to declare your stroke as well as any other pre-existing medical conditions you might have.
- Emergency medical expenses – cover for stroke/ TIA (mini stroke) and any emergency medical expenses
- Cancellation and curtailment – cover for the cancelation of your holiday and also for curtailment, should you have to come home early due to medical circumstances
- Baggage and Personal Property – Your passport, bags, personal possessions and cash can also be covered should they be lost, stolen or damaged while you’re away
- Gadget Cover – your medical travel insurance policy can also cover any gadgets and smart devices that you might need extra protection for
SWIPE TO COMPARE POLICIES
* If you buy a policy which includes cancellation cover. / All these figures are per person and per trip.
Simple 3 step quote process
1. call us or click a quote button on our site, 2. complete our simple medical screening process, 3. get your quotes, why choose all clear for stroke travel insurance.
We hope you have found this guide to travelling following a stroke helpful and we hope you can enjoy your travel plans in the future with a policy you can trust. So why choose AllClear for your medical travel insurance needs? We have been committed to giving the highest level of service and product for over 20 years and our customers have given us a 4.9 Trustpilot rating.
What our Customers Say
Here’s what a recent customer had to say:
We’re very proud to have been awarded many awards and accolades for our commitment to service, product and customer satisfaction. When you travel with AllClear you are travelling with a medical insurance provider specialist. So leave it in the hands of the experts and call AllClear today!
Written by: Letitia Smith | Travel Insurance Expert Last Updated: 6 August 2024
† Based on Trustpilot reviews of all companies in the Travel Insurance Company category that have over 70,000 reviews as of January 2024. AllClear Gold Plus achieved a Which? Best Buy.
Policy Wordings
Modern Slavery Statement
MaPS Travel Insurance Directory
Earn rewards by sharing with friends
- Get covered in 2 minutes
- 1,000's of medical conditions considered
- £10m medical cover
- 14 Day Cooling Off Period
Stroke Travel Insurance
Save 15%Ɨ online
Finding affordable travel insurance after a stroke can be daunting, but we’re here to help. There are over 1.2 million stroke survivors in the UK and more than 100,000 strokes happen every year – our aim is to make purchasing stroke travel insurance the easiest part of your trip.
What cover levels are available on travel insurance for stroke victims?
We pride ourselves on being medical travel insurance specialists. Cover for medical conditions is available on all of our policy types and we provide 100’s of policies for stroke victims each year. Cover levels includes:
Up to £10,000,000 for medical emergencies , such as:
- If you need emergency medical attention
- Hospital benefit
- Repatriation
- Mobility and disability equipment
As well as:
- Up to £5,000 cancellation and curtailment cover
- Up to £4,000 for lost, stolen or damaged possessions
- Up to £750 to cover your travel documents
- Up to £2,000,000 for personal liability
- Up to £50,000 for legal advice
Get A Quote
Why Choose Get Going?
Over 1000 medical conditions considered
24/7 emergency medical assistance team, £10m cover for emergency medical expenses, 93% of customers have rated us 4 or 5 stars $.
SAVE 15%Ɨ BUYING ONLINE!
Safe travel after a stroke
Experiencing a stroke is a difficult time for both you and your wider family. When you’re getting everything back on track, even if you’ve been left with mobility problems, you should be able to get away and have a holiday. There are plenty of tour operators that will specialise in offering a tailored package and it will be worth spending some time researching the right trip for you.
Once you have a holiday in mind, you need to get an adequate travel insurance policy. Use our bespoke medical screening process to get your quick quote . We won’t ever share your information with third party companies and your screening is entirely confidential.
- Before you travel, take the time to save the emergency assistance number in your phone and if you’re travelling with someone, in their phone too.
- If you are travelling with medication, always keep these in your hand luggage. Make sure that any medication is labelled accurately and has your full name on it.
- There are a number of things you can do travel safe after a stroke. Importantly, you should always consult your GP before travelling, they will be able to Offer you advice specific to your circumstances.
- Always keep your medication in your hand luggage and in it’s original packaging. It may also be wise to carry an original copy of your prescription, just in case.
- Before travelling make sure you have our emergency assistance number saved in your phone and written down.
- Also note down the details of our GP service, just in case you need to seek advice whilst abroad.
We offer up to £10,000,000 in case of any medical emergency you could face. This includes medical attention, emergency replacement of prescription medication, plus mobile and disability equipment.
We understand that whether you, a family member or close friend experiences a stroke, going away can feel more daunting, but we’re here to provide specialist cover so you have nothing to worry about.
Frequently Asked Questions
Getting travel insurance after a stroke may seem like it is going to take a lot more of your time and potentially a lot more of your spending budget! Get Going are medical travel insurance specialists. We consider and cover 1000’s of medical conditions every year and regularly provide travel insurance for stroke patients.
Applying for travel insurance after a stroke can stir concern that you’ll be faced with sky high premiums. Get Going provides extremely competitive premiums, even after medical conditions are declared, this is part of what makes us medical travel insurance specialists. The final cost of your policy will be dependent on your policy type, cover level, any additional extensions or activity packs and your final medical declaration.
The best travel insurance for stroke patients is one that is able to cater for your medical history. Once you have that part, you might then look for a policy that meets your cover level requirements and has all of your medical conditions accurately declared upon purchase. If your medical status changes between the time your purchase your insurance and the intended date of travel, give us a call and we can advise based on your new medical status.
What our customers say
Ms Bowditch
“Hi , I’m writing to let you know just how lovely your staff are. I had to phone yet again to alter my travel insurance due to the Corona virus, I spoke to a young lady called Monica this m... Ms Bowditch
Mr Phillips
“Very satisfied, I will contact you before our next holiday which we hope to arrange in September.” Mr Phillips
“Had to change holiday date and all completed with ease with a quick phone call. At NO EXTRA cost what a nice change well done.” Mr Reece
Mrs Tullock
“Unfortunately had to cancel cruise to Alaska due to husband’s sudden illness 6 days before due to go. Once I set the ball rolling for an insurance claim and received necessary document... Mrs Tullock
“I don’t normally leave feedback but after dealing with Paul I have to commend you on an excellent service. It was a pleasure to deal with a polite competent person who sorted out my qu... Mrs Arlett
ƗPlease note, Get Going ‘s online prices automatically include a 15% discount against our Customer Service Centre prices. This is discounted from our core policy price before you add any additional cost of optional extensions or additional medical premium.
$Get Going has been rated 4.7 out of 5 (Excellent) based on over 7000 customer reviews on Trustpilot. Based on Trustpilot data 2024
Stroke Travel Insurance
Compare cover from as little as £19.76*.

Tommy has over 15 years experience within the insurance industry, and his primary focus is helping travellers find the right cover for their medical conditions.
Can you get travel insurance if you have had a stroke or TIA?
Having a stroke should not prevent you from travelling abroad. Find out more about getting travel insurance after a stroke.
And, since there are more than 1.3 million stroke survivors in the UK , it’s a good job that there are plenty of specialist medical travel insurance providers who can cover people who have had a stroke or TIA (mini-stroke) in the past.
If you’ve had a stroke in the past, stroke travel insurance cover provides you peace of mind - knowing that should you become unwell or face a medical emergency on holiday, you’ll be taken care of. With multiple types of cover including single-trip and annual multi-trip insurance , you can tailor your insurance to suit you.
Specialist Medical Cover
We only work with providers who specialise in covering pre-existing conditions.
No discounts. No pressure. We’ll always show you the best prices from providers.
Declaring your condition
Even if you had a stroke a long time ago - it’s still important to declare it with us when comparing travel insurance.
Once you do, it’s likely that you might be asked a few questions, such as:
- How many strokes have you had?
- How long ago was your last stroke?
- Are you awaiting surgery for this condition or for any scans?
- Do you currently use any mobility aids?
- Have you had any transient ischaemic attacks (TIA) since your last stroke?
The answers you provide help insurance providers to determine the more specific nature of your condition, while getting a clearer insight into your medical background.
This helps them to offer you the appropriate insurance for you after a stroke when you start comparing quotes.

Top tips for travelling if you've had a stroke
Dr Sarah Jarvis is the Clinical Director of the Patient Platform, an active medical writer, broadcaster, and the resident doctor for BBC Radio 2.
Having had a stroke or TIA (sometimes called a 'mini stroke') doesn't automatically mean you can't go on holiday. But depending on how long ago your stroke was, and what symptoms you've been left with, you will need to take a few extra precautions to make sure your trip goes smoothly.
- If you've had a stroke in the past few months, check with your doctor whether they think it's safe for you to fly. You certainly shouldn't fly the first two to three weeks after a stroke – this is the time your problems are likely to be most severe and you're most likely to develop other issues related to your stroke. However, if your stroke was caused by a bleed into the brain (rather than the more common clot on the brain) you may need to wait longer.
- If you have mobility problems as a result of your stroke, consider booking with a travel agency that provides a range of activities tailored to your needs. They should also be able to offer options that have step-free access and are wheelchair accessible.
- It's very common to tire more easily if you've had a stroke. Take into account the length of travel involved in getting to your destination and consider booking trips that don't involve early morning or late-night transfers.
- If you've had a stroke, you're at higher risk of a clot on the leg (a deep vein thrombosis or DVT) that could travel to your lungs. Reduce the risk by doing simple exercises to keep your legs moving if you can (most airlines have examples in their in-flight magazines), avoiding alcohol and drinking plenty of non-alcoholic fluids. Speak to your doctor about whether elastic compression stockings might help.
For more tips check out my full guide here .
What does stroke travel insurance typically cover?
You can expect this type of cover to include the same things that a standard travel insurance policy would include - but you can also claim for stroke-related medical issues (whereas you otherwise wouldn’t be able to).
This will normally include:
- Lost, Stolen or Damaged Personal Belongings: Including any medication you need to treat your condition.
- Emergency Medical Expenses and Repatriation: Specifically including any stroke-related medical expenses incurred by emergency medical treatment.
- Cancellation and Curtailment: If you suddenly decide to cancel your trip or end up cutting it short.
- Travel Delay: This won’t always be included, check with your provider.
- Personal Liability: If you cause accidental damage to another person or someone else’s property - cover is provided.
You can compare this type of cover across a range of leading providers, click below to get started.
Optional extras
Also, feel free to add any optional extras that you need - such as gadget cover, cruise cover or winter sports cover.
This may increase your premium, but it’s definitely something to consider when shopping around, especially if you have different types of holidays planned.
- Gadget cover
- Cruise cover
- Winter sports cover
Get cheap quotes from specialist stroke travel insurance providers
Comparing quotes will make it much easier to find the right travel insurance policy to cover your medical conditions with pre-existing medical travel insurance.
We work with plenty of specialist providers, and once you tell us about your trip and medical condition(s) you’ll be able to compare competitive quotes, all in one place - saving you money and precious holiday-planning time.
Rated Excellent
Trusted by thousands of people like you who've reviewed us on Trustpilot.
No phone calls or paperwork. Join millions who've sorted cover online in minutes.
Frequently Asked Questions
With us you can compare specialist stroke travel insurance across a range of providers. Get a quote today and start comparing competitive cover before you embark on your trip.
Premiums vary depending on the nature of your condition - but it’s still possible to compare competitive quotes with us and find a suitable policy for a reasonable cost. Get a quote .
Although not as serious as a stroke, if you have had TIA, you should absolutely purchase travel insurance that covers this particular condition. If you don’t, then any problems caused or lasting symptoms from the TIA whilst you’re on holiday may not be covered by your policy – and you could be left out of pocket should you have to seek medical help on your trip. Get a quote .
Single Trip insurance is for one-off, individual trips and will cover your specified travel dates. This is usually up to 45 days; however, some insurance providers can cover up to 94 days. If you’re not a frequent traveller, single trip cover is a great option and will likely be cheaper than an annual multi-trip cover .
If you travel 2 or more times a year, annual trip cover may very well save you money. The maximum duration of any trip will always be specified and will vary by provider. But don't worry, when you get a quote, we'll ask you what your maximum trip length is and only show you quotes that match!
A pre-existing condition is a diagnosed medical condition that existed before taking out a policy. We'll ask a series of questions about the medical history for you and any travellers on your quote. If you answer yes to any of these, you will need to tell us about the traveller's conditions. This could be a condition that a traveller has now or has had in the past. If you are not sure what conditions you need to declare, we have online support available to help you 24/7!
* Price is based on 1 traveller aged 61, who has declared Stroke and is travelling to France for 7 nights. The price is correct as of July 2024. Prices may vary according to your individual requirements.
Trusted by people just like you
Don't just take our word for it...
If we're unable to help you find cover for a pre-existing medical condition , the Money Helper Directory has listings of companies that may be able to assist you. Further details can be found on their website.
Related Products
Single trip travel insurance.
Compare travel insurance for a specific trip, covering medical conditions and expenses. We'll search our specialist panel and show you prices from over 30 of the UK’s best travel insurance providers.
Annual Multi-Trip Travel Insurance
Taking more than one or two holidays a year? Compare annual multi-trip travel insurance from over 30 specialist insurers and save money whilst having peace of mind whilst you travel.
Travel Insurance for Cruises
If you're taking to the high seas for an adventure, make sure your policy includes specialist cover for cruises. Start your travel insurance comparison today.
Pre-existing Conditions
Save time and money on travel insurance for pre-existing medical conditions. Use our comparison tool to compare medical travel insurance cover.
Winter Sports & Ski Cover
When hitting the slopes, it pays to make sure your travel insurance includes cover for winter sports like skiing or snowboarding.
Check out our articles
Read the latest articles from our blog
We make finding specialist stroke travel insurance simple. Find the most suitable travel insurance provider for you, at the best prices! Compare today!

Sign up to receive regular updates
Get the latest news, advice, travel tips and destination inspiration straight to your inbox.
Oops, did you travel without insurance? We can get you back on track

Mon - Fri 9am - 8pm
Sat 9am - 4pm
Sun 10am - 4pm
- 0800 294 2969
- Single Trip Travel Insurance
- Annual Travel Insurance
- Cruise Travel Insurance
- Family Travel Insurance
- Staycations
- Winter Sports
- Business Travel Insurance
- School Trip Travel Insurance
- All No Upper Age Limit Travel Insurance >
- Car Insurance
- Home Insurance
- Smart Luggage
- Life Insurance
Specialist Travel Insurance with no upper age limit
- Angioplasty
- Atrial Fibrillation
- Cardiomyopathy
- High Blood Pressure
- Multiple Sclerosis
- Breast Cancer
- Skin Cancer
- Lung Cancer
- Prostate Cancer
- Crohn’s Disease
- Back Problems
- Osteoporosis
- Coronavirus
- South Africa
- All Africa Insurance >
- All Asia Insurance >
- The Dominican Republic
- All Caribbean Insurance >
- All Central America Insurance >
- All Europe Insurance >
- Puerto Rico
- All North America Insurance >
- New Zealand
- All Oceania Insurance >
- All South America Insurance >
- Get a Quote
- Airport Hotels & Parking
- Travel Money
- Travel Advice
- Working with Us
- Medical Advice Hub
- Brand Showcase
- Meet The Team
- Careers: Apprenticeship Scheme
- Amend your policy
- Your Questions Answered
- Make A Complaint
- Making a Claim
Travel Insurance for Strokes
Don’t let the fear of a stroke stop you from travelling. your travel insurance has you covered.
Travel can be a concerning prospect if you have had a stroke, and worrying about whether it will happen again is entirely normal. Strokes are a common medical issue for many people in the UK, with reports of a new case every five minutes .
With this in mind, it’s crucial to have a Travel Insurance plan that specifically addresses your needs, especially if you have suffered a stroke in the past or have a medical condition associated with strokes. Our specialised stroke Travel Insurance includes the medical cover you need, designed to give you confidence and peace of mind while you explore the world, ensuring you are well-protected in case of any health emergencies related to a stroke or any other declared medical condition.
Travel Insurance for Stroke Survivors
Our specialist insurers have extensive experience assisting customers in their quest for Travel Insurance that can protect them in the event of a stroke or TIA (mini-stroke) while abroad.
Don’t let the fear of a stroke or TIA stop you from enjoying your well-deserved trip! Getting stroke Travel Insurance that covers you for a stroke, TIA, or a declared medical condition that caused a past stroke, will help you prepare for a medical emergency while you’re on holiday.
Securing Stroke-Specific Travel Insurance: Finding the Right Policy
We aim to make finding Travel Insurance for a stroke or TIA easy by working with a range of insurers which specialise in covering pre-existing medical conditions , including post-stroke. Get a quote online, or if you prefer to speak with someone, contact one of our Travel Insurance specialists, who can help you find Travel Insurance for stroke victims over the phone.
When responding to medical screening questions, try to be as honest and accurate as possible. Once we receive your response, we will be able to scan our market accurately, understand the type of Travel Insurance you need for your pre-existing medical condition, and try to assist you in finding stroke Travel Insurance.
Enjoy Your Holiday with Peace of Mind
Once you have Travel Insurance that covers you for a stroke or TIA, you’re all set to enjoy your holiday. Whether that be lounging at a pool, exploring jungles, or hitting the ski slopes! Just make sure to select winter sports cover or activity pack B as an additional premium if you plan any exciting activities that aren’t included as standard.
Pre-Travel Tips for Stroke Survivors
There are other precautions you can take before travelling as a stroke survivor. Alongside making sure you have stroke Travel Insurance that covers you, we recommend that you speak with your doctor if you are unsure whether you are fit to travel. If you need a specific type of medication, make sure it is easily accessible while travelling. Additionally, getting a note from your GP stating that you need that medication to get through security with no unnecessary delays is a good idea.
Travel Insurance for Stroke FAQs
Frequently asked questions about Travel Insurance for Stroke.
Can I get Travel Insurance after I have had a stroke?
Travel Insurance policies are available for hundreds of pre-existing medical conditions, including strokes or TIA. Finding Travel Insurance that covers your specific situation is essential. Our Travel Insurance specialists are experienced in helping customers who have suffered from a stroke or TIA find stroke Travel Insurance that suits them.
Do I need to declare my stroke on my Travel Insurance?
If you do not declare a stroke or TIA with your insurance company, you could risk your Travel Insurance becoming void if a stroke-related medical issue were to occur while you are away. If you do not declare your stroke, you would not be covered if you had a stroke on holiday, but also anything related, such as a heart attack. To be fully prepared, make sure your Travel Insurance covers stroke or TIA.
Is a stroke a pre-existing condition?
A pre-existing medical condition is any illness or injury you had before taking out your Travel Insurance. If you have suffered from a stroke or TIA, this qualifies as a pre-existing medical condition.
Is Travel Insurance expensive after a stroke?
The average cost of Travel Insurance after a stroke or TIA may increase due to the potentially higher risk of needing to make a claim while travelling. However, it will also depend on your age, other medical history, where you’re going and for how long.
It also depends on how long ago your stroke was. As for full strokes, we will ask you if it was more or less than 3 months ago and how many strokes you have had in the last 6 months, which may affect the price.
Securing stroke Travel Insurance is vital as if something were to happen and you did not have adequate cover, you could end up paying out of pocket. We’ll compare prices from several insurers and offer bronze, silver and gold options on most policies. Secure your peace of mind.
Can you fly after a TIA (Transient Ischemic Attack) or Stroke?
Yes, you can generally fly after experiencing a TIA or stroke, but it’s essential to consult with your GP before making travel plans. The timing of your flight post-stroke or TIA will depend on your overall health, the severity of the episode, and any underlying medical conditions that might have contributed to the TIA. Your doctor will assess your situation and may recommend waiting a period before flying to ensure stability and manage any risks. You must declare these conditions as a pre-existing medical condition when securing Travel Insurance.
Do I need to inform my Travel Insurance company after a TIA?
Yes, you must inform your Travel Insurance company if you’ve had a TIA. Declaring a TIA is crucial because it’s considered a pre-existing medical condition. Not disclosing this information could invalidate your policy, leaving you without cover for any stroke-related medical issues while travelling or if you need to cancel your trip due to your condition. If you have already purchased your Travel Insurance and have suffered a TIA since, have spoken to your doctor and are still planning on travelling, you must update your policy. Informing your insurer allows them to provide a policy that accurately reflects your medical history and ensures you have the appropriate cover, should something happen.
Undiagnosed Medical Condition?
Do you have an undiagnosed medical condition or are you on a waiting list for treatment?
We may still be able to help you find Travel Insurance.
Travel Insurance for Strokes – Your Cover
- Cancellation/ curtailment up to £12,500 (£30,000 on referral)
- Missed departure up to £1,500 per person
- Baggage up to £3,000 per person
- Personal Liability up to £2 million per person
- Zero excess policies available
Medical Cover for Strokes
- Emergency medical expenses and repatriation up to £15 million
- 24/7 emergency medical assistance
- Cover for all types of Autoimmune Conditions
We Compare Prices From These Insurers
Compare Travel Insurance with medical conditions easily with us. We diligently compare various options, helping you find the best Travel Insurance with medical conditions tailored to your needs. Click here to download the Policy Wording and Insurance Product Information document for all insurers. In the event you are unable to find a suitable product from our panel of multiple providers, you can find contact details of some additional Insurers who specialise in travel insurance for people with serious medical conditions here , or call 0800 294 2969 for more information.

