Website maintenance is scheduled for Saturday, October 12, and Sunday, October 13. Short disruptions may occur during these days.

TYLER S. ROGERS, MD, MBA, FAAFP, AND BRENDAN LUSHBOUGH, DO, Martin Army Community Hospital, Fort Benning, Georgia
Am Fam Physician. 2023;107(2):187-190
Author disclosure: No relevant financial relationships.

Key Clinical Issue
What are the risks and benefits of less frequent antenatal in-person visits vs. traditional visit schedules and televisits replacing some in-person antenatal appointments?
Evidence-Based Answer
Compared with traditional schedules of antenatal appointments, reducing the number of appointments showed no difference in gestational age at birth (mean difference = 0 days), likelihood of being small for gestational age (odds ratio [OR] = 1.08; 95% CI, 0.70 to 1.66), likelihood of a low Apgar score (mean difference = 0 at one and five minutes), likelihood of neonatal intensive care unit (NICU) admission (OR = 1.05; 95% CI, 0.74 to 1.50), maternal anxiety, likelihood of preterm birth (nonsignificant OR), and likelihood of low birth weight (OR = 1.02; 95% CI, 0.82 to 1.25). (Strength of Recommendation [SOR]: B, inconsistent or limited-quality patient-oriented evidence.) Studies comparing hybrid visits (i.e., televisits and in-person) with in-person visits only did not find differences in rates of preterm births (OR = 0.93; 95% CI, 0.84 to 1.03; P = .18) or rates of NICU admissions (OR = 1.02; 95% CI, 0.82 to 1.28). (SOR: B, inconsistent or limited-quality patient-oriented evidence.) There was insufficient evidence to assess other outcomes. 1
Practice Pointers
Antenatal care is a cornerstone of obstetric practice in the United States, and millions of patients receive counseling, screening, and medical care in these visits. 2 , 3 There is clear evidence supporting the benefits of antenatal care; however, the number of appointments needed and setting of visits is less understood.
The American College of Obstetricians and Gynecologists recommends antenatal visits every four weeks until 28 weeks' gestation, every two weeks until 36 weeks' gestation, and weekly thereafter, which typically involves 10 to 12 visits. 4
Expert consensus and past meta-analyses have favored fewer antenatal care visits given similar maternal and neonatal outcomes. In 1989, the U.S. Public Health Service suggested a reduction in the antenatal visit schedule based on a multidisciplinary panel and expert opinion in conjunction with a literature review; however, the American College of Obstetricians and Gynecologists has not updated its guidelines, and practices have not changed. 5 A 2010 Cochrane review found no differences in perinatal mortality between patients randomized to higher vs. reduced antenatal care groups in high-income countries, and a 2015 Cochrane review showed no difference in neonatal outcomes for women in high-income countries. 6 , 7
The Agency for Healthcare Research and Quality (AHRQ) review showed moderate- and low-strength evidence and did not find significant differences between traditional and abbreviated schedules when looking at many outcomes, such as gestational age at birth, low birth weight, Apgar scores, NICU admission, preterm birth, and maternal anxiety. The review was limited by a small evidence base with studies that are difficult to compare. The randomized controlled trials that were eligible were adjusted for confounding, whereas the nonrandomized controlled studies were not adjusted and were at high risk for confounding.
Telemedicine, defined as the use of electronic information and telecommunication to support health care among patients, clinicians, and administrators, is a new option for antenatal care delivery. 8 Televisits, the real-time communication between patients and clinicians via phone or the internet, are the specific interactions that encompass telemedicine. Recent literature suggests that supplementing in-person visits with televisits in low-risk pregnancies resulted in similar clinical outcomes and higher patient satisfaction scores. 9 The AHRQ review found no significant differences between rates of preterm births or NICU admissions for a hybrid model of televisits and in-person visits compared with in-person visits only. The review was limited due to the lack of adjustments for potential confounders in the study. For example, some of the studies were conducted during the COVID-19 pandemic, which adds multiple confounders and potential for bias.
The AHRQ review offers limited opportunity for conclusions to suggest changes in current practice. The current evidence supports past evidence, suggesting that fewer visits are not associated with neonatal or maternal harm, and televisits may have a role in antenatal care. Many of the other outcomes of interest had insufficient evidence to generate conclusions.
Editor's Note: American Family Physician SOR ratings are different from the AHRQ Strength of Evidence ratings.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army, the U.S. Department of Defense, or the U.S. government.
For the full review, go to https://effectivehealthcare.ahrq.gov/sites/default/files/product/pdf/cer-257-antenatal-care.pdf .
Balk EM, Konnyu KJ, Cao W, et al. Schedule of visits and televisits for routine antenatal care: a systematic review. Comparative effectiveness review no. 257. (Prepared by the Brown Evidence-Based Practice Center under contract no. 75Q80120D00001.) AHRQ publication no. 22-EHC031. Agency for Healthcare Research and Quality; June 2022. Accessed October 1, 2022. https://effectivehealthcare.ahrq.gov/sites/default/files/related_files/cer-257-antenatal-care-evidence-summary.pdf
Kirkham C, Harris S, Grzybowski S. Evidence-based prenatal care: part I. General prenatal care and counseling issues. Am Fam Physician. 2005;71(7):1307-1316.
Zolotor AJ, Carlough MC. Update on prenatal care. Am Fam Physician. 2014;89(3):199-208.
Kriebs JM. Guidelines for perinatal care, sixth edition: by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. J Midwifery Womens Health. 2010;55(2):e37.
Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. 1991;77(5):782-787.
Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2010(10):CD000934.
Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015(7):CD000934.
Fatehi F, Samadbeik M, Kazemi A. What is digital health? Review of definitions. Stud Health Technol Inform. 2020;275:67-71.
Cantor AG, Jungbauer RM, Totten AM, et al. Telehealth strategies for the delivery of maternal health care: a rapid review. Ann Intern Med. 2022;175(9):1285-1297.
The Agency for Healthcare Research and Quality (AHRQ) conducts the Effective Health Care Program as part of its mission to produce evidence to improve health care and to make sure the evidence is understood and used. A key clinical question based on the AHRQ Effective Health Care Program systematic review of the literature is presented, followed by an evidence-based answer based on the review. AHRQ’s summary is accompanied by an interpretation by an AFP author that will help guide clinicians in making treatment decisions.
This series is coordinated by Joanna Drowos, DO, MPH, MBA, contributing editor. A collection of Implementing AHRQ Effective Health Care Reviews published in AFP is available at https://www.aafp.org/afp/ahrq .
Continue Reading

More in AFP
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Share of mothers receiving at least four antenatal visits during pregnancy
What you should know about this indicator, how is this data described by its producer.