How do I know if my passport is valid?
Aug 12, 2024 | Blogs , Europe , FAQs
This blog contains information on travelling to Europe. For more information on travelling to Europe and for insurance, click here The rules around...

What are the new passport fees?
Jul 26, 2024 | Blogs , Europe
What are the new passport fees? As of the 11th of April 2024, the UK passport increased by 7% compared to last year. This announcement came...

10 Must-Sees in Berlin
Jun 18, 2024 | Blogs
If you've been watching Euro 2024 you will have seen Germany in all its glory. Whether you're a history buff, a nature lover or you're simply...
Compare prices in minutes

Copyright © 2023. Just Travel Cover
- Travel Tips Advice
- Compare Travel Insurance
- Pre-Existing Medical Conditions
- Holiday Home Insurance
Customer Services
- Opening Times
Victoria House, Toward Road, Sunderland, SR1 2QF
Call: 0800 294 2969
Monday - Thursday 9am - 6pm, Friday 9am - 5.30pm
Buy with Confidence
Secure Payments
UK Call Centre
Leading Broker
Justtravelcover.com is a trading style of Just Insurance Agents Limited, which is authorised and regulated by the Financial Conduct Authority (FCA) number 610022 for General Insurance Distribution activities. Registered in England. Company No 05399196, Victoria House, Toward Road, Sunderland SR1 2QF. Our services are covered by the Financial Ombudsman Service. If you cannot settle a complaint with us, eligible complainants may be entitled to refer it to the Financial Ombudsman Service for an independent assessment. The FOS Consumer Helpline is on 0800 023 4567 and their address is: Financial Ombudsman Service, Exchange Tower, London E14 9SR. Website: www.financial-ombudsman.org.uk/
Privacy Overview
HelloSafe » Travel Insurance » Medical Travel Insurances » Stroke Patients: Which Travel Insurance?
Stroke: Which Travel Insurance?
verified information
Information verified by Adeline Harmant
Our articles are written by experts in their fields (finance, trading, insurance etc.) whose signatures you will see at the beginning and at the end of each article. They are also systematically reviewed and corrected before each publication, and updated regularly.

Table of Contents
Do you have (or have you had) stroke and would like to get travel insurance for your coming trip in case you face medical expenses abroad?
Travel insurance that covers stroke treatment can be hard to find or very expensive. But you’ve come to the right place.
In this guide, we will explain everything you need to know about stroke travel insurance: is stroke travel insurance compulsory? What specific medical cover should you get if you have or have had stroke? What are the best stroke travel insurance companies and how much will you pay? Let’s dive in!
Why do I need travel insurance if I have (or have had) stroke?
Travel insurance for stroke patients is not compulsory.
However, you should know that your national healthcare cover, your European Health Insurance Card (if you are travelling in Europe), your credit card travel insurance or any other kind of assistance you would have as a country resident or citizen, may not be sufficient to cover any medical expenses you may have abroad.
Some countries may ask for valid proof of travel insurance to deliver visas, whether you have pre-existing medical conditions or not.
Much more than a nice-to-have, travel insurance is one of the highest value-for-money insurance products, especially for people with stroke.
A recent study from Which has shown that in around 10000 UK travellers in 2018, 64% of them have already had medical treatment while travelling abroad. The average spend of medical care abroad is around £1300. But it can be much more.
As a stroke sufferer, you may especially face expenses such as:
Travelling in Europe, what does my European Health Insurance Card cover?
As a current or former stroke sufferer, always remember that while travelling in Europe, your first ally is your EHIC card. Your EHIC card will cover for any treatment you may need abroad, including any treatment linked to a pre-existing stroke.
Remember that your EHIC will only cover you until 31/12/2020, the time of Brexit. Make sure you have both EHIC and travel insurance before travelling. Many insurers will ask you to get your EHIC if travelling in Europe, and would waive the excess if you have a valid card with you.
If you are going to Australia or New Zealand, the UK also has specific healthcare system cooperation programs.
For any specific information on the European Health Insurance Card, check out the NHS website .

Can I easily get travel insurance with or after stroke?
If you have been diagnosed with stroke, whether you are in remission or not, you may find it difficult to find cheap stroke travel insurance that will cover you for your trip without major exclusions.
Getting travel insurance after stroke can indeed be very time-consuming and you could end up paying three or four times the price people without a medical history would pay for a standard cover policy.
Unfortunately, insurers will see you as being at higher risk of making a claim such as:
- Cancelling your trip for reasons due to stroke, such as an important medical appointment being postponed
- Needing expensive medical treatment linked to your stroke while travelling abroad
- Needing repatriation to the UK.
We all agree that this is unfair, especially, for example, if you are in a very stable condition. But don’t worry, some insurers – fortunately – have agreed to cover people at higher risk. You could get travel insurance post stroke either through:
- Companies that will provide you with standard cover as they would do for any other tourist, but may invalidate any claim due to your treated stroke (if you are sure about your recovery and only need cover for a few days trip, for example);
- Or specialised travel insurance for stroke sufferers (or other existing medical conditions).
We are here to help you find the best and cheapest travel insurance after stroke surgery depending on your current medical condition, your age, the length and destination of your trip, etc.
What are the best travel insurance policies for stroke patients?
You will find below a list of specialist travel insurance policies for stroke patients – as well as for those with other pre-existing medical conditions – who will provide you with good cover and dedicated assistance.
All the above insurers are specialists in covering pre-existing medical conditions. Unless it is clearly mentioned in the features, they all use the Verisk screening system and apply a change in health disclosure in their policy which will allow them to inflate premiums and change or cancel your travel insurance policy if an unexpected event related to your healthcare occurs before your trip.
Find out more cheap travel insurance for stroke with our 100% anonymous tool.
Do I need to declare stroke for travel insurance?
You are required by law to declare any pre-existing medical condition when purchasing an insurance policy.
A pre-existing medical condition is typically one for which you have been diagnosed and have received treatment before you apply for any travel insurance policy, regardless of whether this is short- or long-term.
Therefore, stroke counts as a pre-existing medical condition. You are therefore required to declare your stroke to your insurer, whether you are in remission or not.
Good to know
Not disclosing your stroke could invalidate your claim as well as your entire travel insurance policy.
How does stroke screening for travel insurance work?
If you have stroke, or any pre-medical condition, you are more likely to be screened before applying for a policy.
On insurers’ websites, you’ll be asked to answer a set of questions administered most of the time by the Verisk medical screening system before getting quote results. Some insurers may have their own set of questions and may attribute their risk rating based on your answers.
Do you have or have you had stroke? Here is the list of questions you will most probably be asked to answer when purchasing travel insurance covering stroke:
The below list of screening questions is not exhaustive and may vary depending on your specific answer to each of the question.
Those questions are the most common ones you may find on insurer's websites. In the case that there is no screening system on an insurer’s website, you will need to disclose any health condition by contacting your insurer directly.
How much is stroke travel insurance?
Here are some indicative quotes for single trip and annual travel insurance for stroke patients:
* Quotes above are only indicative and for stroke with no recent complications.
It is quite difficult to give precise ranges of how much stroke care travel insurance is. Prices are based on a wide range of criteria and will not only depend on your pre-existing medical condition, but also:
- Your age and destination
- If you’re going for a single or annual multi-trip, as mentioned above
- If you’re subscribing to upgrades such as cruise, business or gadget cover
- The length of your stay abroad
- If you’re travelling alone, with your partner, a group or your family
- The financial limits you’d like to get in case of a claim
- The excess amount you’re willing to pay
- What you will be doing abroad (e.g. winter or extreme sports).
What is usually covered by stroke travel insurance?
Insurers covering a pre-existing medical condition such as stroke often provide a high compensation amount for trip cancellation, medical expenses and repatriation.
Here is a typical list of what you should pay attention to while applying for stroke travel insurance cover:
Besides compensation limits, you should also go for a company including specific healthcare upgrades as standard such as:
- Bespoke medical screening before applying for travel insurance : the possibility to easily talk to someone and find the right cover for your needs (especially for terminal illness)
- UK-based 24/7 assistance helpline while you’re abroad : dedicated free-of-charge landline to get healthcare advice and help in finding the right doctor or hospital abroad, reactive assistance, etc.
If you are about to make a medical claim while you are abroad, we advise you to get your insurer to accept it first and pay upfront. In the case you need to pay up front, always keep receipts and submit your claim as soon as possible.
What is not covered by stroke travel insurance?
That will vary from one insurer to another.
Besides the main exclusions usually found in insurers’ policy booklets (terrorism, strikes, natural disasters, claims related to drug, alcohol, etc.), regarding pre-existing travel insurance, your claim may be invalidated:
- If you are travelling without your doctor’s consent
- If you have been told you have a terminal illness and you have applied for travel insurance without saying so
- If you are waiting for a diagnosis or medical treatment at the time of applying.
Does travel insurance cover terminal stroke?
As said above, most insurers will not cover any terminal illness diagnosed, and therefore won’t cover incurable stroke.
However, we’ve come up with a list of companies still offering cover for people with terminal stroke depending on the length and destination of your trip, the stability of your medical condition and your doctor’s consent:
Most of the time, insurance companies will still ask you a minimum duration between your prognosis and your return travel date. You should also know that no insurer will cover you for your trip against your doctor’s consent.
What if I am diagnosed with stroke after having applied for travel insurance?
When it comes to medical condition travel insurance, insurers often add an ‘ongoing duty of disclosure’.
It basically means that if any important change related to your healthcare occurs after you applied for travel insurance policy, they have the right to either:
- Screen you again;
- Raise your premiums;
- Change your policy contract;
- Cancel your policy.
Most of the time, if your health condition changes, insurers will either:
- Provide you with new travel insurance for your new health condition with an additional fee;
- Provide you the same insurance but the new condition will be excluded;
- Or simply offer no cover, as they consider your condition too risky.
Ask for a pro rata refund or full refund if they cancel or change your policy before you make any claim.
Can you travel abroad with stroke?
The short answer is yes, of course.
However, here are some tips we would advise you to carefully read:
- Get your doctor’s consent and advice before travelling with past or current stroke.
- Get any vaccinations needed.
- Get the right stroke travel insurance for your trip, covering treatment linked to your disease and any medical care you may need abroad, and carefully read your policy booklet (exclusions, limits and deductible amounts, etc.)
- If you are not in remission, be sure that the trip will not be too much effort and not too tiring for your medical condition.
- Remain prudent and take with you your doctor’s phone numbers and local emergency contact details. If possible, travel with someone.
- Make a list of needed medication and keep them in their original packaging (for customs) and store them safely. Prepare back-up meds.
Top 5 tips to get cheaper travel insurance quotes for stroke victims
If you have or ever had stroke, here are some tips you may like to use to lower your insurance premiums:
- Use our comparison table to find out which companies are the best and the cheapest for stroke patients.
- Take your phone and try to speak to humans! If you have someone on the phone, they are more likely to understand your stroke medical situation and find you the appropriate cover.
- Go for single trip cover rather than annual multi-trip . You’ll be seen as a lower risk traveller as you will only need cover for a defined stay.
- Change your destination and opt for European trip rather than a roadtrip across the USA’s legendary Route 66! You’ll be less likely to make a very high medical care claim, which could see your premium go down.
- Benefit from a joint travel policy discount, insuring both your partner or family and yourself.
Alexandre Desoutter has been working as editor-in-chief and head of press relations at HelloSafe since June 2020. A graduate of Sciences Po Grenoble, he worked as a journalist for several years in French media, and continues to collaborate as a as a contributor to several publications. In this sense, his role leads him to carry out steering and support work with all HelloSafe editors and contributors so that the editorial line defined by the company is fully respected. and declined through the texts published daily on our platforms. As such, Alexandre is responsible for implementing and maintaining the strictest journalistic standards within the HelloSafe editorial staff, in order to guarantee the most accurate, up-to-date information on our platforms. and expert as possible. Alexandre has in particular undertaken for two years now the implementation of a system of systematic double-checking of all the articles published within the HelloSafe ecosystem, able to guarantee the highest quality of information.

Freephone our UK Team
0800 072 6778
Sales & Service
Monday to Friday: 8:30am to 8pm Saturday: 9am to 5:30pm Sunday: 10am to 5:00pm
Monday to Friday: 9am to 7pm Saturday: 9am to 5:30pm
Travel Insurance
Medical travel insurance, seniors travel insurance, europe travel insurance, worldwide travel insurance, coronavirus travel insurance, stroke travel insurance.
- Unlimited medical emergency expenses¹
- Up to £10K cancellation cover
- 24/7 emergency medical helpline

Covered 27 million+ travellers
Trusted for 20+ years
24/7 emergency helpline
Travel insurance after a stroke or TIA
We understand that insuring a medical condition can be a bit frustrating, and with around 100,000 people suffering from strokes every year in the UK , we want to make it as easy as possible for you to get travel insurance . So, if you or someone you care for has been affected by a stroke and are concerned about whether travel insurance will be able to cover you and your condition we may be able to help you, even if you’ve had trouble getting covered in the past.
A Transient Ischemic Attack (TIA), also called a mini-stroke, can affect your holiday plans as much as a stroke. Airlines have different policies on how long you should wait to fly after having a TIA or stroke, but most recommend waiting at least 10 days before getting on a plane for a TIA and 21 days if you’ve had a stroke.
Air travel is known to increase the chance of a stroke or pulmonary embolism. If you have an increased chance of suffering a stroke due to high blood pressure , remember to keep moving your legs regularly and wear flight socks on your journey.
One of the things that makes us stand out from the crowd is that we will consider all medical conditions , including strokes and TIAs! Simply contact us or get a quote online to go through our simple medical screening process.
What does stroke travel insurance cover?
If you have had a stroke or TIA, we’ll do our best to offer a policy that’s suited to your needs. Like all our policies, our travel insurance that covers you in the event of a stroke will include some great features as standard, including:
- Holiday cancellation cover
- Belongings and baggage cover
- Passport, money and documents cover
- Delayed departure cover
- Personal accident cover
- Accommodation cover
- Cover for over 50 sports and activities
- Medical and hospital expenses cover (including expenses related to any medical conditions you have declared and have been covered by us)
For more information on what’s covered with travel insurance for strokes and other medical conditions, have a read of our policy documents . If you have any other pre-existing medical conditions don’t worry, we will still consider you!
And if you still can’t find what you’re looking for, why not get in touch with us; we’ll try and help.
Please note: ‘TIA travel insurance’ is a general term for one of our standard travel insurance policies including cover for other health conditions, which is subject to medical screening and may require an additional premium. We don’t offer specialist cover for this specific condition.
*Discount excludes any premium generated to cover medical conditions or optional extras & is automatically applied. This offer cannot be used in conjunction with any other offer. Discount tiers of 5% for premiums between £0-49, 10% for £50-249, & 20% for £250+ apply. Offer ends at 23:59 on 02/09/24. T&Cs apply.
- Unlimited emergency medical expenses available on Black level policies.
- InsureandGo’s Gold achieved a Which? Best Buy.

- Home Medical Travel Advice Travelling After a Stroke
Travelling After a Stroke
Travel insurance | medication | destination, when to travel after a stroke.
Life after a stroke can be a struggle but people want to try and get back to their normal routine as soon as possible, part of which can be heading abroad on holiday for some much-needed relaxation.
However, buying travel insurance for your holiday after a mini or major stroke can be difficult – but it doesn’t have to be; we have put together everything you need to know about planning a post-stroke holiday and how to find the right travel insurance, that doesn’t cost the earth.
There is no set timeframe to travelling after a stroke as this will depend solely on both the severity and implications of the stroke. Generally, patients are advised not to travel within ten days of suffering a Transient Ischaemic Attack (Mini Stroke), but this can extend to three months or more following a Cerebrovascular Accident (Major Stroke). In all cases, you should consult your doctor about your travel plans before booking your holiday.
It is essential to not travel by air too soon after a stroke as it can be dangerous. When in flight there is less oxygen and it can be taxing on people who have a stroke, heart condition or respiratory condition.
You may be prescribed medication following your stroke, so ensure this is legal in the country you are travelling to as some medication which are prescribed in the UK are banned in other countries. Follow the medication link to read more on taking your medication abroad.

HOW A STROKE CAN AFFECT YOUR TRAVEL PLANS
Following a stroke, you may be left with reduced mobility, speech or sight impairments which could make travelling more difficult, but doesn’t mean you can’t travel. Provided your GP has confirmed it is safe for you to travel you can speak to your transport provider and ask for assistance to be arranged. Airlines, cruise ships and rail companies all offer these services, but they do have to be booked prior to your trip.
You may also be at higher risk of a DVT (deep vein thrombosis/blood clot). Whichever mode of transport you choose it is advisable to wear flight socks if you are going to be seated for long periods of time, and if possible, carry out small exercises in your seat to keep the blood moving. Drinking fluids to avoid becoming dehydrated will also help with blood flow.
Some destinations may be less practical after a stroke, so this will be something to consider when booking your holiday. Make sure the accommodation has the access you require and try to keep everything within walking distance so you don’t exert yourself too much. Depending on how soon after your stroke you are travelling, it is a good idea to consider the activities you will be undertaking and make sure you set a suitable itinerary. Run your plans past your GP first before booking them.
TRAVELLING AFTER A STROKE CHECKLIST
- Check that your doctor is happy for you to travel to your chosen destination and that your itinerary isn’t going to be too much too soon.
- Spend some time research travel insurance companies. There are medical specialists out there, quote prices and cover will vary between them so make sure you buy one that is suitable for your needs.
- Whilst we’re talking about travel insurance, make sure you check the medical excess. This will be applied against your declared medical condition and will only need to be paid if a claim is submitted related to the condition.
- Make sure you pack enough medication to allow for delays. Sometimes transport delays can be over 24 hours so you will need to ensure you have enough medication to allow for this.
- If you are taking medication abroad, speak to your GP and ask for a note confirming your condition, that you are fit to fly and the names of the medication you are taking.
- Once you have chosen your destination spend some time researching where the nearest public hospital and pharmacy is – just in case.
- Before you travel make a note of the policy reference number and travel insurance emergency contact number. It is also a good idea to leave these details with either the hotel or someone back home.
MORE ADVICE FOR TRAVELLING AFTER A STROKE
Before you go
Here are some more articles you might like:

Become an expert in all things travel with our monthly newsletter…
- About Stroke4Carers
- How to use this site
6) Holidays
Holidays should be enjoyable for everyone. When someone has had a stroke you may need to do more forward planning to ensure the trip goes smoothly from start to finish. Any extra planning will depend on how the stroke has affected the person. If they have to use a wheelchair for all or part of the journey, how often they will need a break, do they need to take other equipment or hire additional equipment at the destination. If it is a trip for a day, a weekend or a longer holiday here are some tips when planning and going on holiday.
Tips when planning and going on holiday
- Check facilities when you book . There are travel operators who specialise in holidays for people with disability. The more complex the person’s needs are the more carefully you need to check the facilities at the destination and on the journey.
- Take a note of the person’s medical conditions . If the person does become ill during the holiday you will have information to hand which will help the doctor in the place you are visiting.
- Ensure your vaccinations are up to date This includes the flu vaccination. Take any certificates with you.
- Check the accommodation thoroughly . Some hotel or brochure descriptions of “disabled access or facilities “may not be exactly what you are looking for. Bathrooms in particular can be very variable. Call the accommodation directly and speak to the manager or person in charge and explain what the person needs in terms of space, facilities and equipment. A travel agent or booking clerk will not know what you need.
- Bear in mind that most aircraft have poor access in toilets . Space is very restricted and no room if the person needs assistance. Consider the length of the flight and how long the person can realistically go without a bathroom break.
- Check access for electric powered scooters . Most train operators do not have access for electric powered scooters in passenger carriages.
- If you can - book assistance in advance . This will give you extra help at rail stations, airports or ferry crossings. Remember you will have to book assistance at each stage of the journey for example if you have to change trains.
- Electrical equipment check you have the correct adaptors for your destination.
- Take all your medication in your suitcases . If your luggage is delayed or goes missing you may have difficulty and expense getting replacements .Keep medications in your hand bag or carry on bag. For people who are also diabetic, it is possible to take insulin and needles on board aircraft if you have a doctor’s letter and put them in a separate bag. Some airlines will put your insulin in a cool fridge for the duration of the flight. Check in advance of travel.
- Take as many “home comforts” as you can . Take only what you need. If the person needs help to walk or use a wheelchair, who ever is assisting cannot also pull suitcases or carry bags. Clever packing also helps. Take only what you need and clothes which can be easily washed and dried without looking too creased.
- You don’t need travel or medical insurance . This could be an expensive mistake especially if you are travelling abroad. It may be wise to take out travel insurance even if you are travelling in the UK if you have to take expensive items of equipment with you, a wheelchair for example.If you have to cancel a holiday due to illness some insurance policies will refund the costs. Check with your policy
View Text Alternative
- If you can – book assistance in advance . This will give you extra help at rail stations, airports or ferry crossings. Remember you will have to book assistance at each stage of the journey for example if you have to change trains.
- Take all your medication in your suitcases . If your luggage is delayed or goes missing you may have difficulty and expense getting replacements. Keep medications in your hand bag or carry on bag. For people who are also diabetic, it is possible to take insulin and needles on board aircraft if you have a doctor’s letter and put them in a separate bag. Some airlines will put your insulin in a cool fridge for the duration of the flight. Check in advance of travel.
See Topic 3 Practical advice and tips for carers – Driving and transport alternatives/Transport for wheelchair users on this website.
Travel Insurance
Does anyone know a travel insurer specialising in people who have had a TIA or stroke?
Hi @PeterTS and welcome to the forum.
Travel insurance has come up before & you’ll fibd some recommendations at these links
Annual travel insurance
Travel insurance recommendations, please
As a starting point though I have used LV & RIAS. Stroke Association work with All Clear
And Different Stroke use medical travel compared.
Hope this helps.
Hi and welcome to this forum. I have always used a comparison website when travelling abroad. That way you can get the cover suitable for you, at a price you can afford. I would advise that you declare your medical history when looking for cover.
Good luck, hope that’s helpful.
Regards Sue
Thank you both. The quotes I’ve had to date - after a single event TIA in April from a variety of sources all seem very high!
I’m not sure how much you’ve been quoted but for me and hubby going to Europe last year it cost over £200 single trip. I have a few medical conditions and so does hubby so that will increase costs. Maybe it’s because it isn’t a year since your event but not sure how it works. Definitely try a comparison site but make sure it covers your medical conditions.
Thank you. I have been quoted £600 for a week’s river cruise in France and £800 for a river cruise in Portugal & Spain. Non-river cruise isn’t much different. I have other health issues but a weeks’ cover before my TIA was £250.
Hi @PeterTS - that does seem very high but like others, I’m not sure how it’s worked out. Like @Mrs5K said, maybe it’s because your TIA was recent? My stroke was five years ago and my last annual policy cost just over £400, including the US but excluding cruises.
I always use a comparison site and swap provider if I can get a better deal. As already said, it’s crucial to disclose all medical conditions.
Best wishes.
@PeterTS that does seem high. You’re not awaiting any medical tests or procedures are you? That can affect cover. Maybe it’s because it’s cruising and the cost of getting someone off a ship? Definitely shop around. Another site to try is payingtoomuch.com
I’ve heard of people using staysure, insure and go as well.
Not sure if I can mention this or not but if you are looking for insurance of any kind or any online shopping, I often use Quidco. They get a commission from the sites your query is directed to and they pass that onto you for a small annual fee. Topcashback is another similar site. You shouldn’t pay any more using the link and it can over time save you a very decent amount. I do not benefit in anyway if you use the site, I am simply passing this on as it saves me money. I am a customer of the site only. Screenshot of current cashback rates below.
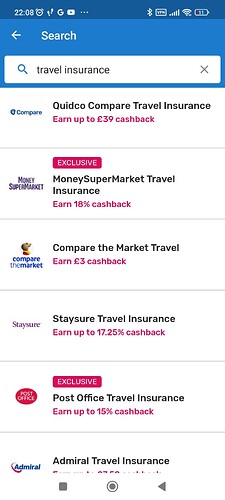
@SimonInEdinburgh This could be an example of how the SA could generate additional income, there are various versions of this that clubs use.
Here’s one for a football club
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Health and social care
- Infected Blood Inquiry Response Expert Group Reports
- Infected Blood Compensation Authority
Infected Blood Inquiry Response Expert Group Final Report
Updated 16 August 2024