Antenatal care (ANC) coverage is an indicator of access and use of health care during pregnancy. The antenatal period presents opportunities for reaching pregnant women with interventions that may be vital to their health and wellbeing and that of their infants. Receiving antenatal care at least four times increases the likelihood of receiving effective maternal health interventions during the antenatal period. This is one of the indicators in the Global Strategy for Women’s, Children’s and Adolescents’ Health (2016-2030) Monitoring Framework, and one of the tracer indicators of health services for the universal health coverage (SDG indicator 3.8.1).
The percentage of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times. Due to data limitations, it is not possible to determine the type of provider for each visit. Numerator: The number of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times. Denominator: Total number of women aged 15-49 with a live birth in the same period.
Method of measurement
The number of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times during pregnancy is expressed as a percentage of women aged 15-49 with a live birth in the same period. (Number of women aged 15-49 attended at least four times during pregnancy by any provider for reasons related to the pregnancy/total number of women aged 15-49 with a live birth) *100. The ANC4+ indicator is based on a standard question that asks if and how many times the health of the woman was checked during pregnancy. Unlike antenatal care coverage (at least one visit), the indicator antenatal care coverage (at least four visits) includes care given by any provider, not just by skilled health personnel. This is because the key national level household surveys do not collect information on type of provider for each visit. Household surveys that can generate this indicator includes Demographic and Health Surveys (DHS), Multiple Indicator Cluster Surveys (MICS), Fertility and Family Surveys (FFS), Reproductive Health Surveys (RHS) and other surveys based on similar methodologies. Registry/facility reporting system can be used where the coverage is high, usually in industrialized countries.
Method of estimation
WHO compiles empirical data from nationally-representative household surveys . Before data are included into the global databases, WHO undertake a process of data verification that includes correspondence with field offices to clarify any questions regarding estimates.
Sources and processing
This data is based on the following sources, world health organization – global health observatory.
The GHO data repository is WHO's gateway to health-related statistics for its 194 Member States. It provides access to over 1000 indicators on priority health topics including mortality and burden of diseases, the Millennium Development Goals (child nutrition, child health, maternal and reproductive health, immunization, HIV/AIDS, tuberculosis, malaria, neglected diseases, water and sanitation), non communicable diseases and risk factors, epidemic-prone diseases, health systems, environmental health, violence and injuries, equity among others.
How we process data at Our World in Data
All data and visualizations on Our World in Data rely on data sourced from one or several original data providers. Preparing this original data involves several processing steps. Depending on the data, this can include standardizing country names and world region definitions, converting units, calculating derived indicators such as per capita measures, as well as adding or adapting metadata such as the name or the description given to an indicator.
At the link below you can find a detailed description of the structure of our data pipeline, including links to all the code used to prepare data across Our World in Data.
Reuse this work
- All data produced by third-party providers and made available by Our World in Data are subject to the license terms from the original providers. Our work would not be possible without the data providers we rely on, so we ask you to always cite them appropriately (see below). This is crucial to allow data providers to continue doing their work, enhancing, maintaining and updating valuable data.
- All data, visualizations, and code produced by Our World in Data are completely open access under the Creative Commons BY license . You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
How to cite this page
To cite this page overall, including any descriptions, FAQs or explanations of the data authored by Our World in Data, please use the following citation:
How to cite this data
In-line citation If you have limited space (e.g. in data visualizations), you can use this abbreviated in-line citation:
Full citation
Our World in Data is free and accessible for everyone.
Help us do this work by making a donation.
Antenatal Care
Percent distribution of antenatal care by type of provider, and percentage of antenatal care from a skilled provider.
1) Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by highest type of provider of antenatal care for most recent birth.
2) Percentage of women with a live birth or a stillbirth in the last 2 years receiving antenatal care from a skilled provider for the most recent birth.
Population base:
a) Women who have had a live birth in the 2 years preceding the survey (NR file)
b) Women who have had a stillbirth in the 2 years preceding the survey (NR file)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (NR file)
Time period: Two years preceding the survey
Numerators:
Number of women within the base population who:
1) were attended for antenatal care (ANC) for their last most recent live birth (m80 = 1) or stillbirth (m80 = 3), distributed according to the type of provider with the highest level of qualification (m2a – m2n = 1). (Note that types of providers and variables below are based on the standard DHS-8 questionnaire. Actual provider types and variables are survey specific but will be from the m2a–m2n series.) The types of providers are country specific but typically include:
a) Doctor (m2a = 1)
b) Nurse/midwife (m2b = 1)
c) Auxiliary midwife (m2c = 1)
d) Community health worker/fieldworker (m2i = 1)
e) Traditional birth attendant (m2g = 1)
f) Other (m2h = 1 or m2j = 1 or m2k = 1 or m2l = 1 or m2m = 1)
g) No ANC (m2n = 1)
2) Number of women receiving antenatal care from a skilled provider for the most recent most recent live birth (m80 = 1) or stillbirth (m80 = 3). The classification of skilled provider is also country specific, but typically includes providers such as Doctor, Nurse/midwife, and Auxiliary midwife (often m2a = 1 or m2b = 1 or m2c = 1, but depends on the survey)
Denominator: Number of women in each of the population bases:
a) Women who have had a live birth in the 2 years preceding the survey (m80 = 1 & p19 < 24)
b) Women who have had a stillbirth in the 2 years preceding the survey (m80 = 3 & p19 < 24)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (m80 = 1 or 3 & p19 < 24 )
Variables: NR file.
Calculation
During data collection respondents may mention more than one provider. The percent distribution by type of provider takes the highest type of provider from the list above and does not include other providers mentioned by the respondent.
For each type of provider, the numerator divided by the overall denominator, multiplied by 100.
Handling of Missing Values
"Don't know" or missing values on type of provider are excluded from numerators but included in denominators.
Notes and Considerations
Percent distribution adds up to 100 percent.
The category “Trained nurse/midwife” includes only medically trained and licensed personnel. Traditional birth attendants (also sometimes called midwives) are not considered skilled providers, whether trained or untrained.
The category “Traditional birth attendant/other” includes auxiliary health personnel and cases where the respondent did not know the level of qualification.
The category skilled provider typically includes doctor/nurse, midwife, and auxiliary midwife. The category ‘auxiliary midwife’ may or may not be considered skilled in providing ANC and should be adapted to reflect the country’s healthcare system as in most countries, not all cadres of health care professionals are considered “skilled” in providing ANC.
Footman, K., L. Benova, C. Goodman, D. Macleod, C. A. Lynch, L. Penn‐Kekana, and O. M. R. Campbell. 2015. "Using multi‐country household surveys to understand who provides reproductive and maternal health services in low‐and middle‐income countries: a critical appraisal of the Demographic and Health Surveys." Tropical Medicine & International Health , 20(5): 589-606.
Lawn, J. E., Blencowe, H., Waiswa, P. et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016. 387(10018), 587-603.
Wang, W., S. Alva, S. Wang, and A. Fort. 2011. Levels and trends in the use of maternal health services in developing countries. DHS Comparative Reports No. 26 . Calverton, Maryland, USA: ICF Macro. https://dhsprogram.com/publications/publication-cr26-comparative-reports.cfm
DHS-8 Tabulation plan: Table 9.1
API Indicator IDs:
RH_ANCP_W_DOC, RH_ANCP_W_NRS, RH_ANCP_W_AUX, RH_ANCP_W_CHW, RH_ANCP_W_OHW, RH_ANCP_W_TBA, RH_ANCP_W_OTH, RH_ANCP_W_MIS, RH_ANCP_W_NON, RH_ANCP_W_SKP
( API link , STATcompiler link )
MICS6 Indicator TM.5a: Antenatal care coverage: at least once by skilled health personnel.
Changes over Time
This indicator changed significantly in DHS-8. The reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Also, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey. Finally, the categories of providers changed slightly. “Auxiliary nurse/midwife” was changed to “Auxiliary midwife” and “Community health worker” was changed to “Community health worker/fieldworker”.
Percent distribution of number of antenatal care visits, and of timing of first antenatal visit
1) Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by number of antenatal care visits for most recent birth.
2) Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by number of months pregnant at time of first antenatal care visit for most recent birth.
1) Received antenatal care for their last most recent live birth (m80 = 1) and/or stillbirth (m80 = 3), according to grouped number of visits (m14)
2) Received antenatal care for their last most recent live birth (m80 = 1) and/or stillbirth (m80 = 3), according to grouped number of months they were pregnant at time of first visit (m13)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (m80 = 1 or 3 & p19 < 24)
Number of antenatal visits is grouped into categories of no antenatal visits, 1 visit, 2 visits, 3 visits, 4-7 visits, 8+ visits, and “don’t know” before calculating percentages. Timing of first antenatal visit is grouped into categories of no antenatal visit, <4 months, 4-6 months, 7+ months, and “don’t know” before calculating percentages. The percentages are the numerators divided by the denominator, multiplied by 100.
"Don't know" or missing values on number of antenatal care visits and timing of first ANC are excluded from numerators but included in denominators.
Percent distributions add up to 100 percent.
In DHS-8, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. The population base for this indicator was also expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey.
Also, in DHS-8, the groupings were changed to include 8+ ANC visits based on WHO recommendations.
Benova, L., Ö. Tunçalp, A.C. Moran and O.M.R. Campbell, 2018. “Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries.” BMJ Global Health , 3 (2), p.e000779. https://gh.bmj.com/content/3/2/e000779
MacQuarrie, K.L.D., L. Mallick, and C. Allen. 2017. Sexual and reproductive health in early and later adolescence: DHS data on youth Age 10-19 . DHS Comparative Reports No. 45. Rockville, Maryland, USA: ICF. https://dhsprogram.com/publications/publication-cr45-comparative-reports.cfm
Owolabi, O.O., K.L.M. Wong, M.L. Dennis, E. Radovich, F.L. Cavallaro, C.A. Lynch, A. Fatusi, I. Sombie, and L. Benova. 2017. "Comparing the Use and Content of Antenatal Care in Adolescent and Older First-Time Mothers in 13 Countries of West Africa: A Cross-Sectional Analysis of Demographic and Health Surveys." The Lancet Child & Adolescent Health 1(3):203-212. https://www.sciencedirect.com/science/article/pii/S2352464217300251
Wang, W., S. Alva, S. Wang, and A. Fort. 2011. Levels and trends in the use of maternal health services in developing countries . DHS Comparative Reports No. 26. Calverton, Maryland, USA: ICF Macro. https://dhsprogram.com/publications/publication-cr26-comparative-reports.cfm
World Health Organization. 2016. WHO recommendations on antenatal care for a positive pregnancy experience . Geneva: World Health Organization. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/
World Health Organization. 2018. Global reference list of 100 core health indicators . Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/259951
DHS-8 Tabulation plan: Table 9.2
RH_ANCN_W_NON, RH_ANCN_W_N01, RH_ANCN_W_N23, RH_ANCN_W_N4P, RH_ANCN_W_DKM,
RH_ANCT_W_NON, RH_ANCT_W_TL4, RH_ANCT_W_T45, RH_ANCT_W_T67, RH_ANCT_W_T8P, RH_ANCT_W_DKM
WHO 100 Core Health Indicators: Antenatal care coverage
MICS6 Indicator TM.5b: Antenatal care coverage: at least four times by any provider.
MICS6 Indicator TM.5c: Antenatal care coverage: at least eight times by any provider
Median number of months pregnant at time of first antenatal care visit
Median number of months pregnant at the time of first antenatal care visit for the most recent birth (live birth or stillbirth) in the 2 years preceding the survey.
a) Women who have had alive birth in the 2 years preceding the survey (NR file)
Time period: Two years preceding the survey.
Number of women within each base population who received antenatal care for their most recent live birth (m80 = 1) or stillbirth (m80 = 3) according to the single number of months they were pregnant at time of first visit (m13)
a) Women who have had a live birth in the 2 years preceding the survey who received antenatal care for the live birth (m80 = 1 & m13 < 96 & p19 < 24)
b) Women who have had a stillbirth in the 2 years preceding the survey who received antenatal care for the stillbirth (m80 = 3 & m13 < 96 & p19 < 24)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who received antenatal care for their last birth (m80 = 1 or 3 & m13 < 96 & p19 < 24)
For the median, first calculate percentages of single months pregnant at first visit by dividing the numerators by the denominator. Cumulate the percentages by single months starting with the lowest value.
Linearly interpolate between the number of months immediately before and after where the cumulated distribution exceeds 50 percent to determine the median. See Median Calculations in Chapter 1 .
“Don’t know” and missing values excluded from numerators and denominator of percentages for median calculation.
In DHS-8, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Also, in DHS-8, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey.
DHS-8 Tabulation plan: Table 9.2
RH_ANCT_W_MED
Percentage of women receiving components of antenatal care
1) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had their blood pressure measured.
2) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had a urine sample taken.
3) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had a blood sample taken.
4) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had the baby’s heartbeat listened for.
5) Among women with a live birth or a stillbirth in the last 2 years the percentage that were counseled about maternal diet.
6) Among women with a live birth or a stillbirth in the last 2 years the percentage that were counseled about breastfeeding.