© Crown copyright 2024
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/infected-blood-inquiry-response-expert-group-summary-report/infected-blood-inquiry-response-expert-group-final-report
Foreword by the Minister for the Cabinet Office
I am very grateful for the specialist advice provided by the Infected Blood Inquiry Response Expert Group, offering specialist expertise to ensure the Compensation Scheme can serve the victims of infected blood. In particular, I would like to thank the chair Professor Sir Jonathan Montgomery for his clear direction of the group and willingness to facilitate the provision of wide-ranging advice.
An interim summary of the Infected Blood Inquiry Response Expert Group’s work was published on gov.uk on 21 May 2024. Since the publication of the interim report, the Interim Chair of the Infected Blood Compensation Authority - Sir Robert Francis KC - has conducted an engagement exercise with representatives of the infected blood community to gather feedback on the proposed scheme before it is finalised in regulations.
In his recommendations, Sir Robert recommended the Expert Group to provide further detail on the rationale underpinning their advice. He also asked them to review clinical and legal practicalities for a number of areas of the proposed scheme in light of the engagement exercise outcome. The final report includes the reviewed areas of work recommended by Sir Robert.
I hope that the report provides reassurance surrounding the decisions taken in the Compensation Scheme. The Government is committed to providing fair and full compensation to victims of infected blood, and work of the Expert Group has played a critical part in delivering this.
Rt Hon Nick Thomas-Symonds MP, Minister for the Cabinet Office
Acknowledgements & Thanks
From the Expert Group Chair, Professor Sir Jonathan Montgomery
I am extremely grateful to my colleagues on the Expert Group, and to the civil servants who have supported us, for their commitment during the intense period that is covered in this report of our work in providing advice to Ministers. Each has brought distinctive professional expertise to our deliberations. They have worked together with mutual respect and compassion for those who are entitled to justice under the compensation scheme recommended by Sir Brian Langstaff in his Second Interim Report. We have aimed to provide robust and objective advice on technical aspects of the design of the scheme. We have been acutely aware that justice demands fair compensation and that the very long delays that victims have already suffered mean that it must now be delivered as soon as is practicable. We hope that our advice will assist the Government in that task.
Our terms of reference did not permit us to take evidence directly from members of the infected community. We have done our best to take note of evidence received by the Inquiry and we have drawn on members’ insights from their professional work. Had time and the restrictions of confidentiality permitted wider consultation, then we would have found that helpful. The Government decided to tender for legal expertise from a single firm rather than to invite representatives from a number of different lawyers. This has precluded the collaborative approaches that solicitors aim to adopt. I have been deeply impressed by the care taken by all those involved to consider not just their own judgements but also the range of views they know others might suggest.
We have benefited from feedback from the Engagement Events that were convened by Sir Robert Francis KC in his capacity as Interim Chair of the Infected Blood Compensation Authority. The Expert Group is grateful to him for allowing me to attend those meetings and convey the insights to the Expert Group to refine its advice. Many very helpful and constructive points were made that needed to be taken into account.
Membership of the group is set out in Annex A
Executive Summary
The moral case for compensation for the victims of the infected blood scandal is compelling. The impact of the wrongful infection on their lives is substantial and far-reaching. They have been let down by the NHS, in whose care they trusted. Information to which they were entitled has been withheld or lost, both by the health service and Government. They have suffered terrible stigma when they deserved support. Justice has been long delayed. Issues about research misconduct have been identified more strongly in the final report than we anticipated and we have added some observations on the implications for the compensation scheme to our initial advice.
In his Second Interim Report, Sir Brian Langstaff set clear expectations for the scope and shape of the compensation scheme that described who should be eligible and the categories of loss that should be reflected in the awards. He recommended that it should be based on a tariff approach and that it should be characterised by speed of provision, simplicity of process, accessibility, fairness and efficiency. Sir Brian also recommended that proactive support would be needed for people claiming the compensation to which they are entitled.
It will be for His Majesty’s Government to determine the details of the final scheme, through the Regulations that will be laid before Parliament within three months of the Royal Assent to the Victims and Prisoners Bill. Our task has been to advise on how Sir Brian’s recommendations could be implemented. In particular, we have been asked to ensure that compensation should be deliverable rapidly; that the scheme would be worthy of the trust of the communities which have been infected (and also affected), so that they would prefer it to litigation through the courts; that there should be a simple and sensitive application process (that avoids re-traumatisation), that requires of applicants minimal time, effort or stress. Sir Brian recommended that the development of the scheme should involve the infected community. We support that principle, but our terms of reference precluded public engagement in our work. We have revised our initial advice in a number of respects based on the feedback from the Engagement events convened by Sir Robert Francis KC as Interim Chair of the Infected Blood Compensation Authority..
Sir Brian recommended that the compensation scheme should provide for awards based on five components and that their quantification should reflect different impacts on people who were infected and on those who were close to them (described by Sir Brian as ‘affected’) and also take into account differences between the diseases caused by HIV (human immunodeficiency virus), HCV (Hepatitis C virus) and HBV (Hepatitis B virus) and the impact of co-infections. Sir Brian explained that the components of compensation need to address
- The Injury suffered
- The Social Impact of that injury
- The interference with people’s Autonomy
- The additional Care costs that people incurred as a result of the injury, and
- The Financial Loss that was suffered from being unable to work
Awards for people who were wrongfully infected
Sir Brian recommended, building on the Compensation Study undertaken by Sir Robert Francis, that the scheme should reflect the different impacts of infection by developing severity bandings but did not define them. The clinical members of the Expert Group have proposed the following bandings, beginning with those who have experienced the most significant impacts
- People who have been co-infected with HIV and/or HCV and/or HBV
- People who have been infected with HIV
- People who have been infected with HCV or HBV who have progressed to liver cancer, decompensated cirrhosis and/or those who have needed to receive a liver transplant,
- People who have been infected with HCV or HBV who have progressed to cirrhosis
- People whose HCV and HBV infection is chronic (lasts more than 6 months) but has not progressed to cirrhosis
- People who have been acutely infected with HCV (but did not develop chronic infection)
- People who died or received a liver transplant because of an acute HBV infection
- These bandings are based on clinical markers. The Expert Group considered that it was important to ensure that the evidence required from people claiming their right to compensation should be readily available to them, be verifiable in order to enable objective assessment of their entitlement, be proportionate to the need to operate the scheme and that inappropriate intrusive questions should be avoided.
For people who have been infected, this enables an injury award for each band to be calculated by reference to judicial guidelines on the damages that are appropriate in personal injury cases. This has been done by taking the descriptions developed by clinicians of the symptoms that are typical of people with these diagnoses and examining case law and judicial guidelines for comparable cases. These injury awards would be uplifted where people suffered more than one infection as the clinical advice is that co-infections are significantly more harmful.
Following the Engagement Events, we reflected on the feedback that insufficient recognition was given to the impact that some victims experienced. We revised our advice to add six supplementary health impact groups where adjustments would be made for additional care needs or financial loss. These cover
- Severe visual impairment
- Neurological disorders which result in long term severe physical/mobility disability
- Neurological disorders which result in long term severe neurocognitive impairment
- Severe psychiatric disorders
- Other Hepatitis C associated extra hepatic disorders resulting in long term severe disability (including those on current support scheme enhanced payments)
- End stage kidney disease requiring renal replacement therapy
The Expert Group believes that social impact awards should not differ as much across the bandings as injury awards because the stigma suffered is usually as a result of societal prejudice rather than knowledge of the clinical symptoms or specific infection. We recommend that there is a flat rate for most beneficiaries that is fixed at the upper end of the band suggested in the report from Sir Robert Francis. This would be reduced for those in the HCV acute band, as they most likely will not have been aware of their infection and the likelihood of stigma is reduced, and increased for those who were infected by more than one virus as the impact is likely to have been more obvious and there was therefore a greater risk of stigma.
There are limited comparators for the autonomy awards that Sir Brian Langstaff recommends as a new head of loss. They need to reflect the aggravated distress caused by interferences in people’s autonomy and private life such as lack of informed consent, lack of sufficient information about the risks of treatment, and about diagnosis, treatment and testing, or being the subject of research without their informed consent. Awards should also include the effects of lack of candour and inadequate responses by authority. These may not have all applied to every victim but they will all have experienced a lack of respect for their autonomy in some of these ways. The Expert Group has found elements of the Windrush Compensation Scheme to be the most useful guide to the quantification of this category of award, although it is not a direct comparator.
Care awards aim to compensate for the cost of care that has been received, or its value if it has been given without charge. The clinical experts have set out a typical pattern of care needs after infection in the different clinical bands. Where the wrongful infection was likely to have caused death (or is likely to do so for those still living with the infection), then it would be expected that these awards need to cover a period of end-of-life care, some months of high care, and some years of moderate care, with (for those who survive longer) periods with clearly defined lower care needs. These patterns are typically different for those with HIV from those with Hepatitis alone. People with decompensated cirrhosis or liver cancer will typically face greater care needs for longer periods than those with cirrhosis or chronic infections. These care needs have been costed by experts who are experienced in commissioning and delivering care to severely injured people as well as costing care regimes, both in practice and for the purposes of legal cases. This approach means that once the date and nature of the infection and the clinical banding is known, a formula can be used to calculate the award due for a typical pattern of care needs. This can be paid without the need for further evidence, thereby reducing delay. Where people’s care needs have exceeded the typical pattern, additional payments could be made to cover the actual costs after assessment by the Infected Blood Compensation Authority. Care Awards should be paid to the estates of those infected persons who are deceased to cover the cost of care between the date of infection and death. For those living with wrongful infections a choice should be available between a lump sum to cover the anticipated costs over their expected years of life or periodical payments.
Sir Robert Francis suggested that the calculation of financial loss awards should provide people who were wrongfully infected with compensation based on the assumption that they would have earned 5% more than an average salary if they had not been infected. The Expert Group recommends a formula based on this approach that also takes into account that the impact on a person’s ability to work will vary over time. There will be stages in a person’s life where they cannot work at all because of their infection. At other times, possibly for a long period, their ability to do work will be impaired. The clinical experts have estimated the degree of impairment, taking into account that this would have sometimes been greater prior to improvements in available treatment than it would be in the present day. We have revised our advice based on feedback from the Engagement Events to limit the assumption that victims of the infected blood scandal would have experienced the benefits of improvements in treatment.
Many people who have been wrongfully infected will have the length of their working life reduced and this is a loss that must be compensated. The Expert Group proposes that for those who are deceased, awards should include compensation for earnings lost until retirement age based on annual earnings plus 5% and for financial loss between their retirement and their death at half that rate (as would be typical for defined benefit retirement schemes). Compensation for financial losses up to the date of death would be paid to the estate of the deceased. Where there are dependants of the deceased, they should receive further compensation related to lost earnings between death and the date when the death of the deceased might have been expected in the absence of the wrongful infection. This should be paid directly to the dependants. For those living with wrongful infections a choice should be available between a lump sum to cover the anticipated financial loss during the remaining expected years of life or periodical payments.
Awards for people affected by the wrongful infections of others
Sir Brian Langstaff was clear that awards to people who were affected by the infections of those close to them should be made on the basis that they are entitled to compensation in their own right. The Expert Group considers that this means that the awards should primarily reflect the relationship between the person affected and the person infected rather than which virus or viruses were involved.
We recommend that injury awards should reflect the quantum of damages that would be ordered by courts in respect of psychological damage, distress, anxiety and emotional upset that are likely to have been caused. No specific or additional evidence of such impacts should be required beyond establishing the relationship of the person who is affected to the infected person. The scale for injury awards should vary according to the closeness of the relationship, with the largest awards for partners, reducing for parents who have lost children, then children who have lost parents, with others getting a lower rate. For immediate family members, where the law provides for loss of society or bereavement awards, then this should lead to an increase in injury awards in cases where the infection was likely to have contributed to an early death (cirrhosis, decompensated cirrhosis, liver cancer and HIV).
The Expert Group advises that there should be a flat rate of social impact award as all those close to people who are infected will have been affected by societal stigma without variation by virus, disease condition or relationship. As Sir Robert Francis noted, awards under this head should be proportionate to those made to people who were infected as it would be inappropriate for those affected to receive more than they did. The recommendation is that the Social Impact award for affected persons should therefore be a proportion of the award for persons with chronic infections.
It is recommended that autonomy awards for those affected by another’s wrongful infection broadly reflect court awards for the intrusion into privacy. These awards should be made to the partners, parents and children of the infected person. For partners, it is recommended that a comparator of judicial awards for very serious intrusions is adopted. For parents and children, it is recommended that the benchmark should be the mid-point of awards that have been made as aggravated damages in privacy cases.
The Expert Group advises that care costs should be part of the awards to infected persons rather than those who are affected. These costs are related to the services required by the person who is infected. They are calculated by reference to their needs and paid directly to them (or if they have died to their estates). It will be for the infected person or those administering the estate of the deceased to choose how to divide the funds between those who provided the care in order to provide fair recompense. It would not be appropriate for the compensation scheme to take away the control from the infected person. There would therefore not be separate care awards for those who are affected by the wrongful infection of others. Rather, the costs incurred by them, and which Sir Brian Langstaff recognises must be met by the compensation scheme, would be reflected in the care awards for the persons who are infected. The Compensation Authority could be asked by beneficiaries to pay awards directly to others on their behalf.
Financial loss awards should be paid to dependants of an eligible deceased person in order to compensate for the support that they will have lost due to the death. These should reflect the deceased’s lost earnings between the actual and expected date of death, discounted by 25% to recognise that some of those earnings would have been spent by the deceased person on their own account. As noted above, compensation for financial losses up to the date of death would have been paid to the estate.
The Expert Group notes that for most people an acute HCV infection was without enduring consequences (that is it was not in the ‘chronic’ severity band) and was often not identified at the time. This means that there would have been very limited impact on those around the person who was acutely infected. It therefore recommends that no awards should be payable to those affected by a person who was acutely but not chronically infected. The Expert Group recognises that some people have developed significant post-viral symptoms following infection and such individuals and their partners may choose to present evidence of impact to the Infected Blood Compensation Authority and seek a further supplementary award.
Clarifications of eligibility criteria
Sir Brian Langstaff set out the eligibility categories for the new compensation scheme. The Expert Group has advised on clarifications required to ensure that in practice the scheme will operate in accordance with the principles that have been set out above.
All those registered with current or previous support schemes will be eligible. Some further information may be requested to enable the calculation of their compensation but not to assess whether or not they are eligible. The Expert Group has identified relevant clinical parameters that should be recorded in medical records that show disease progression. It has also identified imaging and biopsy results that can be used to assess severity banding.
For those persons infected but not previously accepted on to a scheme, evidence of infection and receipt of a contaminated product will be needed. The Expert Group has identified relevant clinical markers of infection that ought to be documented in and accessible from medical records. The Expert Group recommends that mention of HIV, HCV and HBV on a death certificate should suffice as evidence of infection (although its absence would not be taken to exclude it). Further clarification and examples might emerge as the compensation scheme becomes operational. Where there is an absence of clear medical records of receipt of a contaminated product, the Expert Group recommends that the likelihood of receipt of a blood product could be inferred, for example from major surgical procedures, even if it is not specifically recorded in notes. Patient and Carer narratives similar to those used by the different National Infected Blood Support Schemes could be considered. The Expert Group confirms the finding of Sir Brian Langstaff that there should be no rigid cut-off that precludes claims in relation to receipt of products after any specific dates. However, this may make the causal link between their receipt and the infection unlikely and require further inquiry.
Persons who are ‘affected’ become eligible under Sir Brian’s recommendations because of their connection with a person who was eligible for compensation due to their wrongful infection. The Expert Group has recommended definitions of partner, parent, child, sibling to reflect the range of family relationships as well as formal legal status. It suggests that where eligibility is based on having provided care the threshold should be the same as that used for the ‘low’ banding of provision that is used to calculate the care awards made to persons who are infected. This marks a difference between occasional support and regular care. The Expert Group has not been able to identify ways to make workable the category of affected individuals who were ‘so close that it could reasonably be expected that their mental or physical health would be seriously affected by the consequences of the disease, and who have suffered emotionally, mentally and/or physically as a result’.
The Expert Group believes that the approach set out in its advice will enable the Infected Blood Compensation Authority to calculate the awards to which people would be entitled under Sir Brian Langstaff’s recommendations promptly and without disproportionate requests for complex or inaccessible evidence.
The Moral Case for Compensation
The moral case for compensation for the victims of the infected blood scandal is compelling.
The demands that justice makes arise from particularly cruel circumstances, in which there is more than a specific injury because whole lives have been ruined. The impacts are often lifelong and they permeate all aspects of life. This applies not just to infected persons but also to those around them. The impact of infection has often led to the denial of financial security usually available to citizens such as insurance, pensions, and mortgages. Societal stigma attached to infections has further exacerbated this suffering. The moral case is based on the cumulative effect of a number of grounds that make the call for justice exceptional, possibly uniquely so. Not every victim would be able to prove in legal proceedings that they have suffered each of these injustices but the absence of formal proof of injustice is not proof that they have been treated fairly. The scheme should avoid penalising people for lack of specific evidence when the case for compensation is so overwhelming. Records of treatments that should have been maintained are too often no longer available as the NHS failed to maintain the integrity of patients’ records so that documents were destroyed or lost.
The injustices have been compounded by the fact that many of those infected have not been fully informed about the risks of treatment or always told about their diagnoses. The general failure to respect patients’ autonomy sometimes led to further wrongs; patients being denied care/treatment because their health condition was not acknowledged, being denied the chance to manage risks of infection to others, or the chance to make informed choices about family life. The Expert Group has offered advice on the basis that the NHS has failed in its ethical responsibilities to all victims, making it unnecessary and inappropriate to separate out elements of these wrongs. It also considers that it is inappropriate to make fine distinctions when successive Governments have falsely represented that no wrong had been done to victims, falsely asserted that the treatment they received had in fact been the best available, and failed to secure the relevant paperwork to enable the history to be understood.
Principles Underpinning the Scheme
In this section, we set out the principles that we used to guide our work. These were set by Sir Brian Langstaff, the Government in the work programme that it gave us, and through our discussion of the challenges to be addressed.
Sir Brian Langstaff’s Second Interim Report
In his Second Interim Report, Sir Brian Langstaff set clear expectations for the scope and shape of the compensation scheme that described who should be eligible and the categories of loss that should be reflected in the awards. We have aimed at all times to follow that structure and advise on how it can effectively be implemented. We have used the recommendations as our starting point and used the text of his report to guide our understanding of the rationale behind them. We have also used the Compensation Study to help that understanding, while noting that the Second Interim Report sometimes diverged from the suggestions that it made. We have also relied upon its rich details on options for consideration that go beyond the specific recommendations and assisted us in developing details in a way that was consistent with the underlying principles.
Sir Brian recommended that the Scheme should be based on a tariff approach at least for injury, social impact and autonomy awards. We have sought to extend that approach into care and financial loss awards so that the key objectives that he set can be achieved. These were that the compensation scheme should be characterised by speed of provision, simplicity of process, accessibility, fairness and efficiency.
One of the principles that Sir Brian Langstaff recommended should underpin the scheme was community involvement. The engagement events convened by Sir Robert Francis provided us with important feedback that we have taken into account to revise some of our advice. We would have benefited from such feedback at an earlier stage. However, our terms of reference did not enable us to take direct evidence.
Sir Brian made a number of additional and important points of principle in Recommendation 14 about how the scheme would operate in practice, once the design was agreed by the Government. These include that proactive support would be needed for people claiming the compensation to which they are entitled, and that the Compensation Authority would have access to the records of previous support schemes. We agree that this will be very important. For the purpose of our work, we have assumed that it will be available.
Government aspirations
As part of our induction, the Expert Group was informed of the Government’s intention to agree a Scheme with a number of features, which were consistent with the desire to implement the recommendations in the Second Interim Report. The first was compensation should be deliverable rapidly. Second, it must be trusted by the community and preferred by those seeking redress to court actions. Third, minimal time, effort and stress should be required for eligible parties to participate in the scheme. In particular, there should be a simple and sensitive application process (with the risk of re-traumatisation recognised and avoided). Applicants should automatically be eligible if already a member of a previous scheme. Advice and support should be available for applicants not already registered on scheme.
Reflection on past schemes
As we began our work, we discussed what we could learn from the difficulties that had been experienced by beneficiaries of previous schemes. We could not take direct evidence on this but we were able to note issues that were recorded in evidence to the Inquiry, noted by the All Party Parliamentary Group, chronicled by reporters, or known by expert members from those they look after or worked with. We identified the following additional principles
First, compensation must become a matter of entitlement rather than charity. The APPG had described previous schemes as requiring the ‘worst form of modern-day begging’. To avoid this, we think discretion should be kept to a minimum. Where discretionary judgements are required, these should relate to specific components of assessment not total amounts, reasons should be recorded for such the exercise of such discretion so that challenge/appeal can be made when errors or unreasonable judgements have been made. We also noted that subsequent good fortune does not negate entitlement to compensation for past wrongs, noting that it was reported that the MacFarlane Trust had used this as a reason for declining support.
Second, entitlements must be secure and not ad hoc. The past use of loans, sometimes with equity in houses being taken, had created unacceptable vulnerability. The aim should be to resolve claims fairly once and not to require multiple applications based on extreme need.
Third, the process must not be demeaning for applicants and intrusive inquiries should be avoided (such as asking about sexual relationships to exclude other possible sources of infection).
This led us to identify some principles governing evidence requirements that we have used to guide the eligibility descriptions. Any evidence required should be:
- Accessible to claimants (and assessors) so that we ask for information that we can reasonably expect to be available;
- Assessable so that the relevant question about eligibility can be answered
- Verifiable, so the integrity of the scheme is maintained;
- Privacy is maintained but applicants can be asked to consent to access to medical records; and
- Excessive detail is not sought as it is unnecessarily time consuming (leading to delay and expense in processing cases).
The Task of the Expert Group
It is for His Majesty’s Government to determine the details of the final scheme, through the Regulations that will be laid before Parliament within three months of the Royal Assent to the Victims and Prisoners Act. Our task has been to advise Ministers and civil servants in the Cabinet Office on how Sir Brian’s recommendations could be implemented. Our independent advice on the work that has been done by the Government on its proposals is set out in this report, which elaborates and develops the earlier Summary Report.
We were not asked to make recommendations on the architecture of the Scheme. That had already been done by Sir Brian Langstaff. He, and Sir Robert Francis, had recommended that two panels, one clinical and one legal, be set up to develop that architecture further. We have worked as a single group rather than separating the tasks. This has been very helpful in bringing together the insights of the various experts rather than working in parallel. We have understood that our role was to take on the tasks that were suggested for those panels as well as to respond to any other requests for support in developing the details of the scheme. It has not been our role to make recommendations for changes to the fundamental design, which would be a policy matter for the Government. We have provided advice on the technicalities of implementation.