7) Among women with a live birth or a stillbirth in the last 2 years, the percentage that were asked about vaginal bleeding.
b) Women who received antenatal care for their most recent live birth in the 2 years preceding the survey (NR file)
c) Women who have had a stillbirth in the 2 years preceding the survey (NR file)
d) Women who received antenatal care for their most recent stillbirth in the 2 years preceding the survey (NR file)
e) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (NR file)
f) Women who received antenatal care for their most recent birth (live birth or stillbirth) in the 2 years preceding the survey (NR file)
Number of women within each base population who:
1) had their blood pressure measured (m42c = 1)
2) had a urine sample taken (m42d = 1)
3) had a blood sample taken (m42e = 1)
4) had baby’s heartbeat listened for (m42f = 1)
5) were counseled about maternal diet (m42g = 1)
6) were counseled about breastfeeding (m42h = 1)
7) were asked about vaginal bleeding (m42i = 1)
Denominators: Number of women in each of the population bases:
b) Women who have had a live birth in the 2 years preceding the survey who received antenatal care for their last birth (m80 = 1 & m2n = 0 & p19 < 24)
c) Women who have had a stillbirth in the 2 years preceding the survey (m80 = 3 & p19 < 24)
d) Women who have had a stillbirth in the 2 years preceding the survey who received antenatal care for their stillbirth (m80 = 3 & m2n = 0 & p19 < 24)
e) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (m80 = 1 or 3 & p19 < 24)
f) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who received antenatal care for their last birth (m80 = 1 or 3 & m2n = 0 & p19 < 24)
For percentages, the numerator divided by the denominator, multiplied by 100.
“Don’t know” and missing values on key components of antenatal care (e.g., urine sample taken) are excluded from numerators but included in denominators, assuming that they did not receive the antenatal care component.
In DHS-8, a number of changes were made to indicators on content of ANC. First, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Second, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey. Additionally, maternal report of receipt of these specific items of ANC are now reported among both number of women with a livebirth and/or stillbirth in the last 2 years AND number of women who attended ANC for their livebirth and/or stillbirth in the last 2 years.
Several additional key items for content of ANC were added as a proxy for quality of care. These included listening to the baby’s heartbeat and counseling on maternal diet and breastfeeding.
Indicators on iron-supplementation and deworming used to be included in the same table as these components but are now presented in a separate table.
DHS-8 Tabulation plan: Tables 9.3.1 and 9.3.2
RH_ANCC_W_IRN, RH_ANCC_W_PAR, RH_ANCS_W_BLP, RH_ANCS_W_URN, RH_ANCS_W_BLS
MICS6 Indicator TM.6: Content of antenatal care
Percentage of women receiving food/cash assistance, deworming, and iron-containing supplementation during pregnancy
1) Percentage of women with a live birth or a stillbirth in the last 2 years who received food or cash assistance during their most recent pregnancy.
2) Percentage of women with a live birth or a stillbirth in the last 2 years who took intestinal parasite drugs during their most recent pregnancy.
3) Percentage of women with a live birth or a stillbirth in the last 2 years who took iron tablets or syrup during their most recent pregnancy.
1) received food or cash assistance during the pregnancy of the most recent live birth or stillbirth (m82 = 1)
2) took iron tablets or syrup during the pregnancy for the most recent live birth or stillbirth (m45 = 1)
3) took intestinal parasite drugs during the pregnancy for the most recent live birth or stillbirth (m60 = 1)
“Don’t know” and missing values on indicators of food/cash assistance, deworming, and iron-containing supplementation are excluded from numerators but included in denominators, assuming that they did not receive the intervention.
In DHS-8, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Also in DHS-8, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey.
The indicator on food/cash assistance was added in DHS-8. The indicators on iron-supplementation and deworming used to be included in the same table as the other ANC components but are now presented in a separate table.
Bhutta ZA, Das JK, Bahl R, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014;384(9940):347–70
DHS-8 Tabulation plan: Table 9.4
Percent distribution of number of days taking iron-containing supplements during pregnancy
Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by number of days taking iron-containing supplements during their most recent pregnancy.
Number of women within each base population who by number of days she took iron-containing supplements during the most recent pregnancy (m46)
Number of days during which women took iron-containing supplements is grouped into categories of none, <60, 60-89, 90-179, 180+, and “don’t know” before calculating percentages. Percentages are the numerators divided by the denominator, multiplied by 100.
“Don’t know” values included in percent distributions. Missing values are excluded from numerators but included in denominators.
(API link TBD, STATcompiler link TBD)
Percentage of women who obtained iron-containing supplements, by source of supplements
Percentage of women with a live birth or a stillbirth in the last 2 years who obtained iron-containing supplements during their most recent pregnancy, by source of supplements.
a) Women who have had a live birth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent live birth (NR file)
b) Women who have had a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent stillbirth (NR file)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the most recent pregnancy (NR file)
Number of women within each base population who were given or bought iron-containing supplements during pregnancy, by declared source of iron-containing supplements (m45 = 1 & m81a – x)
a) Women who have had a live birth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent live birth (m80 = 1 & m45 =1 & p19 < 24)
b) Women who have had a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent stillbirth (m80 = 3 & m45 =1 & p19 < 24)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the most recent pregnancy (m80 = 1 or 3 & m45 =1 & p19 < 24)
Numerators divided by the same denominator and multiplied by 100.
Supplements may have been obtained from more than one source.
DHS-8 Tabulation plan: Table 9.5
Loading metrics
Open Access
Peer-reviewed
Research Article
Number of antenatal care visits and associated factors among reproductive age women in Sub-Saharan Africa using recent demographic and health survey data from 2008–2019: A multilevel negative binomial regression model
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Epidemiology, Gambella Regional Health Bureau, Gambella, Ethiopia
Affiliation Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Affiliation Department of Human Nutrition, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
* E-mail: [email protected]
Affiliation Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- Fetene Getnet Gebeyehu,
- Bisrat Misganaw Geremew,
- Aysheshim Kassahun Belew,
- Melkamu Aderajew Zemene

- Published: December 27, 2022
- https://doi.org/10.1371/journal.pgph.0001180
- Peer Review
- Reader Comments
Antenatal care is one of the best strategies for maternal and neonatal mortality reduction. There is a paucity of evidence on the mean number of ANC visits and associated factors in Sub-Saharan Africa (SSA). This study aimed to investigate the mean number of ANC visits and associated factors among reproductive-age women in Sub-Saharan Africa using the Demographic and Health Survey conducted from 2008 to 2019.
A total of 256,425 weighted numbers of women who gave birth five years before the survey were included. We used STATA version 14 for data management and analysis. A multilevel negative binomial regression model was fitted. Finally, the Adjusted Incident Rate Ratio (AIRR) with its 95% CI confidence interval was reported. Statistical significance was declared at P-value < 0.05.
The mean number of ANC visits among women who gave birth five years before the survey in SSA was 3.83 (95% CI = 3.82, 3.84) Individual-level factors such as being aged 36–49 years (AIRR = 1.20, 95% CI = 1.18,1.21), having secondary education &above (AIRR = 1.44, 95% CI = 1.42, 1.45), having rich wealth status (AIRR = 1.08, 95% CI = 1.07, 1.09), media exposure (AIRR = 1.10, 95% CI = 1.09,1.11), and grand multiparity (AIRR = 0.90, 95% CI = 0.89, 0.91) were significantly associated with the number of ANC visits. Furthermore, rural residence (AIRR = 0.90, 95% CI = 0.89, 0.91), Western SSA region (AIRR = 1.19, 95% CI = 1.18, 1.20) and being from a middle-income country (AIRR = 1.09, 95% CI = 1.08, 1.10) were community-level factors that had a significant association with the number of ANC visits.
The mean number of ANC visits in SSA approximates the minimum recommended number of ANC visits by the World Health Organization. Women’s educational status, women’s age, media exposure, parity, planned pregnancy, wealth status, residence, country’s income, and region of SSA had a significant association with the frequency of ANC visits. This study suggests that addressing geographical disparities and socio-economic inequalities will help to alleviate the reduced utilization of ANC services.
Citation: Gebeyehu FG, Geremew BM, Belew AK, Zemene MA (2022) Number of antenatal care visits and associated factors among reproductive age women in Sub-Saharan Africa using recent demographic and health survey data from 2008–2019: A multilevel negative binomial regression model. PLOS Glob Public Health 2(12): e0001180. https://doi.org/10.1371/journal.pgph.0001180
Editor: Jitendra Kumar Singh, Janaki Medical College, Tribhuvan University, NEPAL
Received: May 27, 2022; Accepted: November 27, 2022; Published: December 27, 2022
Copyright: © 2022 Gebeyehu et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The dataset is available from the DHS program official database www.measuredhs.com .
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Antenatal care (ANC) is care provided by skilled healthcare professionals to pregnant women to ensure the best health conditions for both the mother and fetus during pregnancy [ 1 ]. ANC decreases maternal and perinatal morbidity and mortality [ 2 ]. The ANC service includes birth preparedness, advice on danger signs of pregnancy, counseling on optimal nutrition, prevention, identification and treatment of obstetric complications, and advice on options for family planning [ 3 ].
Maternal death is defined as the death of a woman while pregnant or within 42 days of the pregnancy’s termination from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes [ 4 ]. Child and maternal mortality continued to be major public health concerns in developing countries. Yearly, 527,000 women in low-income countries die from pregnancy-related complications, and nearly 4 million neonates die in their first of which 98% are from developing countries [ 5 ].
According to the World Health Organization (WHO) sustainable development goal (SDG) 3, countries should reduce child mortality to less than 25 deaths per 1,000 live births and maternal mortality to less than 70 per 100,000 live births by the year 2030 [ 6 ]. Although 121 countries had met the target on under-5 mortality, progress will need to accelerate in 53 countries, two-thirds of which are in sub-Saharan Africa [ 7 ]. Studies showed that utilization of at least one antenatal care visit by a skilled provider during pregnancy decreases the risk of neonatal mortality by 39% in sub-Saharan African countries. Thus, to accelerate progress toward the reduction of neonatal mortality, all pregnant women should receive antenatal care [ 8 ].
Globally, 87% of pregnant women received antenatal care visits at least once, and only 60% received the minimum required number of antenatal care visits [ 3 ]. In Sub-Saharan Africa, 49–53% of women received the minimum recommended number of ANC visits 35% accessed at least one visit and 13% of women had no antenatal care visits [ 9 ].
Due to the high burden of maternal and child mortality, WHO adopted the focused antenatal care model by the year 2002, which recommends a minimum of four antenatal care visits by a pregnant woman [ 10 ]. By the year 2016, at the start of the Sustainable Development Goal era, maternal and child mortality was unacceptably high and the world health organization changed the focused ANC model to an essential core package of routine ANC and the number of visits increased to eight [ 1 ].
Previous studies affirmed that Place of residence [ 11 , 12 ], wealth status [ 13 , 14 ], educational status [ 15 , 16 ], distance from a health facility [ 17 , 18 ], quality of health service [ 19 , 20 ], and cost of service [ 21 ] were factors associated with the number of antenatal care visit. Barriers to quality maternal health care must be recognized and addressed at all levels of the health system to enhance maternal health [ 22 ].
Though there are studies on the prevalence of ANC and associated factors in different African countries, we found limited evidence on the mean number of ANC visits and associated factors in SSA using the count model. Since most of the studies were conducted using binary logistic regression, information was lost while categorizing women’s different numbers of visits in the same group. Most of the studies focused on factors associated with the timing of the first ANC initiation. There is a paucity of information on the average number of ANC visits and associated factors among women in SSA.
The count model has the added benefit of estimating the mean number of ANC visits and associated factors, and information loss may not be an issue. Therefore, this study aimed to investigate the mean number of antenatal care visits and associated factors among reproductive-age women in SSA based on the 2008 to 2019 Demographic and Health Survey data.
Methods and materials
Study design, area, and period.
Secondary data analysis was conducted based on the recent Demographic and Health Survey (DHS) data of 35 Sub-Saharan African countries from 2008 to 2019. According to the United Nations geo scheme classification, the continent of Africa is commonly divided into five regions [ 23 ]. Sub-Saharan Africa contains four of these regions namely Eastern Africa, Central Africa, Western Africa, and Southern Africa. This study was conducted in these regions using their recent DHS datasets.
Source and study population
The source population was all reproductive-age women who gave birth five years before each respective survey in Sub-Saharan Africa, whereas those in the selected Enumeration Areas (EAs) were the study population. The sample size was determined from the kids to recode file “KR file” from the standard DHS dataset of Sub-Saharan African countries with at least one survey from 2008 to 2019. DHS uses a two-stage stratified cluster sampling technique. In the first stage, a sample of EAs was selected independently from each stratum with proportional allocation stratified by residence (urban & rural). In the second stage, from the selected EAs, households were taken by systematic sampling technique [ 24 ]. The final sample size was 257,924 (weighted sample 256, 425) women.
Variables and data collection procedure
The outcome variable was the number of antenatal care visits. The independent variables for this study were from two sources such as individual and community-level factors. The individual-level factors include; socio-economic and demographic-related factors, pregnancy-related factors, and behavioral-related factors. Community-level factors include; community-level media exposure, community-level women’s education, place of residence, sub-regions within SSA, and year of the survey. The data were accessed and downloaded from the webpage of the international Demographic and Health Survey.
Operational definitions
The number of antenatal care visits..
Non-negative integer for which this study aims to identify a proper count regression model.
Media exposure.
It was obtained by aggregating women’s exposure to television, radio, and newspaper and if women had been exposed at least once a week it was coded as “1” for yes, and if a woman had not been exposed at least once a week it was coded as “0” for no.
Wealth status.
Is a composite measure of a household’s cumulative living standard divided into 5 quantiles using the wealth quantile data derived from principal component analysis. Finally, it was coded as "0" for the poor, "1" for the middle, and "2" for the rich.
Community-level media exposure.