Sir Brian recommended that the development of the scheme should involve the infected community. We support that principle, but our terms of reference have precluded public engagement in our work. The speed with which we have needed to work in order to meet the Government’s schedule and later statutory deadlines has made this task particularly challenging. We hoped that our advice could be validated by wider discussion before the Regulations were drafted. We have not been able to do this directly, but we have been briefed on issues that have been raised during the engagement meetings convened by Sir Robert Francis as interim chair of the Infected Blood Compensation Authority and have revised our advice to reflect the feedback on matters that are within the scope of our Terms of Reference.
How we worked
The Expert Group met virtually and held over 30 plenary meetings between the beginning of February and the end of July 2024. Additional meetings were convened on specific issues that involved relevant members of the Expert Group. These included defining clinical parameters and giving advice to the Communications team within the Cabinet Office on appropriate terminology. Other sessions addressed actuarial considerations such as expected lifetimes, consistency with the Ogden tables used to calculate awards in personal injury litigation, the fair design of periodical payments. In addition, there were discussions with modellers to assist their understanding of the number of people likely to fall within severity bands.
We began by reviewing the Interim Reports of the Inquiry and the Compensation Study by Sir Robert Francis. We were briefed on the extensive work that had already been done by civil servants on the implementation of the recommendations. This had identified a series of questions on which advice was sought to progress the detailed design. These provided the initial agenda for our work.
The Chair also met with Sir Robert Francis to clarify the Group’s understanding of some of the issues his report examined and with Professor Christopher Hodges, chair of the Horizon Compensation Advisory Board to understand learning from the Post Office scandal.
In order to address questions about eligibility we were provided with documentation on the operation of existing support schemes, and had the opportunity to discuss issues they raised for us with assessors and administrators from the England Infected Blood Support Scheme (some of whom also worked with the Scotland Scheme). We were grateful for the opportunity to explore some issues of evidence and prevalence with experts from the Advisory Committee on the Safety of Blood, Tissues and Organs (SABTO) that helped us appreciate what material was available and accessible. Social Care issues were explored in separate virtual workshops with the social care experts which some clinical members as well as the chair attended.
Our advice informed and helped to shape the proposals that Ministers agreed and which were published by the Government on 21 May 2024. Once the process of drafting the Regulations began, we responded to a series of requests from the drafters for clarification and specification that they needed.
Building on the Architecture of the Second Interim Report
The first stage in developing the detailed framework of the Compensation Scheme was to specify the severity bandings that had been proposed by both the Second Interim Report and the Compensation Study. The clinicians developed these by reference to disease impact and clinical markers that should be available and accessible in health records, in accordance with the principles of evidence that we adopted (see above). They were then asked to provide summary descriptions of the impact of each of these bands on the people who were infected, which were used by the legal experts to identify comparators in case law, judicial council guidelines on compensation tariffs, and from the Compensation Study. This was an interactive process in which further clarification was requested by lawyers of the clinicians in order to refine the range of likely court awards, and in which clinicians probed the basis of the legal advice to avoid misunderstandings. This process led to the quantification of the injury awards.
We then sought to understand how care and financial loss awards could be quantified from the descriptions of the impact of different viruses and severity of impact. This led to a description of the likely care needs for each of the bands, which was refined in discussion with the care experts. The care experts then identified the care provision that would be needed to meet those needs drawing on their experience in commissioning and delivering care to severely injured people. The patterns of care provision were then costed in the way the experts would have done if commissioning the care or assisting in the preparation of litigation. We have been able through this process to devise a way of calculating the value of care awards that does not require specific evidence from beneficiaries beyond that needed to ascertain the appropriate severity banding.
For financial loss awards, we similarly sought to develop an approach that would not require detailed evidence from beneficiaries of loss of earnings. To demand this would delay the assessment of awards and would disadvantage those who did not have comprehensive financial records, including people in insecure employment or out of the workforce who would struggle to evidence their potential earnings. We took the lead from observations of Sir Robert Francis on the calculation of support scheme payments and developed a tariff approach based on the likely impacts of infections and their severity on people’s ability to work.
This process enabled us to advise that a scheme of core awards could be designed that required only a limited amount of evidence from infected persons. We believe that this will enable appropriate compensation for the majority of beneficiaries much more quickly than a scheme based on specific assessment. It will need to be supplemented with additional amounts for those for whom the assumptions underpinning the calculations can be shown to be false (for example greater than usual care needs, or higher than average earnings) or where there are specific impacts that go beyond those identified by the clinicians as shared by most people with a particular severity of impact. Since the publication of our summary report and the Government’s proposals in May 2024, we have been able to develop more detailed advice on the supplementary awards. This element of our work has been helped considerably by the feedback that we received from the infected community through the engagement events. We describe the conclusions of this further below.
For social stigma awards and autonomy awards we have drawn from components of court awards that correspond to the elements that were described in the Compensation Study and Second Interim Report as falling under these Heads of Loss. We also examined the approaches to quantification taken in other compensation schemes that were mentioned in the Compensation Study. We also looked for comparisons from other areas of law such as privacy litigation. We explain this further below.
Sense Checking
As part of our way of working, we ‘sense-checked’ the emerging advice by developing a set of scenarios and comparing the likely outcome of successful litigation with the awards that the proposed scheme would provide, and also with the payments that would be made through the existing support schemes. The legal experts identified illustrative circumstances from contributors to the Infected Blood Inquiry, to include Treloar College victims and their families; single child and multiple sibling families. Clinical experts commented on draft scenarios to ensure that they were realistic and they were revised accordingly. Then the legal experts prepared the comparisons for discussion. This process reassured the Expert Group that the proposed scheme could be efficiently and effectively applied to common scenarios to generate proposed awards without detailed inquiry. It also showed that awards would be similar to or larger than the predicted litigation outcomes. It was noted that there were some scenarios in which the different basis on which the Support Scheme payments were calculated might lead to more generous amounts. We advised that on the basis of the ministerial commitment that no one should be worse off, there might be a need to consider transitional protections.
Taking into account other Schemes
In the Second Interim Report’s Recommendation 8, Sir Brian Langstaff proposed that the tariff should be set broadly taking into account, but not limited by, current practice in courts and tribunals across the UK and sums payable in other UK compensation schemes. Bearing this in mind, we have disregarded the ruling of the UK Supreme Court in Paul v Wolverhampton NHST [2024] UKSC 1 which was decided after the report was published. It was clear that Sir Brian believed that affected persons (who had not suffered a bereavement) were directly entitled to compensation. Given the overwhelming moral case to compensate those affected by the infected blood scandal, we felt that it would be inappropriate to take into account the Supreme Court’s position as it would exclude most affected persons from claiming in their own right.
We have also disregarded the fact that the parties in litigation will usually settle out of court and in doing so will take into account uncertainties of evidence and will be advised to accept a discounted award that reflects the risk of losing the case. The uncertainties of litigation will be high in infected blood cases due to the problems of evidence that we discuss above. However, we did not think it appropriate to apply any litigation-risk discount in our advised awards. We have, however, adopted some conventions from litigation, such as in relation to how awards for past gratuitously given care would be reduced to reflect the fact that no tax or national insurance would have been paid. We have not made any deduction for the costs of earning a wage (such as work clothes and commuting) even though this is commonly deducted in judicial awards.
Where there are differences in the approaches taken in the four UK legal jurisdictions we have aimed to use the one that best reflects the requirements of justice in the view of the expert group.
We have generally used the illustrations in the Compensation Study as a starting point in looking for appropriate comparators and then reviewed outcomes from litigation brought by infected blood victims (updating the award values for inflation). This could not be definitive as the awards reported in the judgments were often only provisional and we did not regard ourselves as limited to them. We have considered the Judicial College Guidelines, themselves developed from the precedents of the courts, as providing indicative levels for the injury award tariffs. However, these guidelines are organised by the body part that is damaged rather than infections and do not specifically address HIV, HCV, or HBV. It is therefore not straightforward to determine which aspect of the guidelines provides the most appropriate comparator. We found it more helpful to consider reported cases concerning conditions where the impacts on people’s lives were in some ways comparable, such as cancer, mild brain damage, extrapolating from them where possible.
Engagement meeting feedback
Although our terms of reference preclude taking evidence directly from members of the infected communities or their representatives, we have benefited from feedback from the engagement meetings convened by Sir Robert Francis in June 2024. These very constructive and informed observations were helpful and have led to us modifying some elements of our proposals and clarifying the rationales of others. We would have found this useful at an earlier stage in our work.
We have made a number of modifications to our advice, of which the most important concerned the the feedback that we had ‘downgraded’ the ‘Special Category Mechanism’ (SCM, using the English Infected Blood Support scheme terminology) that had been developed to recognise that some beneficiaries with chronic hepatitis had significantly greater needs than others. We reviewed the criteria used in the four nations’ schemes and considered how to incorporate them into a supplementary award category. We also considered what other conditions were equivalent as the support schemes only addressed these issues in relation to HCV. The advice set out below reflects this further consideration.
We noted the feedback that people were not able to return to work after treatments for hepatitis C and B improved as the proposed scheme anticipated. Following the evaluation of this evidence and relevant clinical studies, we propose to disregard the increased potential for work when beneficiaries either suffer from chronic fatigue or are aged 55 or more (to reflect the fact that re-entering the workforce at an older age is significantly more difficult). We believe that this should cover the examples raised at the meetings. While the expert group’s review of the evidence shows that most people are able to return to work after modern treatments this is clearly not always the case.
There were some important matters raised in the feedback that have not led us to revise our advice as we considered them to be outside our remit. This includes the issue of exemplary or punitive damages, which Sir Brian Langstaff’s Second Interim Report, Recommendation 7, said should be a matter for the courts. He did not revise that recommendation in his final report and we do not think it is an issue for the Expert Group.
We do not believe that the concerns that awards that are made to estates might not be shared in the way some participants hope can be resolved by revisiting the design of the Scheme. This is a policy issue that needs to be addressed elsewhere.
CJD (Creutzfeldt–Jakob disease) infections were not included within the scope of Sir Brian’s recommended scheme and we have therefore not considered them. We note that this was of concern to the community but have not been asked to advise on it.
The points raised about the continuation of the Support Schemes and the proper interpretation of representations made to beneficiaries are matters of policy for the Government. We have followed Recommendation 13(c) of Sir Brian Langstaff’s Second Interim report that any continued payments under the support schemes should be taken into account in assessing awards for future financial loss and care provision. We believe that the proposals based on our advice implement that recommendation.
Research Ethics Failures
A possible exception to the principle that victims share equally in their moral demands for compensation was raised in the engagement meetings convened by Sir Robert Francis. These raised the question as to whether there were additional wrongs done in respect of unethical research practices that should be treated separately. Designing the structure for such awards raises a number of complexities.
The Inquiry Report uses a number of examples to illustrate and highlight issues, but notes that these are echoed in other centres. If the unethical practices were widespread and affected all treatment centres, then this may be an example of a systemic disrespect for autonomy, such as already recognised in autonomy awards. However, if the research ethics failures affected only some victims then the Group sees a strong case for increasing autonomy awards for those who were subjected to unethical research. However, without detailed investigations it would not be easy to assess eligibility and the criteria would need to be defined.
It will be difficult to identify who participated in which types of studies from available records. It may be appropriate to make a supplementary autonomy award to those who can show that they were entered into studies but consideration needs to be given to the sense of injustice this would create for those who believe that they were wronged in this way but cannot provide evidence.
The detailed account of the failures at Treloar College shows the extent of governance failures, but also that there were some cases where parents signed consent forms although they were not properly informed. There is some evidence of parents being consulted although the degree of consultation was inadequate. The Report notes that there are different kinds of research and some was retrospective and observational (with nothing being done that would not have happened anyway). It may be that these different studies require different levels of compensation.
We have been able to have only limited discussion of these issues and have not had time to reach firm conclusions. We have not therefore offered specific advice about compensation for victims who were part of research studies. It may be that further consideration would be beneficial and that compensation should be addressed as part of this.
Heads of Loss
Sir Brian noted that ‘the underlying principle adopted by the civil courts in awarding compensation for wrong-doing is to put a successful claimant into the same position in which they would have been had they not suffered the wrong, so far as money can achieve that object.’ In order to achieve that, he recommended that the compensation scheme should provide for awards based on five components and that their quantification should reflect different impacts on people who were infected and on those who were close to them (described by Sir Brian as ‘affected’) and also take into account differences between the diseases caused by HIV, HCV and HBV and the impact of co-infections.
He recommended that compensation to both infected and affected persons should be built up from awards against the following heads of loss:
- Injury Impact Award for past and future physical and mental injury, emotional distress and injury to feelings caused by the infection and treatments for it, or being affected by them or by the death of an eligible infected person, including an award for loss of society of the deceased.
- Social Impact Award for past and future social consequences of the infection including stigma and social isolation.
- Autonomy Award as additional redress for the distress and suffering caused by the impact of the disease, including interference with family and private life (e.g. loss of opportunity to have children). This should include sums for the aggravated distress caused by interferences in their autonomy and private life such as lack of informed consent in regards to their treatment.
- Care Award for the future care needs of the eligible infected person, and to compensate for past losses in respect of care necessitated by their infection (to be paid directly to the infected person where they have paid for care, and/or directly to an affected person who has provided care).
- Financial Loss Award for past/future financial loss suffered as a result of infection.
These five heads of loss are the basis on which we have developed our advice.
The principles behind a tariff approach
Sir Brian Langstaff’s Second Interim Report recognised that the importance of an individually assessed figure for these awards should be balanced against the importance of avoiding further delay and incurring excessive cost. He therefore recommended against the Irish Tribunal Scheme because of the delays in assessing claims that followed from the preparation required for an individually assessed award. A single lump sum figure would be quicker to administer but could not reflect the differences between cases. He proposed as ‘the best compromise’ a scheme in which ‘banded awards’ were ‘set to take into account the broad features of a case, allowing for individualised assessment within those bands to the extent the bandwidth permits’. This would avoid a ‘one-size-fits-all’ process that would be quick but fail to recognise individual circumstances.
For injury awards, this tariff approach is familiar to lawyers and claims can be quantified using Judicial College Guidelines and reports of judicial awards and settlements. This was illustrated in the Compensation Study and the legal experts on the Group have been able to update the figures used by reference to more recent guidance. Although social impact and autonomy awards are novel heads of loss, some of the matters that they compensate for have been discussed in the case law and we have been able to advise on tariff amounts. The tariff for injury awards reflects the viruses with which people were infected and their clinical consequences. Those for social impact reflect the likelihood of stigma based on the responses of others. This may be independent of the actual virus involved. For affected persons, the closeness of the relationship with the infected person will generally be more significant than the specific virus.
Creating a tariff approach to care awards was more problematic. We have been able to advise on a way of calculating them that is based on a standardised profile of care needs for each of the severity bands. This creates a tariff formula rather than a set rate. This will reflect common experience and is banded so as to reflect the range of impacts of infection over a person’s life. Individualisation would not be possible without requiring extensive evidence from beneficiaries or intrusive questioning and personal assessments. That would conflict with the principles we believe should underpin the scheme. Where the core tariff formula approach would fail to reflect actual costs, this can be addressed by allowing a supplementary claim where evidence can be supplied that actual costs have exceeded the ones the model anticipated.
We have advised that a similar tariff formula should be applied to calculate financial loss. This would be based on an annual earnings figure that would be paid for each of the years of working life that have been lost due to the infection, reduced for post-retirement years to be equivalent to a workplace pension. Both Sir Brian Langstaff and Sir Robert Francis envisaged that actual financial loss would be individually assessed. However, such assessments would take time and in order to meet the principle that the Scheme should be set up in a way that enables payments to be made quickly a different approach was adopted. The tariff formula approach was suggested by examples from the Compensation Study of how financial loss could be assessed by reference to statistics on earnings (SRF 8.5) and its discussion of how a tariff for annual support payments might be fixed (SRF 9.87- 8.93). By adapting the recommendation of Sir Robert Francis to adopt the benchmark of average earnings (net of tax and National Insurance) plus 5%, we are able to suggest an approach that would match or exceed the lost earnings of the majority of people without need for specific proof. The need for individualised assessment can be met by making available a set of supplementary awards where the beneficiary has evidence that their earnings would have been higher.
Core and supplementary awards
The Expert Group’s advice is therefore that core awards can be determined applying the tariff approach. There would be fixed amounts for injury, social impact and autonomy awards and formulas for calculating care costs and financial loss that would reflect the common impact of viruses on most of those infected. However, there is a range of circumstances where we believe additional impacts will be felt by some people. Where the Expert Group believes broadly equivalent burdens are borne by most victims in a severity band, then this should be factored into the core award. Where a subset of victims can be identified where the harms are greater than this, then this should entitle them to a supplementary award. The concerns raised in the engagement meetings has led us to advise that the scope of this supplementary route should be expanded from our initial expectations and we set out our revised advice below. These supplementary award calculations would remain part of the statutory scheme. It would not be a substitute for the residual right to bring legal claims, which Sir Brian Langstaff was clear should not be removed.
Severity Bandings for people who were wrongfully infected
Sir Brian Langstaff recommended, building on the Compensation Study undertaken by Sir Robert Francis, that the scheme should reflect the different impacts of infection by developing severity bandings but did not define them. The clinical members of the Expert Group have proposed the following bandings. The Expert Group considered that it was important to ensure that the evidence required from people claiming their right to compensation should be readily available to them, be verifiable in order to enable objective assessment of their entitlement, be proportionate to the need to operate the scheme and that inappropriate intrusive questions should be avoided. Consequently, clinical markers are used to define the bandings.
Core Bandings
The below table defines the core severity bandings.
Enhanced, Advanced and ‘Special Category’ bands
Feedback from the engagement meetings has prompted us to review the need for an additional banding to reflect the greater impact that some people with HCV have experienced. We therefore reviewed the criteria used in the four national Infected Blood Support schemes where beneficiaries have shown that there has been a greater than average impact on them of chronic HCV or complications of their disease (Annex B). These are similar but not identical. The Expert Group has considered the equivalent features in relation to HBV, not currently within the scope of the support schemes and also whether they should be recognised in relation to HIV.
Some of these aspects of people’s experience have already been incorporated into core awards as the advice from the Expert Group is that they affect most people. This is the case in relation to chronic fatigue for all viruses. Others will be less common, but when they arise they will require compensation beyond the core awards. The Expert Group therefore proposes that there should be six groups of circumstances where the calculations of care needs and financial loss should be adjusted to recognise the increased impact that some beneficiaries experience from their disease. This should take the form of a supplementary route application and have the adjustments set out below. Those who have already been recognised as qualifying for the enhanced payment categories under the Support Schemes would not need to produce further evidence to qualify.
The Expert Group did consider whether there should be different injury award bandings for these categories but considers that they are best understood as uncommon consequences of the same injuries rather than separate severity bands attracting a different level of injury award. It does not therefore advise any changes to the injury, autonomy or social impact awards for people in the supplementary health impact groups.
Supplementary route health impact groups
The below tables defines the enhanced, advanced and special category bands.
- Condition as a consequence of HIV or Hepatitis B or Hepatitis C infection.
- Adjustment to care profile from date of diagnosis of condition until escalation of care required as per profile for core route.
Injury Awards
This award recognises the physical and mental injury, emotional distress and injury to feelings that may have been caused or will in future be felt as a result of infected blood and/or related medical treatments. This broadly reflects what is described in personal injury litigation as ‘general damages’ to cover pain, suffering and loss of amenity, although Sir Brian Langstaff also mentions the need to include sums for emotional distress and injury to feelings caused by the infection and treatments for it.
For people who have been infected, an injury award for each band has been calculated by reference to judicial guidelines on the damages that are appropriate in personal injury cases.
This has been done by taking the descriptions developed by clinicians of the symptoms that are typical of people with these diagnoses and examining case law and judicial guidelines for comparable cases. The values of awards in the cases were updated for inflation and this uprating is reflected in the amounts noted below. All those infected should receive at least a sum of £10,000. Additional sums would be based on the nature and impact of the infection as follows.
‘HCV exposed’ are people exposed to the virus but who, typically, will have had no symptoms nor major interference in their quality of life. Payments reflect the acknowledgement of harm in the absence of significant impact and where the psychological distress will usually be minimal. In one 2006 case of a needlestick injury where infection did not take hold, possibly because of vaccination given against HBV, an award was made of £4,000 (current updated value). People who experience specific harms not usually suffered from exposure that does not lead to a chronic infection can seek recompense via the supplementary route. We advise that the £10,000 would be an appropriate level of injury award for this band of severity.
Chronic viral hepatitis (HBV or HCV) leads to stigma and autonomy loss, which is of a similar level for both infections. Both infections are associated with impaired work capacity (more marked for HCV than HBV) that usually resolves when the virus is eliminated by treatment. There is likely to be a significant psychological impact that affects people’s ability to function, that should be reflected in the injury award for all beneficiaries in this category. Comparators have been taken from the National Blood Authority litigation (2001) and also from other personal injury cases involving liver damage, potential lifelong complications, stoma, and chronic fatigue. These comparators included compensation for the impact and side effects of treatment with interferon, where the awards ranged in 2001 from £17,000 to £45,000 (current updated values). We advise that an injury award of £60,000 would be appropriate.
Cirrhosis, regardless of the aetiology, leads to a common health impact with common needs. The impact, including psychological impact, is significantly greater than for people with chronic infection. Patients are unlikely to be able to work full time. Comparators have been taken from personal injury cases concerning severe liver damage. These awards made in the 2001 litigation ranged from £59,000 to £99,000 (current updated values). We advise that an injury award of £120,000 would be appropriate.
People with decompensated cirrhosis, regardless of cause, have enhanced care needs, will be unable to work, and will suffer significant fatigue. We think that those with liver cancer or who need a liver transplant should be banded in the same category. The injury award is calculated on the assumption that there are significant psychiatric symptoms in addition to the physical effects of the virus. Comparators have been taken from personal injury cases involving terminal cancer. For example, the proposed level of injury award is slightly above that in a 2021 case where the claimant was awarded £178,000 (current updated value) when she lost the opportunity to prevent cervical cancer, had to undergo a radical laparoscopic hysterectomy, experienced urinary incontinence, bowel problems, radiotherapy, stoma, chemotherapy, and was left with a very limited life expectation. In a 2001 case that was part of the litigation against the National Blood Authority an award of £99,000 (current updated value) was made to a claimant who had received a liver transplant as well as having received interferon earlier in her treatment. We advise that an injury award of £180,000 would be appropriate.
The estates of people who died during an acute Hepatitis B infection should receive the same injury award as those with decompensated cirrhosis or HIV as the impact of the infection was so great.
HIV mono infection is a single severity band because HIV is a lifelong infection and the vast majority of people infected with HIV through blood products will have experienced progression to advanced symptomatic HIV disease including AIDS conditions and will have died as a consequence of their infection. This group will comprise a relatively small number of people, many of whom will be deceased and relevant evidence for different subdivisions will be difficult to access. Those who have survived will continue to be severely impacted by their infection. In these circumstances, it would be disproportionately complex and onerous to disaggregate the category even if some victims might get greater compensation than they would if a detailed inquiry was carried out. The injury award is calculated on the assumption that there are significant psychiatric symptoms in addition to the physical effects of the virus. We advise that this should be the same as for those with decompensated cirrhosis, &/or liver cancer &/or liver transplantation and therefore suggest the injury award should be £180,000.
Where people have more than one infection, these injury awards need to be increased.
Co-infections cause significantly greater harm. As HIV is considered the primary infection in terms of impact, injury awards are quantified on the basis of full HIV award plus a percentage uplift of the relevant severity of Hepatitis infection, with the percentage increasing with severity. For those infected with both HBV and HCV (but not HIV), they should get a 25% uplift on the award for the most serious impact.
Social Impact Awards
The Expert Group believes that social impact awards should not differ as much across the bandings as injury awards because the stigma suffered is usually as a result of societal prejudice rather than knowledge of the clinical symptoms. We advise that there should be a single rate of £50,000 across all chronic single infections. That is fixed at the upper end of the band suggested in the report from Sir Robert Francis, who proposed a severity linked range of figures for social impact award of £10,000 for mild diseases of 0-4 years up to £51,500 for co-infected for 15+ years. The Social Impact Award would be reduced to £5,000 for those in the HCV acute band, as they most likely will not have been aware of their infection and the likelihood of stigma is reduced. It should be increased to £70,000 for those who were infected by more than one virus as the impact is likely to have been more obvious and there was therefore a greater risk of stigma.
Sir Brian Langstaff initially described this head of loss as ‘a Social Impact Award for past and future social consequences of the infection including stigma and social isolation, loss of educational opportunity, and loss of congenial employment’ (p42). The Expert Group noted that financial losses were covered separately and therefore focused on stigma and social isolation when looking for comparators for quantifying these awards.This is consistent with the formulations in the recommendations of both the Compensation Study (R8) and Second Interim Report (R6), which cover ‘past and future social consequences of the infection including stigma and social isolation.’
Autonomy Awards
There are limited comparators for the autonomy awards that Sir Brian Langstaff recommends as a new head of loss. They need to reflect the aggravated distress caused by interferences in people’s autonomy and private life such as lack of informed consent, lack of sufficient information about the risks of treatment, and about diagnosis, treatment and testing, or being the subject of research without their informed consent. They should also include the effects of lack of candour and inadequate responses by authority. These may not have all applied to every victim but they will all have experienced a lack of respect for their autonomy in some of these ways.
The Expert Group found elements of the Windrush Compensation Scheme to be the most useful guide to the quantification of this category of award, although it is not a direct comparator. Awards under that Scheme at Level 5 were for lump sums of £100,000. These include injury to feelings, anxiety and distress, family separation (social impact effect) and impact on physical and mental health. Some of these elements are covered in other Heads of Loss, leading us to suggest that autonomy awards for people who were infected should be in the range of £40,000- £50,000. We noted that the ‘very serious’ invasion of Sir Cliff Richard’s privacy by the BBC resulted in aggravated damages of £20,000, but consider this was too low to properly mark the disrespect for the autonomy in infected blood victims.
The HCV exposed autonomy award is lower as the impact was for a limited period. It is similar to the Windrush Scheme’s category of ‘Marked detriment such as inconvenience, annoyance, frustration and worry, where the effect on the claimant was fairly short lived (lasting up to a few weeks)’ which is compensated at £10,000. We suggest that this would be appropriate for HCV exposed. We think it is appropriate to uplift the autonomy awards for those with co-infections as they are likely to have experienced greater constraints on their choices.
Care Awards
Care awards aim to compensate for the cost of care that has been received, or its value if it has been given without charge. The clinical experts have set out a typical pattern of care needs after infection in the different clinical bands. Where the wrongful infection was likely to have caused death (or is likely to do so for those still living with the infection), then it would be expected that these awards need to cover a period of end-of-life care, some months of high care, and some years of moderate care, with (for those who survive longer) periods with definite but lower care needs. These patterns are typically different for those with HIV from those with Hepatitis alone. People with decompensated cirrhosis or liver cancer will typically face greater care needs for longer periods than those with cirrhosis or chronic infections.
These care needs have been costed by experts who are experienced in commissioning and delivering care to severely injured people. They made a number of revisions to and clarifications of the suggested specification of needs prior to costing the care regimes, drawing on their experience in doing so for the purposes of legal cases as well as in the arrangement of care. No account has been taken of DWP benefits or NHS continuing care payments that might be available or have been received in the past. The focus has been on identifying care needs and quantifying the award required to meet them.
Estimating care needs
Every infected person’s care needs will vary; in terms of the level of care they require, the length of time for which they will need it, and whether their needs steadily increase or fluctuate. In order to enable the scheme to make payments without detailed inquiry it is necessary to identify a pattern of likely care requirements that can form the basis of an award without any further evidence being required of beneficiaries once severity bandings have been established.
The profiling followed four steps.
- The clinical experts were asked to describe the nature of care likely to be required by people in the different severity bandings.
- The care experts were then asked to comment on whether those profiles were consistent with their experience and to cost them as they would in preparation for a legal claim.
- Following discussion of the results of these first two steps, five categories of care were defined and costed; end of life, high care, moderate care, low care, and domestic support.
- The clinical experts were then asked to advise on how much of their lives an infected person would typically need each of these categories of care.
This process has enabled the Expert Group to recommend a formula for an award to be calculated that would reflect what a court would be expected to award for a typical pattern of care.
The care bands are set out in this table. The first column provides a summary category. The second provides a description of care needs. The third explains the inputs of care that would be required to meet those needs and the cost of doing so on a commercial basis. These calculations are based on current national rates. We do not consider that it is proportionate to seek to adjust for regional rates as this would require detailed inquiries as to the place of residence of beneficiaries. These commercial rates are also used to calculate awards for future care as it gives beneficiaries the flexibility to arrange for care on a paid basis if they so choose.
Using current rates even for past care is a reasonable way to adjust for inflation. However, it is likely that care will in the past have been provided by family members or friends rather than by commercial agencies. To reflect this, the care award for past care is calculated on the basis that tax, national insurance and other costs will not have been paid. As noted by the Compensation Study paragraph 9.63 the discount of 25% that we have applied to is consistent with court practice.
Where past care has in fact been purchased at commercial rates, then a supplementary application based on evidence of invoices and payments would ensure full reimbursement.
Care Profiles
In order to calculate awards, it is necessary to determine how much care a person is likely to need in each of these categories. The clinical experts have estimated the likely duration of each category of care while a person lives with the viruses. The periods of higher care needs may not necessarily come together, as needs may wax and wane, but we believe these are reasonable estimates of the cumulative time for which each category of care will be required over their lifetime.
The lifetime care profile for those co-infected with HIV and either HCV or HBV , is estimated to be similar to someone with HIV alone. The reason for this is that the severity of disease impact in terms of the number of life threatening illnesses over a finite period is likely to be similar.
Where a person does not live for the full period after infection that is set out in this table, then it should be assumed that they have the highest level of needs for the time that they survived. That is, the amounts due under the columns from the left should be paid as a priority over those to the right. For example, the care profile of a person with HIV infection who died 10 years after infection would constitute 0.5 years of end of life care, 1.5 years of high care, 7 years of moderate care and 1 year of low care, 10 years in total.
Calculations
This approach means that once the date and nature of the infection and the clinical banding is known, a formula can be used to calculate the award due for a typical pattern of care needs. This can be paid without the need for further evidence, thereby reducing delay.
Where people’s care needs have exceeded the typical pattern, a supplementary route for additional payments should be available to cover the actual costs after assessment by the Infected Blood Compensation Authority. There may also be a need for adjustment for those in the supplementary health impact groups described above, depending on the evidence of care needs.
Care Awards should be paid to the estates of those infected persons who are deceased to cover the cost of care between the date of infection and death. For those living with wrongful infections a choice should be available between a lump sum to cover the anticipated costs over their expected years of life or periodical payments. Care awards can be paid directly to affected persons on the request of an infected person or their estate representative.
Financial Loss Awards
Courts will award compensation for the financial losses suffered by victims as a result of the wrongful injuries through loss of earnings. This usually requires detailed individual assessments and is expensive and slow to assess. It would also disadvantage those who were not in the workforce at the time of infection who will find it difficult to prove loss of earnings. Sir Brian Langstaff and Sir Robert Francis envisaged that actual financial loss would be individually assessed. However, in order to meet the principle that the Scheme should be set up in a way that enables payments to be made quickly the Expert Group has advised that a tariff formula should be applied to calculate financial loss. This would be based on an annual earnings figure that would be paid for each of the years of working life that have been lost due to the infection, reduced for post-retirement years to be equivalent to a workplace pension. An assumption would be made about the impact of the virus on earning capacity for each of the severity bands, adjusted where advances in treatment mean that those infected more recently may have had less severe financial losses than those infected longer ago.
The financial loss formula for people who were infected would take the assumed baseline salary and multiply it by the number of years when financial loss was suffered. For those who are deceased, this would be from infection to death. For living beneficiaries who wish to take a lump sum payment, this would be from the date of infection to their “healthy” life expectancy. A lump sum supplement should be added to all annual payments of, say £12,500, to cover other items such as increased insurance costs, additional transport costs. These are likely to arise from having been infected and are not significantly altered by the impact of the infection.
People will not always have been completely excluded from work by their infections. The clinical experts have advised on the likely impacts on earning potential of each of the severity bands.
They have also advised on when new treatments will be likely to have reduced the loss of earning potential, taking into account the likelihood that the NHS will not have made them widely available immediately. This element of the advice from the Expert Group was revised to take into account feedback from the Engagement Meetings that many victims of the infected blood scandal did not in fact experience the benefits that the general population gained.
The baseline earnings assumption
Sir Robert Francis suggested that the calculation of financial loss awards should provide people who were wrongfully infected with compensation based on the assumption that they would have earned 5% more than an average salary if they had not been infected. This would be paid net of tax and national insurance.
The Expert Group has adopted this as a baseline, although it noted that there might also be a case for adopting the median without the uplift, as implied in para 9.95 of the Compensation Study: ‘Where the relevant category of employment for that applicant cannot be shown, or working out a probable career path is speculative or disproportionately complex, to assess there should be a presumption that the applicant has lost income equivalent to the national median earnings.’
Adopting this baseline would provide greater compensation than a court would award to those who worked part-time hours or in insecure jobs because it assumes the same rate of remuneration during every year of working age. The Expert Group advises that this is a reasonable approach to deliver the simplicity and speed of provision that the Government wishes to see.
Higher earners
In the compensation study, Sir Robert Francis recommended that those who could prove actual loss of earnings at a higher level, that was caused by an inability to work due to the infection or its consequences, should be able to recover more. He recognised that this might be difficult to show and suggested that where there was no evidence, average earnings for a class of employment might be used using figures from the Office of National Statistics Annual Survey of Hours and Earnings (SRF 9.95). The Expert Group advises against this complication of the Scheme, noting that it could be said to disadvantage groups in irregular employment or out of paid employment. It advises that compensation for actual loss of earnings should be available via a supplementary route but that the core route should retain the single earnings rate. We note that an individualised assessment would need to take into account years when earnings were below the average (plus 5%) as well as those years when earnings were greater.
Assessing the impact of illness
The Expert Group recommends a formula based on this approach that also takes into account that the impact on a person’s ability to work will vary over time. There will be stages in a person’s life where they cannot work at all because of their infection. At other times, possibly for a long period, their ability to do work will be impaired. The clinical experts have estimated the degree of impairment, taking into account that this would have sometimes been greater prior to improvements in available treatment than it would be in the present day.
Financial loss for people infected with Hepatitis
The prevailing narrative around liver disease amongst experts is that it is largely asymptomatic and that individuals living with various forms of liver disease do not experience symptoms until the advanced stages; usually when cirrhosis develops. There is increasing recognition, however, that this is rather a simplistic point of view. Increasing numbers of studies that have investigated the impact in particular of HCV infection in people living with the virus have demonstrated that there is impairment in quality of life compared to healthy individuals. This especially manifests as fatigue as well as a phenomenon called ‘brain fog’. These symptoms are often not related to the degree of liver scarring. Based on this, it is indeed probable that individuals infected with HCV may well have experienced difficulties in employment both in terms of their ability to persist at jobs and to take on more demanding work. There is some evidence that curing individuals of HCV infection can reverse many but not all of these symptoms. This is why there is recognition in the table above of financial loss even for the more ‘mild’ stages of HCV infection with a higher percentage being awarded to those who lived with the virus prior to the widespread availability of modern directly acting antiviral therapy. The onset of cirrhosis is undeniably associated with further impairments in the quality of life in persons living with HCV and this is recognised in the uplift to the financial loss award once individuals progress to this stage. Once decompensated cirrhosis occurs or individuals are diagnosed with Hepatocellular carcinoma or undergo transplantation, then it is safe to assume that their ability to work will be severely impaired and that financial loss will be 100%.
Although the data for persons living with HBV is much less mature, preliminary studies have identified impairment in the quality of life regardless of the stage of liver disease. In light of this, the categories of financial loss are equivalent to those with HCV. For those infected with HBV who die in the acute phase of their infection, there will be a short period of financial loss and it is proposed that a flat rate of £17,500 is used for people in this category.
The ability of claimants to work may have been strongly influenced by the time frame in which infections started and therefore the treatments available to patients. A person who acquired an infection in the 2000s is likely to have a different outcome and options to manage impact on working ability compared to an individual who acquired an infection in the 1970s. The assumptions about the reductions of earning capacity that are made in calculating financial loss should be adjusted accordingly.
Hepatitis C: Effective curative treatment for HCV was widely available from 2016 onwards - these directly acting antiviral agents (DAAs) had minimal side effects (by enlarge) and were very efficacious even enabling a subset of patients with decompensated cirrhosis to improve back to compensated disease.
Hepatitis B: Effective treatment for HBV was widely introduced circa 2008 with the wider availability of Entecavir and Tenofovir. Prior to that, weaker antivirals were widely used (e.g. Lamivudine) from circa 1998 but were associated with the development of resistance making treatments ineffective.
These adjustments should not be applied from the age of 55, given how difficult it is to re-enter the workforce after a period of absence. This point was made strongly in the engagement meetings. The tables below set this out by reference to the date of birth of those who would have reached the age of 55 before the treatment advances became widely available. We hope this strikes an appropriate balance of fairness while remaining simple to administer.
Table 1: Hepatitis B- For those born before 1953
Table 2: hepatitis b- for those born after 1953, table 3: hepatitis c- for those born before 1961, table 4: hepatitis c-for those born after 1961, table 5: hepatitis co-infection- for those born before 1961, table 6: hepatitis co-infection- for those born after 1961.
Supplemental route: Whilst the categories above are designed to enable rapid processing of individual claims, it is recognised that there will be some individuals whose ability to work is fully hampered due to the fatigue they experienced. There is also clear evidence that some individuals experienced HCV or HBV-associated stigma and discrimination in the workplace. In such cases, individuals will be able to apply higher levels of financial award via the supplementary track to bring their financial loss compensation inline with their actual financial loss.
Financial Loss for people infected with HIV
HIV is a lifelong infection and the majority of those infected will have experienced progression to advanced symptomatic HIV disease including AIDS conditions and have died as a consequence of their infection.
Early antiretroviral therapies were of low efficacy and were associated with frequent and multiple adverse side effects, further limiting the capacity to work. Even when newer more tolerable treatments became available, exposure to the earlier drugs often resulted in long term sequelae such as painful peripheral neuropathies, lipodystrophy, chronic diarrhoea, pancreatic, liver and bone co-morbidities.
The life-shortening and life-damaging impact of an HIV diagnosis meant that people no longer had the educational, training and work opportunities that someone of their age might reasonably expect. There is also clear evidence of HIV associated stigma and discrimination in the workplace that further compromised the ability of people with HIV to fulfil their working ambitions and potential.
Although effective combination antiretroviral therapy became available in 1998 and will have had an immediate impact on improving survival and reduced risk of disease progression, the majority of those surviving will have continued to experience side effects from medications and symptoms from long term sequelae of severe immunodeficiency impacting on their quality of life and work capacity. It was not till the mid to late 2000s that more tolerable antiretroviral treatments with lower risk of side effects became more routinely available. Even on effective ART, ageing with HIV infection is associated with increased risk of multiple non-AIDS co-morbidities and increased frailty compared to the general population, further affecting their ability to work.
The majority of those infected will have experienced significant psychological ill health including chronic depression and anxiety and adjustment disorders impacting on ability to work and financial planning.
Because all those with HIV will have been impacted by their infection in a way that compromised their working lives, a 100% financial award is appropriate. It may be that the ability to work was compromised prior to diagnosis and treatment and this is reflected by assuming impairment rather than inability to work during the period between infection and diagnosis.
Persons co-infected with HIV and HCV/HBV infections experience a faster progression to severe liver disease when compared to those people with viral hepatitis mono-infection. Even after the availability of effective combination ART for HIV infection, those co-infected with HCV continued to experience a higher mortality from liver disease through the 2000s. There was a higher risk of treatment failure with the earlier HCV treatments in HIV co-infected patients. In addition, their access to potentially life saving liver transplants was curtailed. The direct consequences of HIV across the entire course of infection on physical and mental health compromised people’s ability to work. For people with co-infections the impact would have been even greater.
HIV and Co-infection of HIV and Hepatitis C or Hepatitis B financial loss award
Enhanced impact.
Whilst the categories above are designed to enable rapid processing of individual claims, it is recognised that there will be some individuals whose ability to work is fully hampered due to the fatigue they experienced. There is also clear evidence that some individuals experienced HCV or HBV-associated stigma and discrimination in the workplace. In such cases, individuals will be able to apply for higher levels of financial award via the supplementary track to bring their financial loss compensation inline with their actual financial loss.
There may also be a need for adjustment for those in the supplementary health impact groups described above. This is not applicable for people diagnosed as infected with HIV as it is already assumed that they would lose all their earning capacity.
Lifetime impacts
Many people who have been wrongfully infected will have the length of their working life reduced and this is a loss that must be compensated. The Expert Group proposes that for those who are deceased, awards should include compensation for earnings lost until retirement age based on average annual earnings plus 5% and for financial loss between their retirement and their death at half that rate (as would be typical for defined benefit retirement schemes). Compensation for financial losses up to the date of death would be paid to the estate of the deceased. Where there are dependants of the deceased, they should receive further compensation related to lost earnings between death and the date when the death of the deceased might have been expected in the absence of the wrongful infection. This should be paid directly to the dependants. For those living with wrongful infections a choice should be available between a lump sum to cover the anticipated financial loss during the remaining expected years of life or periodical payments.
Awards for People with Acute Hepatitis B/Hepatitis C Infection
Not all hepatitis infections become chronic. For Hepatitis C, this means that the impact will last for a shorter period during which earning capacity will have been impaired, with limited care needs and a lesser likelihood of experiencing stigma and other impacts as many of those around the infected person will be unaware that they had been infected. Most of those who suffer an acute Hepatitis B infection that clears without becoming chronic will experience limited effects and some may not even be aware that they had been infected. Sir Brian Langstaff recommended that the scheme should not compensate them. However, a small number of those infected with Hepatitis B die during the acute phase of infection. Sir Brian recognised that they require compensation. The injury, social impact and autonomy awards for these people should match those of the most badly affected HCV and HBV beneficiaries. Care awards reflect the likely intense needs at the end of life. Financial loss is a flat rate calculated on the basis of six months loss of earnings.
(*)This figure is to reflect end of life care required for the deceased infected person, discounted by 25% to reflect past care costs.
Injury awards for those affected
We recommend that injury awards should reflect the quantum of damages that would be ordered by courts in respect of psychological damage, distress, anxiety and emotional upset that are likely to have been caused. The Expert Group noted a number of potential comparators for social impact awards, including Judicial College Guidelines on ‘“the indignity, mental suffering, humiliation, distress, or anger caused” for victims in abuse cases (suggested typically to lead to awards ranging £15,000-£25,000).
No specific or additional evidence of such impacts should be required beyond establishing the relationship of the person who is affected to the infected person. The scale for injury awards should vary according to the closeness of the relationship, with the largest awards for partners, reducing for parents who have lost children, then children who have lost parents, with others getting a lower rate.
For immediate family members, where the law provides for loss of society or bereavement awards, then this should lead to an increase in injury awards in cases where the infection was likely to have contributed to an early death (cirrhosis, decompensated cirrhosis, liver cancer and HIV).
Bearing these points in mind, the Expert Group initially approached the quantification of injury awards for affected persons by considering values drawn from the middle Vento bands (awards drawn from a court case to reflect injury to feelings) as suggested by Sir Brian Langstaff on pp 44-5 of the Second Interim Report. We took the upper end of the band for partners and the lower end for others. A 20% discount was then applied for overlap between Vento awards with reference values used to set autonomy and social impact awards. We then added a psychological injury award at a flat rate of £10,000 and also a bereavement award in circumstances where it is likely that the virus had or could cause death.
As a cross-check, we then looked at the different approaches under the Fatal Accidents Acts in England, Wales and Northern Ireland and compared them to the Scottish provision for loss of society. In cases where there was or could be a bereavement, we noted that our proposals were for significantly higher awards than under the Fatal Accidents Acts but less generous than the Scottish law would provide. We therefore adjusted the amounts upwards to the mid-point of the estimates that we had been given from Scottish Law firms as likely outcomes in proceedings there.
Our advice at the end of this process is set out in the tables below.
Injury Awards for affected of HCV/HBV Cirrhosis, HCV/HBV Decompensated cirrhosis, HIV mono-infected and all Co-infected
Injury awards for affected of hcv/hbv chronic.
This approach may lead to the scheme paying more compensation when there are more affected persons in relation to a deceased infected persons. In cases of larger families this will provide greater compensation than would be payable under the Fatal Accidents Acts in England, Wales and Northern Ireland, where awards are shared. We believe this is fairer and closer to the intention of the Second Interim Report than would be achieved by a closer mimicking of that legislation.
Social Impact awards for those affected
The Expert Group recommends that there should be a flat rate of social impact award as all those close to people who are infected will have been affected by societal stigma without variation by virus, disease condition or relationship. We have understood the social impact award to reflect the stigma experienced as a result of external pressures. It would therefore be the fact of connection as perceived by outsiders rather than the closeness of that connection that would generate attention. For that reason, once people are within the scope of the ‘affected’ category, then we believe it makes sense to give them the flat rate of social impact award.