Was obtained by aggregating the individual level media exposure at the cluster level by using the proportion of women who had media exposure and it was coded as “0” for low (communities in which < 50% of women had media exposure), “1” for high community-level media exposure. This community-level media exposure shows the overall media exposure in the community.
Community-women education.
It was obtained by aggregating the individual-level women’s education into clusters by using the proportion of women who had attended at least primary education. It was coded as “0” for low (communities in which < 50% of women had at least primary education), and “1” for high community-Community-level.
Year of the survey.
The period when the survey was conducted.
Data analysis
The data was cleaned, coded, and extracted using MS excel and STATA version 14 software. Variables with missed values greater than 5% / not applicable were dropped. During data cleaning and coding, the same STATA command was applied for each country. After coding and cleaning the dataset for each country independently, all country dataset was appended to one dataset for further analysis. Sample weighting was done for each country before appending it to one dataset.
Poisson regression model
The standard Poisson regression model was the first model considered while working with count data. It is a technique used to describe count data as a function of a set of independent variables and which assumes the observations should be independent over time and the mean and the variance of the dependent variable should be equal [ 25 ].
However, the assumption of the Poisson regression failed (the sample variance exceeds the sample mean), in the case of overdispersion. In such a case the negative binomial regression model that includes an unobserved specific effect (random term or error term) for the parameter was the preferred one to handle the overdispersion. A Likelihood Ratio(LR) test for the parameter α (p-value < 0.001) was used for the over-dispersion parameter, in the negative binomial (NB) specification against the Poisson model specification [ 26 ].
Multilevel model building
Since DHS data has hierarchical nature different measures of variation (intra-class correlation coefficient (ICC), and Median Incident Rate Ratio (MIRR)) were calculated to detect any clustering effect. Finally, four multilevel count models were fitted.
First, a ‘‘ null ” model ( model 1 ), which only includes a random intercept and allows us to detect the existence of a possible contextual dimension for a phenomenon was estimated and provided evidence to assess random effect using the Intraclass Correlation Coefficient (ICC). Then the individual characteristics were included in the model ( model 2 ) to investigate the extent to which the overall difference in the number of ANC visits was explained by the individual variation. Next, community-level variables were added to the model ( model 3 ) to investigate whether this contextual phenomenon was conditioned by community-level characteristics. Finally, both individual and community-level characteristics were added to the model ( model 4 ) at the same time as the number of ANC visits.
Parameter estimation method
The fixed effects (a measure of association) were used to estimate the association between explanatory variables and the number of ANC visits at both individual and community levels. Factors with a p-value ≤ 0.25 were selected as candidates for the final model. The crude Incident Rate Ratio (CIRR) and the Adjusted Incident Rate Ratio (AIRR) were assessed and finally Adjusted Rate Ratio (AIRR) was presented. Associations between dependent and independent variables were assessed and their strength was presented using adjusted rate ratios and 95% confidence intervals with a p-value of <0.05.
The variance inflation factor (VIF) was assessed to check for multi-linearity and the mean VIF for the fitted model was 1.86. Finally, a model comparison was done using the deviance test, and the model with the lowest deviance was selected as the best-fit model.
Ethical consideration
The waiver of written informed consent was approved by the University of Gondar Institutional Review Board (IRB). As well, after online requesting and explaining the objective of this study to DHS Program/ICF International Inc., a letter of permission was waived from the International Review Board of Demographic and Health Surveys (DHS) program data archivists to download the dataset for this study. The data was not shared or passed on to other researchers.
Socio-demographic characteristics of respondents
A total of 257,924 reproductive-age women who gave birth within five years before the survey were included. The median age of women was 28 years with Inter Quartile Range (IQR) of 23–34 years. Nearly three fourth (72.3%) of the study participants were between the age of 20–35 years. More than one-third (38.43%)of the participants had no formal education. Nearly half (45.71%) of the respondents were from poor and poorest households, and about two-thirds (66.85%) were from rural areas. More than three fourth (77%) of the respondents were from the eastern and western regions of sub-Saharan Africa. And approximately one-third (28%) of the pregnancies were unwanted ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0001180.t001
Number of ANC visits during pregnancy
The mean number of ANC visits in SSA was 3.83 (95% CI = 3.82, 3.84) with the minimum average number of visits among Chadian women (2.29, 95% CI = 2.26, 2.34) and maximum average number of visits among Ghanan women (6.44, 95% CI = 6.35, 6.53). There was also a difference in the mean numbers of ANC visit among regions of SSA with 3.55 (95% CI = 3.53, 3.58) for women from the Central region, 3.66 (95% CI = 3.65, 3.67) for women from the Eastern region, 4.02 (95% CI = 4.00, 4.04) for women from Western region and 4.99 (95% CI = 4.93, 5.06) for women from Southern region.
Multilevel negative binomial regression analysis
Random effect and model comparison results.
Although we considered fitting different count models, we preferred the negative binomial regression model to the standard Poisson regression model as the sample variance (6.6) exceeds the sample mean (3.83) and the Likelihood Ratio (LR) test became significant (p-value <0.001). The data were also checked for excess zeros to determine if there was a possibility to choose models that are suitable for data with an inflated number of zeros (ZIP, ZINB, HP, and HNB). Different measures of variations were calculated to determine whether there is a clustering effect or not. First, the intra-class correlation was calculated and it affirmed that the total variability in the number of ANC visits explained by the cluster variation was only 1.1% ( Table 2 ). This indicated that the cluster variation was not large to use a multilevel model instead of the standard negative binomial regression model, but it is not always true [ 28 ].
https://doi.org/10.1371/journal.pgph.0001180.t002
Furthermore, we could use a likelihood ratio test to compare the likely hood of the fitted multilevel model with the standard model [ 29 ]. The p-value associated with the chi-squared statistics was less than 0.001, hence we would reject the null hypothesis of no between-cluster variation in the rate of occurrence of the outcome (number of ANC visits). In addition, the median incident rate ratio (MIRR) allows us to determine the median relative change in the rate of occurrence of the outcome (number of ANC visits) between an individual in a cluster with a high rate of outcome (ANC visit) and an individual from a cluster with a low rate of outcome (ANC visit) was calculated. The MIRR for the null model became significant (MIRR = 1.20, 95% CI = 1.18,1,21) ( Table 2 ), which tells us doing a multilevel model was preferred over the standard model [ 29 ].
The percent change of variance (PCV) which measures the total variation attributed to individual-level and cluster-level factors was calculated. The deviance test was used to select the best-fitted model and its values are decreasing across model 1 to model 4. Therefore model 4 was the model with the lowest deviance test value and it became the preferred model. The Percent change variation in the final model showed that about 63.6% of the total variability in the number of antenatal care visits was explained by the full model.