As Sir Robert Francis noted, awards under this head should be proportionate to those made to people who were infected as it would be inappropriate for those affected to receive more than they did. The recommendation is that the Social Impact award for affected persons should therefore be proportionate to the award for persons with chronic infections, bearing in mind that there may be a number of persons ‘affected’ in relation to a single infected person. These awards are not shared within the family as would be the case under the fatal Accidents legislation. It would be inappropriate for them to cumulatively be awarded more than the infected person but this is possible as each affected person receives an award in their own right. We suggest the figure of £8k as the lowest rate for infected persons recommended in the Compensation Study, discounted by 20% to reflect some overlap with the Vento awards, which had already been factored into injury awards.
Autonomy Awards for those affected
It is suggested that autonomy awards for those affected by another’s wrongful infection broadly reflect court awards for the intrusion into privacy. These awards should be made to the partners, parents and children of the infected person. For partners, we advise that a comparator of judicial awards for very serious intrusions is adopted. For parents and children, it is advised that the benchmark should be the mid-point of awards that have been made as aggravated damages in privacy cases. This leads to the following figures.
Care Awards for those affected
The Expert Group advises that care costs are part of the awards to infected persons rather than those who are affected. These costs are related to the services required by the person who is infected. They are calculated by reference to their needs. They should normally be paid directly to them (or if they have died to their estates). It will be for the infected person or those administering the estate of the deceased to choose how to divide the funds between those who provided the care in order to provide fair recompense. It would not be appropriate for the compensation scheme to take away the control from the infected person. There would therefore not be separate care awards for those who are affected by the wrongful infection of others. Rather, the costs incurred by them, and which Sir Brian Langstaff recognises must be met by the compensation scheme, would be reflected in the care awards for the persons who are infected. The Compensation Authority could be asked by beneficiaries to pay awards directly to others on their behalf.
Financial Loss for dependants
Under Fatal Accident Acts dependants are able to claim a variety of dependency awards (although of varying amounts). These cover both the loss of the financial earning power of the deceased and loss of services. In litigation cases all dependants should come forward as one claim within 3 years of the death so apportionment could be agreed with a known cohort of dependants/affected. Should the compensation scheme wish to pay the affected dependants of people who are deceased directly there would be a need to understand the size of the group of people who are dependent affected claimants. If this approach were adopted, it would therefore probably require that a deadline is set for all those who are affected to come forward before financial loss awards to the deceased person could be paid out.
Financial loss awards should be paid to dependents of an eligible deceased person in order to compensate for the support that they will have lost due to the death. These should reflect the deceased’s lost earnings between the actual and expected date of death, discounted by 25% to recognise that some of those earnings would have been spent by the deceased person on their own account. This would apply during the dependency and be derived from the formula explained above. As noted above, compensation for financial losses up to the date of death would have been paid to the estate.
Where an infected person is deceased, past financial loss from the point of infection to death is paid to the estates of the deceased person. Financial loss from the point of death to the estimated healthy life expectancy age of the deceased is paid to the affected dependants [footnote 1] registered with the Scheme. Healthy life expectancy is determined using the Office for National Statistics Expectations of Life tables and where necessary the Ogden Tables [footnote 2] .
To enable bereaved affected dependants to receive Financial Loss awards independent of when other affected persons apply for compensation, the Scheme proposes a tariff-based approach to assess the financial loss of dependants. The Scheme proposal assigns fixed proportions of financial loss to affected individuals considered most likely to have a dependency, i.e. partners and children under the age of 18 at the time of the infected person’s death. Partners or children under the age of 18 at the time of the infected person’s death would not need to provide evidence of a dependency on the infected person.
Starting from the net median UK earnings + 5% described above, we propose the Scheme assigns proportions of financial loss to bereaved affected persons. We propose the scheme first deducts 25% to reflect the expenditure that the infected person is assumed to have spent on themselves. Proportions of the remaining financial loss would then be assigned to bereaved affected persons. The proportions assigned are 75% for a partner and 25% for a child. A child who has lost both parents to infected blood related infections can claim both a child’s and partner’s tariff rate i.e. 100%.
Proposed tariff rates for Financial Loss awards to bereaved affected persons, dependent on circumstances are therefore as follows:
- Partner of an infected person at time of death: £16,682 per annum.
- Child under 18 at the time of the infected person’s death: £5,561 per annum, until the age of 18.
- Child under 18 who has lost both parents to infected blood related infections: £22,243 per annum, until the age of 18.
Other bereaved affected persons (e.g. parents or children over the age of 18 with a disability) may be eligible to receive Financial Loss awards but they would be required to provide evidence of dependency on the infected person at the time of death. This would be done via the Supplementary Route.
Beneficiaries with multiple claims
Where a recipient has multiple loved ones who have been infected, multiple injury awards will be made to reflect the scale of their loss. A single Autonomy award and Social Impact award will be made. The issuing of Financial Loss and Care awards will depend on individual circumstances. Where a person is eligible as both an infected and an affected person, the person will receive all awards due to an infected person, as well as (an) additional Injury award(s) as an affected person. A single Autonomy award and Social Impact award will be made. The issuing of Financial Loss and Care awards will depend on individual circumstances.
Sir Brian Langstaff set out the eligibility categories for the new compensation scheme. The Expert Group has advised on clarifications required to ensure that in practice the scheme will operate in accordance with the principles that have been set out above.
Eligibility for people wrongfully infected by contaminated blood or other products.
For those persons infected but not previously accepted on to a scheme, evidence of infection and receipt of a contaminated product will be needed (akin to what has been required for acceptance on to the current Infected Blood Schemes). This will include all those eligible because of HBV infection as that has not previously been covered by the Support Schemes.
In determining eligibility for new applicants, the Expert Group acknowledges there is a balance between the need to provide supportive medical evidence,that may be difficult to obtain or be considered intrusive, and the need to have sufficient information to be able to assess and exclude claims from applicants who acquired their infection by other means. In addition to clinical confirmation of infection and the applicant’s personal narrative (or in the case of an application on behalf of a deceased individual the applicant narrative), the Expert Group sets out below types of supportive evidence that could be considered in determining eligibility. The quality, extent and detail of this evidence would need to be assessed by the Infected Blood Compensation Authority vetting processes.
The Expert Group has identified relevant clinical markers of infection that ought to be documented in and accessible from medical records. The Expert Group recommends that mention of HIV, HCV and HBV on a death certificate should suffice as evidence of infection (although its absence would not be taken to exclude it). Further clarification and examples might emerge as the compensation scheme becomes operational. Where there is an absence of clear medical records of receipt of a contaminated product, the Expert Group recommends that the likelihood of receipt of a blood product could be inferred, for example from major surgical procedures, even if it is not specifically recorded in notes. The Expert Group confirms the finding of Sir Brian Langstaff that there should be no rigid cut-off that precludes claims in relation to receipt of products after any specific dates. However, this may make the causal link between their receipt and the infection unlikely and requires further inquiry.
Direct Infections
This category includes those who have been directly infected:
- with HIV through the use of NHS-supplied blood, blood products and/or tissue;
- with an acute or chronic case of Hepatitis C through the use of NHS-supplied blood, blood products and/or tissue;
- with a chronic case (more than 6 months) of Hepatitis B through the use of NHS-supplied blood, blood products and/or tissue;
- with an acute case (less than 6 months) of Hepatitis B through the use of NHS-supplied blood, blood products and/or tissue and died as a result of the Hepatitis B infection during the acute period.
Indirect Infections
A person who is or was indirectly infected when there has been
- transmission of infection from a person who is or was directly infected (e.g. a person infected by their partner); or
- transmission of infection, in defined circumstances, from another person who was infected by someone who was directly infected (e.g. a child infected by their mother who was infected by her partner).
This will not be easy to assess and the clinical experts have provided the following summary of the available evidence.
HIV: Mother to child (vertical) transmission of HIV can happen during pregnancy, during childbirth and through breast milk. Most mother to child infections happen during delivery and through breast feeding. Without anti-retroviral treatment and intervention between 25 and 30% of babies born to women living with HIV will acquire HIV. The risk of transmission is related to the mother’s viral load - the higher the viral load the greater the risk. With effective treatment for the mother, appropriate interventions during delivery and with replacement feeding the likelihood of transmission is less than 1%.
HCV: Mother to child transmission of HCV occurs in 4-6% of viraemic mothers. The timing of transmission is not clear and may be either in utero or during delivery. Mother to child transmission post delivery is very rare and breast feeding and close maternal contact are not recognised risk factors, albeit occasional transmission events by, for example, bleeding nipples may occur. Co-infection with HIV increases the risk of materno-fetal transmission, particularly in the context of high HIV viral loads. Children born to HCV infected mothers should be tested for infection during the first few months when antibodies to the virus will be present (passive transfer from the mother) but only infected children will have detectable HCV RNA. A repeat test at 12-18 months of age is recommended when maternal antibodies will have disappeared in the non-infected and at this time point a positive antibody and RNA test is confirmation of infection. Treatment with current agents is not approved for children under the age of 3 and therefore the family must wait until the child is at least 3 years old before therapy can be given. Previous treatments, interferon and ribavirin, were usually only given to older children, typically over the age of 10, although practice varied.
Fathers are not believed to infect their children.
HBV: Mother to child transmission (MTCT) is thought to be the most common route of HBV infection worldwide. The risks of transmission mainly depend on the levels of virus (HBV DNA) in the mother. The administration of hepatitis B immunoglobulin (HBIG) at birth in high risk pregnancies as well as timely birth dose vaccination and completion of the full HBV vaccination regimen significantly reduces MTCT.
In addition, antiviral therapy is recommended in the third trimester for all high risk mothers (HBV DNA >200,000 IU/ml) and has been shown to significantly reduce MTCT risk. In the absence of any preventative measures, the risk of transmission of HBV to the infants born to HBe antigen positive mothers is believed to be as high as 70-90%. With preventative measures the risks of an e antigen positive mother transmitting HBV to her child is reduced to 8-30%. Testing of infants for Hepatitis B surface antigen (HBsAg) and HBV DNA is only accurate after 6 months of birth as transient positivity in these tests can occur at the time of birth but do not necessarily indicate the establishment of chronic infection. It is important to note that routine antenatal testing for hepatitis B was introduced in the UK in 2000 and so since that date the chances of vertical transmission of HBV for children born in the UK has been significantly mitigated. The various Public Health bodies in the UK provide enhanced surveillance of maternal testing of HBV as well as preventative measures taken for confirmed cases to reduce transmission.
HBV transmission - household transmission is possible, but this is rare. Needlestick injury transmission is very rare, mainly due to at risk individuals being vaccinated against HBV.
HBV is considered a highly infectious virus, thus national and international guidelines recommend vaccination of household contacts to minimise the risk of HBV transmission. The main risk of transmission would be to children (under the age of 4 years), where HBV infection is more likely to result in a chronic infection. Exposure to older children, young adults and adults would most likely result in an acute self limiting HBV infection.
Establishing eligibility as an ‘affected’ person
Persons who are ‘affected’ become eligible under Sir Brian’s recommendations because of their connection with a person who was eligible for compensation due to their wrongful infection. The Expert Group has recommended definitions of partner, parent, child, sibling to reflect the range of family relationships as well as formal legal status.
It suggests that where eligibility is based on having provided care the threshold should be the same as that used for the ‘low’ banding of provision that is used to calculate the care awards made to persons who are infected. This marks a difference between occasional support and regular care. The Expert Group has not been able to identify ways to make workable the category of affected individuals who were ‘so close that it could reasonably be expected that their mental or physical health would be seriously affected by the consequences of the disease, and who have suffered emotionally, mentally and/or physically as a result’. The summary of our advice on eligibility criteria for affected persons is as follows.
The Expert Group believes that these recommendations will enable the Infected Blood Compensation Authority to calculate the awards to which people would be entitled under Sir Brian Langstaff’s recommendations promptly and without disproportionate requests for complex or inaccessible evidence. Our initial advice had to be provided to the Government without the opportunity to hear directly from those harmed by the contaminated blood scandal. There has been a limited opportunity for us to understand their thoughts on the advice that we offered and the Government’s decisions on the proposed Scheme. We have revised a number of our suggestions in the light of the feedback received through the Engagement Events that Sir Robert Francis KC has convened in his capacity as Interim Chair of the Infected Blood Compensation Authority. It will be for the Government to finalise the details of the Scheme and for Parliament to approve it. The Infected Blood Compensation Authority will then take on the vital task of making the payments that victims are entitled to. We hope that some measure of justice will then be achieved, albeit far too late.
Annex 1: Infected Blood Inquiry Response Expert Group Terms of Reference
(Membership Updated 17 June 2024)
Background
- In 2017, the UK government launched an independent ‘Infected Blood Inquiry’ (www.infectedbloodinquiry.org.uk) to “examine the circumstances in which men, women and children treated by National Health Services in the United Kingdom were given infected blood and infected blood products in particular since 1970” under the Inquiries Act 2005. This is the largest public inquiry ever carried out in the UK.
- The inquiry is ongoing and is expected to publish its final report on 20 May 2024. To date, there have been two interim reports published. On 29 July 2022, the Chair of the inquiry, Sir Brian Langstaff, published his first interim report on the subject of interim compensation for victims of infected blood. On 17 August 2022, the Government announced that interim payments of £100,000 would be made to infected and bereaved partner beneficiaries of the current infected blood support schemes. These payments were made by October 2022. The government has also accepted the moral case for compensation.
- On 5 April 2023, Sir Brian Langstaff’s second interim report was published outlining the Chair’s final word on compensation and recommending that work begin immediately to develop a compensation system.
- The Government is currently considering all recommendations made by Sir Brian Langstaff, alongside the 2022 Compensation Framework Study and recommendations made by Sir Robert Francis. Compensation and redress for the victims of infected blood: recommendations for a framework - GOV.UK (www.gov.uk)
- The Cabinet Office (CO) is the sponsor department for the Infected Blood Inquiry and is leading on the Government’s response. The CO has been working with other government departments, including the Department of Health and Social Care, HM Treasury, Department for Work and Pensions and Ministry Of Justice [not exhaustive], to consider the recommendations and Government’s response.
Role and Purpose of the Expert Group
- The Infected Blood Expert Group will provide expert advice (legal and clinical) to the HMG, working with officials to help develop a potential infected blood compensation framework. Advice provided by group members will be based on their area of expertise.
- Reviewing existing work undertaken by officials on policy and cost analysis;
- Advising and supporting Government in defining eligible infections and severities;
- Providing advice and support to Government on potential compensation tariffs for the eligible infected and affected beneficiaries based on infection severities, within the principles agreed by Government;
- Advising and supporting Government to develop a potential compensation framework within the principles agreed by Government;
- Members of the group are expected to work collaboratively with the Chair, other group members, CO and other cross-government officials and the Minister for the Cabinet Office.
- In addition, the Expert Group is expected to respond to any ad-hoc issues that the CO may require expert advice on during the development of the compensation framework, which might be required at short notice.
- The expertise of each group member and any evidence provided to the members (e.g. independent research / findings on infection severities and care requirements, case law on Personal Injury damages);
- Evidence and modelling provided by CO and/or other government departments or agencies;
- Evidence and feedback gathered from any separate targeted consultation with infected and affected focus groups;
- Evidence submitted to and made public by the Inquiry.
- For the avoidance of doubt, ‘evidence’, as listed above, cannot be provided by the Expert Group inviting a person (or group of people) who is not ordinarily a member of the Expert Group to attend a meeting to provide such evidence.
- The Expert Group will have representation from legal and clinical experts. The full list of expert members can be found at Annex A.
- Direct Ministerial appointed members will be remunerated for their time (to be agreed with each member separately) and reasonable travel and subsistence which will be paid in line with the CO expenses policy.
- For commercially contracted members of the group, costs will be in accordance with the CCS Framework terms and conditions or as agreed in the contract at the time of appointment.
- The Chair will also be directly appointed by the Minister for the Cabinet Office (MCO).
- The Chair and Expert Group members will nominate a deputy who would act as the Chair in their absence. The deputy Chair will chair meetings and represent the Expert Group in Government led meetings as required.
- Harness the full expertise of the Expert Group;
- Represent the views of the Expert Group;
- Act impartially and ensure the independence of the Expert Group;
- Ensure the Expert Group’s advice stays within the scope agreed by Cabinet Office;
- Act as a liaison or ‘point person’ between the secretariat (Annex B) and the Expert Group;
- Undertake the role of the Chair in addition to the role of Expert Group members, working with CO and reporting directly to the MCO.
Conflict of Interest and confidentiality
- Members will have signed a declaration form to alert the secretariat to potential conflicts of interest or concerns.
- All terms under the Letter of Engagement, particularly on confidentiality and use of official information at paragraphs 24-25 are applicable. Members will agree to honour confidentiality in terms of all information and advice provided by the MCO, CO and other government departments. The work of the Expert Group is to be treated with the strictest confidence, and the sensitivity of the discussion and individual members’ views must be respected.
- This confidentiality applies to all discussions, papers and/or evidence provided by the MCO, CO and all other government departments, to the Expert Group, to facilitate the group’s role. These papers must not be shared with anyone who is not a member of the Expert Group without consent from the Chair and CO.
- Expert Group members must not discuss or disseminate, in the public domain, any discussion or decision made by the group, CO, MCO and other government departments before, during and after work is completed on the infected blood inquiry.
- Expert Group members conduct in office should be at all times in accordance with the Nolan Report Recommendations, ‘The Seven Principles of Public Life’ which are attached as Annex C, and such relevant provisions of the Code of Conduct for Board Members of public bodies as could reasonably be applied to the appointment.
Governance and secretariat
- The Expert Group will be sponsored by the CO, who will provide a secretariat function for the group. Only the appointed Chair of the Expert Group, members, CO officials and Minister of the Cabinet Office can request a meeting of the Expert Group and commission work as appropriate.
- The Chair of the Expert Group will provide advice to CO and other government departments as appropriate, who will advise their respective Ministers. However, on occasion the Expert Group may be requested to advise Ministers directly and attend other CO led meetings and, in such instances, advance notice and prior agreement with individuals will be sought as applicable.
- The secretariat will ensure timely meeting notifications and dissemination of meeting papers and minutes.
Timing and Meetings
- The duration of the Expert Group is expected to be time limited, anticipated up to 3 months, with the possibility to extend for a further 6 months. If the Expert Group is extended, agreement from each member will be sought in advance.
- The Chair and Expert Group members will meet weekly on Thursdays for 1 hour or as required to progress work.
- The Expert Group will meet virtually (e.g. Microsoft Teams / Google meet). However, face to face meetings will be considered and if agreed, these will be held outside of the government estate, paid for by the CO.
- The quorum for a meeting of the Expert Group shall be two-thirds of members present. At least the Technical Chair or deputy Chair must be present before a meeting can commence.
Transparency
- Details of the Panel’s Terms of Reference;
- Membership of the Panel, (as agreed in the first instance the name of the Chair will be published); and
- Meeting minutes so far as appropriate to disseminate into the public domain.
Annex A: Membership of the Infected Blood Inquiry Response Expert Group
The Infected Blood Inquiry Response Expert Group is composed of legal and clinical experts, assisted by care specialists and an actuarial expert.
Chair: Professor Sir Jonathan Montgomery
Sir Jonathan is an experienced healthcare law scholar who has played a leading role in UK public bioethics for many years, having previously chaired the Human Genetics Commission (2009-2012), the Nuffield Council on Bioethics (2012-2017) and the Health Research Authority (2012-2019). Sir Jonathan is currently the Chair of the Oxford University Hospitals NHS Foundation Trust and Professor of Healthcare Law at University College London. Sir Jonathan received a knighthood in 2019 for his services to bioethics and Healthcare Law.
Clinical experts
Professor jane anderson cbe.
Consultant physician in HIV Medicine at Homerton Healthcare NHS Foundation Trust. Professor Anderson has been involved in the clinical care of people with HIV since the beginning of the epidemic. Professor Anderson is a past Chair of the British HIV Association. Professor Anderson received a CBE in 2015 for services to HIV Medicine and Sexual Health Research.
Dr David Asboe
Consultant and past Clinical Director (2014-2022) of HIV Medicine and Sexual Health, Chelsea and Westminster Hospital, London. Past Chair of the British HIV Association (2013-2016) and past Chair (2019-2022) of the NHS England Clinical Reference Group. Dr Asboe’s specialist clinical and research interests are antiretroviral resistance and treatment, sexual health of people living with HIV, and HIV and ageing.
Dr Ahmed Elsharkawy
Consultant Transplant Hepatologist at University Hospitals Birmingham with experience in Hepatitis C, Hepatitis B and Hepatitis D and extensive knowledge of liver fibrosis. Dr Elsharkawy is an honorary senior lecturer at the University of Birmingham and a Fellow of the Royal College of Physicians of London and past Chairman of the British Viral Hepatitis Group. He is the Treasurer of the British Association for the Study of the Liver and a member of the governing board of the European Association for the Study of the Liver.
Professor Graham Foster
Professor of Hepatology at Queen Mary University of London and a consultant at Barts Health Trust. Professor Foster has a long-standing interest in the management of chronic viral hepatitis and is a past President of British Association for the Study of The Liver and was previously the NHS England Clinical Lead for Hepatitis C.
Professor Patrick Kennedy
Professor of Translational Hepatology at Queen Mary University of London with extensive experience in viral liver disease. Professor Kennedy is an expert advisor for the World Health Organisation, the European Association for the Study of the Liver and he provides expert opinion for the United Kingdom Advisory Panel on blood-borne viruses. Professor Kennedy is the current chair of the British Viral Hepatitis Group and former Lead for the British Association for the Study of the Liver Hepatitis B special interest group.
Dr Ian Williams
Former senior clinical academic in the Centre for Clinical Research in Infection and Sexual health, Institute for Global Health at University College London and past honorary consultant physician at Central North West London NHS Trust and University College London Hospitals NHS Trust. Dr Williams has extensive clinical and research experience in HIV medicine since 1987. Dr Williams is a past chair of the British HIV Association and chair of the clinical reference group for HIV for NHS England from 2015 to 2019.
Legal experts
Legal advice was provided by Browne Jacobson LLP
Care experts
The Expert Group received advice from health and care expert witness agencies including:
Apex Health Associates
Lisa Barnes & Associates Ltd
Actuarial specialist.
Professor alexander mcneil .
Professor of Actuarial Science at the University of York since September 2016. Educated at Imperial College London and Cambridge University, he was formerly Assistant Professor in the Department of Mathematics at ETH Zurich and Maxwell Professor of Mathematics in the Department of Actuarial Mathematics and Statistics at Heriot-Watt University. He founded and led the Scottish Financial Risk Academy between 2010 and 2016.
Annex B: Cabinet Office contacts
Name & responsibility Contact details
Health Policy Team Lead REDACTED
Expert Group Secretariat Support REDACTED
Annex C: The Seven Principles of Public Life
Holders of public office should take decisions solely in terms of the public interest. They should not do so in order to gain financial or other material benefits for themselves, their family, or their friends.
Selflessness Holders of public office should act solely in terms of the public interest.
Integrity Holders of public office should not place themselves under any financial or other obligation to outside individuals or organisations that might influence them in their performance of their official duties.
Objectivity In carrying out public business, including making public appointments, awarding contracts, or recommending individuals for rewards and benefits, holders of public office should make choices on merit.
Accountability Holders of public office are accountable for their decisions and actions to the public and must submit themselves to whatever scrutiny is appropriate to their office.
Openness Holders of public office should be as open as possible about all the decisions and actions that they take. They should give reasons for their decisions and restrict information only when the wider public interest clearly demands.
Honesty Holders of public office have a duty to declare any private interests relating to their public duties and to take steps to resolve any conflicts arising in a way that protects the public interests.
Leadership Holders of public office should promote and support these principles by leadership and example.
These principles apply to all aspects of public life. The Committee has set them out for the benefit of all who serve the public in any way. Committee on Standards in Public Life .
Annex 2: Special Category Criteria used in the Support Schemes
Northern ireland.
Dependant as defined in the Fatal Accidents Act 1976 ↩
Ogden tables: actuarial compensation tables for injury and death ↩
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. Please fill in this survey (opens in a new tab) .

IMAGES
COMMENTS
If you have a stroke while on holiday, you might need to take a flight to get back home. If you have medical insurance, your insurance company should give you help and advice on medical treatment and getting back home. You can also contact the local British Consulate, which can offer advice and practical support. Travel and blood circulation.
For every travel insurance policy bought via this page, Different Strokes will receive a donation. This will not affect the price you pay, so benefits stroke survivors through accessing appropriate travel insurance while earning important funds for Different Strokes. My Neuro Survey. August 12, 2024No Comments.
A stroke, or mini-stroke counts as a pre-existing condition for travel insurance. You need to let your travel insurer know about the condition at quote stage and you might need to pay an extra premium to get it covered. Travel insurance with stroke cover includes protection for anything related to your condition - including hospital treatment ...
Protect your gadgets (phones, tablets, cameras, e-readers, etc.) for up to £2,000 per person when you're on holiday. Cover against accidental loss, damage, theft, and unauthorised usage. Based on. 393440. 303,770 reviews on. by Peter Holt. "Very happy with a straighforward process.
Having fulling declared your stroke, our travel insurance will cover you: For medical emergencies, including medical conditions that may arise as a result of your stroke. To use our medical emergency helpline. This means you can access assistance in the event of a medical emergency 24 hours a day, 7 days a week. For replacement medication.
AllClear are committed to providing tailored, comprehensive travel insurance policies. Get specialist cover for pre-existing medical conditions such as a stroke. Call Free 0800 848 8608. or. Get Quote Online.
You can still enjoy going on holiday after having a stroke - and with a good travel insurance policy, you can relax knowing you're fully protected. You may have to pay more for travel insurance as one of the 1.2 million stroke survivors in the UK. The type of policy you can get will depend on the severity of your stroke and its effects on you.
Stroke, cerebrovascular accident, TIA, mini stroke, brain haemorrhage - whatever the diagnosis, look to Freedom to provide a travel insurance policy Get An Online Quote Now £10,000,000
There are over 1.2 million stroke survivors in the UK and more than 100,000 strokes happen every year - our aim is to make purchasing stroke travel insurance the easiest part of your trip. What cover levels are available on travel insurance for stroke victims? We pride ourselves on being medical travel insurance specialists.
Get cheap quotes from specialist stroke travel insurance providers. Comparing quotes will make it much easier to find the right travel insurance policy to cover your medical conditions with pre-existing medical travel insurance. We work with plenty of specialist providers, and once you tell us about your trip and medical condition (s) you'll ...
Applying for travel insurance after a stroke. You can apply for travel and holiday insurance through our online quote journey or over the phone with our friendly UK call centre. We aim to make the process as simple as possible and you can rest assured that all information remains confidential. If you need assistance obtaining a quote, we ...
Compare travel insurance for stroke patients. Someone will experience a stroke every 5 minutes, with 1.3 million stroke survivors living in the UK currently. If you need travel insurance after having a stroke, here is what you can do to get the cover you need at a fair price. 1. Call and speak to a stroke travel insurance expert (or get an ...
Call our UK contact centre. 01223 446 914. Monday, Wednesday & Friday - 9am to 5pm ... It can be advisable to obtain a travel insurance for after stroke survivors quote prior to booking your trip, as depending on the destination there can be a large variation in premiums. Freedom Insurance specialise in covering pre-existing medical conditions ...
Stroke travel insurance. For stroke victims, the unpredictable nature of the condition can make the idea of travelling seem a little daunting. ... Great Lakes Insurance UK Limited is a company incorporated in England and Wales with company number 13436330 and whose registered office address is 10 Fenchurch Avenue, London, United Kingdom, EC3M 5BN.
Travel Insurance for Strokes - Your Cover. Cancellation/ curtailment up to £12,500 (£30,000 on referral) Missed departure up to £1,500 per person. Baggage up to £3,000 per person. Personal Liability up to £2 million per person. Zero excess policies available. Get a Quote.
Here are some indicative quotes for single trip and annual travel insurance for stroke patients: 7 days' trip to Europe*. 18-35 years old. £27,87. 36-55 years old. £41,18. 56+. £91,23. stroke travel insurance price.
Travel insurance after a stroke or TIA. We understand that insuring a medical condition can be a bit frustrating, and with around 100,000 people suffering from strokes every year in the UK, we want to make it as easy as possible for you to get travel insurance.So, if you or someone you care for has been affected by a stroke and are concerned about whether travel insurance will be able to cover ...
Generally, patients are advised not to travel within ten days of suffering a Transient Ischaemic Attack (Mini Stroke), but this can extend to three months or more following a Cerebrovascular Accident (Major Stroke). In all cases, you should consult your doctor about your travel plans before booking your holiday.
If you're planning a holiday and you have a heart and circulatory condition, you may need travel insurance before you book. Travel insurance isn't needed by law, but the government recommends you get covered before travelling whether you have a condition or not. Some countries require you to have cover before you can enter.
4. Care at home > Self help. Holidays should be enjoyable for everyone. When someone has had a stroke you may need to do more forward planning to ensure the trip goes smoothly from start to finish. Any extra planning will depend on how the stroke has affected the person. If they have to use a wheelchair for all or part of the journey, how often ...
AllClear Travel Insurance for stroke survivors. We work with AllClear to offer specialist Medical Travel Insurance to people affected by stroke. AllClear can cover holidays for stroke survivors. Both single trip and annual multi-trip policies are. And Different Stroke use medical travel compared. Medical Travel Compared.
A third of travellers with pre-existing medical conditions admitted they won't declare all of them when buying travel insurance this summer - up from a quarter in the spring, according to new research from travel insurer AllClear.. The research - based on surveys of travellers every three months since 2021 - also identified large numbers of customers 'cutting corners' in other ways to ...
In 2017, the UK government launched an independent 'Infected Blood Inquiry' (www.infectedbloodinquiry.org.uk) to "examine the circumstances in which men, women and children treated by ...