Fixed effect results; multilevel negative binomial regression analysis
Maternal age, maternal education, wealth status, media usage, and parity are individual-level factors that had a significant association with the number of ANC visits in the final model. The frequency of ANC visits increased by 8% (AIRR = 1.08, CI = 1.07, 1.10) and 18% (AIRR = 1.18, 95% CI = 1.16, 1.20) for women aged 20–35 and above 35 as compared to women of 15–19 years of age, respectively. Primary education and secondary & above had increased the frequency of ANC visits by 26% (AIRR = 1.26, 95% CI = 1.25, 1.27) and 44% (AIRR = 1.44, 95% CI = 1.42, 1.45) compared with women with no education, respectively. Middle and rich wealth status had increased the frequency of ANC visits by 5% (AIRR = 1.05, 95% CI = 1.04, 1.06) and 8% (AIRR = 1.08, 95% CI = 1.07, 1.09) respectively as compared to women of poor wealth status. Women’s media exposure had increased the frequency of ANC visits by 10% (AIRR = 1.10, 95% CI = 1.09, 1.11) when compared to women with no media exposure. Whereas multiparity and grand multiparity decreased the frequency of ANC visits by 2% (AIRR = 0.98, 95% CI = 0.97, 0.99) and 10% (AIRR = 0.90, 95% CI = 0.89, 0.91) respectively when compared with primiparity. Women with planned pregnancies had 3 percentage points (AIRR = 0.97, 95% CI = 0.96, 0.98) reduced frequency of ANC visits when compared with their counterparts.
Furthermore, community-level factors were significantly associated with the frequency of ANC visits. Women from the rural residence had 10% (AIRR = 0.90, 95% CI = 0.89–0.91) lower ANC visits than their counterparts. Women from Eastern, Southern, and Western SSA regions had 3% (AIRR = 1.03, 95% CI = 1.02, 1.04), 11% (AIRR = 1.11, 95% CI = 1.09, 1.13), and 17% (AIRR = 1.17, 95% CI = 1.16, 1.18) number of ANC visit respectively when compared to women from central SSA region. Women from the community with a high level of media exposure and high level of women’s education had 3% (AIRR = 1.03, 95% CI = 1.02, 1.04) and 2% (AIRR = 1.02, 95% CI = 1.01–1.03) increment with a frequency of ANC visit respectively compared with those from a lower level. Women from middle-income countries had 10% (AIRR = 1.10, 95% CI = 1.09, 1.11) of a greater number of ANC visits compared to their counterparts. In addition, women surveyed from 2012–2015 and 2016–2019 had 5% (AIRR = 1.05, 0.95% CI = 1.04, 1.06) and 7% (AIRR = 1.07, CI = 1.06, 1.08) a greater number of ANC visits when compared with women surveyed from 2008–2011 ( Table 3 ).
https://doi.org/10.1371/journal.pgph.0001180.t003
Antenatal care is an indicator to measure the efficiency of maternal care utilization. It helps in preventing adverse pregnancy outcomes when provided early in the pregnancy and continued through delivery. Identification of problems in pregnancy results in early referrals for women with complications. So this study focused on the mean number of ANC visits and determinants of the number of Antenatal care visits in SSA using the multilevel negative binomial analysis to estimate individual and community-level factors.
This study revealed that although the mean number of ANC visits in SSA approximates the minimum recommended number of ANC visits by the World Health Organization (WHO) [ 1 ], there were still disparities from region to region regarding the number of visits. This might have resulted from inequalities in the accessibility of maternal health services, poor/absence of transportation, inequality in the number of health care providers, and disparities in access to education [ 30 , 31 ]. In addition, this disparity might be due to the difference in the country’s policy and program implementation regarding maternal health service delivery, women’s education, and the role of women in household wealth status [ 32 ]. The other possible reason might be the difference in the implementation of different maternal and child health programs among regions of SSA.
In this study individual and community-level factors are responsible for approximately 64% of differences in the number of ANC visits during pregnancy in Sub-Saharan Africa. In the current study women aged 36–49 and 20–35 years were eighteen and eight percentage points more likely to visit health institutions for ANC service when compared to women aged 15–19 years. The finding supports other studies done previously in different countries [ 33 , 34 ] that showed a positive association between ANC visits and increased age of women. This might be due to birth-related complications and poor health conditions as age advances which trigger the women to demand more visits. In addition, it indicates that young women (15–19 years) probably lack experience in pregnancy care compared to older women [ 9 ].
Our finding also showed that women who had attained primary and secondary and above education were 26 and 44 percentage points more likely to have frequent ANC visits when compared with women with no education respectively. This finding is similar to other studies [ 16 , 35 – 38 ] conducted before in SSA as well as in other countries. This might be a result of the improvement in health literacy as the educational level increase [ 39 ].
Another factor that had a significant relationship with the frequency of ANC visits was whether the pregnancy was planned or not. The study indicated that unwanted pregnancy was 3 percentage points more likely to have a reduced frequency of ANC visits. The finding was consistent with the findings of other studies done before [ 38 , 40 – 42 ]. It is obvious that if the pregnancy was wanted women’s willingness to get health services would increase and there might be early detection of pregnancy, which in turn leads to early booking for ANC, as a result, the frequency of ANC visits would increase.
Furthermore, this study showed that the wealth status of the woman had a positive and significant effect on the frequency of ANC visits. Women from the middle and rich wealth quintiles were more likely to have a frequent number of ANC visits than women from the poor wealth quintile. This finding was consistent with the findings in other studies conducted in different countries [ 13 , 14 , 17 , 43 ]. This indicates that wealth status is an important variable that can influence the frequency of ANC visits. This could be because poor women can not afford transportation fees to a health facility for ANC service utilization. Besides, it can also affect the utilization of ANC services indirectly due to a lack of media exposure and access to education when compared to women with a high wealth status [ 44 , 45 ].
In this study, women’s exposure to mass media has a significant effect on the number of ANC visits. The result showed that women who had media exposure were more likely to have frequent ANC visits than their counterparts. This finding is consistent with previous research [ 9 , 11 , 17 ]. The possible explanation for this finding is that providing women with adequate information about maternal health services increases their utilization of such services. Parity is another factor that had a significant relationship with the frequency of ANC visits. According to our findings, primipara women were more likely to have frequent ANC visits than those with multiparity. In other words, the greater the women’s parity, the less likely they were to have frequent visits. This finding is supported by other previous studies [ 46 – 48 ]. This might be a result of increased confidence from previous birth experiences [ 37 , 49 – 51 ].
Women from rural residences were less likely to have frequent ANC visits. The result was consistent with the findings of studies conducted in different countries [ 44 , 45 , 52 ]. The possible explanation for this is the lack of health facilities in rural areas as compared to urban settings. Furthermore, rural women have no access to health-related information.
Moreover, the geographical region of SSA was found to be a significant factor that could affect the frequency of ANC visits. This study was in line with previously conducted studies [ 11 , 16 , 17 ]. This could be due to disparities in access to health facilities, transportation, and socioeconomic differences.
Our study revealed that women in middle-income countries were more likely to have frequent ANC visits than women in low-income countries. Although no similar study has been conducted, the possible explanations will be improved access to health services, and transportation as the income is higher. Regarding the DHS survey year, women surveyed from 2012–2015 and 2016–2019 were 5 and 7 percentage points more likely to have a greater number of visits than women surveyed from 2008–2011. This might be due to the advancement in the accessibility of health service infrastructures, and the increment in the number of health professionals from time to time.
The current study found that women from high-education communities were more likely to visit healthcare facilities during pregnancy than women from low-education communities. This finding is supported by another study [ 34 ]. This can be explained by herd health literacy where health-related information will be easily accessible in the community.
Women with a high level of media exposure are more likely to have ANC visits than women with a low level of media exposure. The explanation could be that access to the media is an enabling factor for ANC service utilization.
Strength and limitations
This study used large population-based data with a large sample size, which is representative of 35 sub–Saharan African countries. Furthermore, a count data analysis (multilevel Negative Binomial regression analysis) was applied which enabled us to model the effects of each determinant on the frequency of ANC visit efficiently. The novelty of this paper lies in the fact that we have modeled the determinants of the number of antenatal care services in SSA using the most recent DHS data for each country. One significant point of departure of this study is that some countries had no recent DHS data and data from some other countries are not publicly available. Despite the cross-sectional nature of the DHS data, reports of this finding are explained by the incidence rate ratio.
The mean number of ANC visits in SSA approximates the minimum recommended number of ANC visits by the WHO. Maternal education, maternal age above 20 years, media exposure, rich wealth status, high level of community education, high level of media exposure, country GDP, and being from the western and southern regions of SSA increased the frequency of ANC visits. On the other hand, rural residence, multiparity, and unplanned pregnancy negatively affected the frequency of ANC visits. Therefore, this study suggests that addressing geographical disparities and socio-economic inequalities will help alleviate the reduced utilization of ANC services.
Acknowledgments
The authors would like to thank the MEASURE DHS program for the on-request open access to its dataset.
- 1. WHO recommendation on antenatal care for positive pregnancy 27/02/21. Available from: https://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf .
- View Article
- PubMed/NCBI
- Google Scholar
- 3. Unicef for every child, Antenatal care 2021. Available from: https://data.unicef.org/topic/maternal-health/antenatal-care/ .
- 4. WHO, Causes of maternal and child deaths 24/02/21. Available from: https://www.who.int/pmnch/topics/child/countdownreportpages11-21.pdf .
- 5. World bank. Maternal and Child Mortality Development Goals 24/02/21. Available from: https://openknowledge.worldbank.org/handle/10986/17413 .
- 6. WHO. SUSTAINABLE DEVELOPMENT GOAL 3, Ensure healthy lives and promote well-being for all at all ages 2015. Available from: https://sdg-tracker.org/good-health .
- 7. Nation U. The Sustainable Development Goals Report. 2020.
- 10. Antenatal Care Module 03/03/21. Available from: https://www.open.edu/openlearncreate/mod/oucontent/view.php?id=44&print .
- 22. WHO, maternal health 24/02/21. Available from: https://www.afro.who.int/health-topics/maternal-health .
- 24. USAID. Guide to DHS Statistics, DHS-7 (version 2), The Demographic and Health Surveys Program. May 2020.
- 25. Parodi S, Bottarelli E. Poisson regression model in the epidemiology-an introduction [animal diseases]. Annali della Facoltà di Medicina Veterinaria-Università di Parma (Italy). 2006.
- Open access
- Published: 17 November 2021
Timing of first antenatal care visits and number of items of antenatal care contents received and associated factors in Ethiopia: multilevel mixed effects analysis
Zeitpunkt der ersten Besuche bei der Schwangerenvorsorge und Anzahl der erhaltenen Inhalte der Schwangerenvorsorge und damit verbundene Faktoren in Äthiopien: Mehrebenenanalyse mit gemischten Effekten
- Berhanu Teshome Woldeamanuel ORCID: orcid.org/0000-0002-1930-5432 1 &
- Tadesse Ayele Belachew 1
Reproductive Health volume 18 , Article number: 233 ( 2021 ) Cite this article
3623 Accesses
14 Citations
2 Altmetric
Metrics details
Receiving quality antenatal care (ANC) from skilled providers is essential to ensure the critical health circumstances of a pregnant woman and her child . Thus, this study attempted to assess which risk factors are significantly associated with the timing of antenatal care and the number of items of antenatal care content received from skilled providers in recent pregnancies among mothers in Ethiopia.
The data was extracted from the Ethiopian Demographic and Health Survey 2016. A total of 6645 mothers were included in the analysis. Multilevel mixed-effects logistic regression analysis and multilevel mixed Negative binomial models were fitted to find the factors associated with the timing and items of the content of ANC services. The 95% Confidence Interval of Odds Ratio/Incidence Rate Ratio, excluding one, was reported as significant.
About 20% of the mothers initiated ANC within the first trimester, and only 53% received at least four items of antenatal care content. Being rural residents (IRR = 0.82; 95%CI: 0.75–0.90), wanting no more children (IRR = 0.87; 95%CI: 0.79–0.96), and the husband being the sole decision maker of health care (IRR = 0.88; 95%CI: 0.81–0.96), were associated with reduced items of ANC content received. Further, birth order of six or more (IRR = 0.74; 95%CI: 0.56–0.96), rural residence (IRR = 0.0.41; 95%CI: 0.34–0.51), and wanting no more children (IRR = 0.61; 95%CI: 0.48–0.77) were associated with delayed antenatal care utilization.
Conclusions
Rural residences, the poorest household wealth status, no education level of mothers or partners, unexposed to mass media, unwanted pregnancy, mothers without decision-making power, and considerable distance to the nearest health facility have a significant impact on delaying the timing of ANC visits and reducing the number of items of ANC received in Ethiopia. Mothers should start an antenatal care visit early to ensure that a mother receives all of the necessary components of ANC treatment during her pregnancy.
Zusammenfassung
Hintergrund.
Eine qualitativ hochwertige Schwangerenvorsorge (ANC) durch qualifizierte Anbieter ist für die Sicherung der kritischen Gesundheitslage einer schwangeren Frau und ihres Kindes unerlässlich. In dieser Studie wurde daher untersucht, welche Risikofaktoren bei Müttern in Äthiopien in signifikantem Zusammenhang mit dem Zeitpunkt der Schwangerenvorsorge und der Anzahl der Inhalte der Schwangerenvorsorge stehen, die in den letzten Schwangerschaften von qualifizierten Anbietern durchgeführt wurden.
Die Daten wurden aus dem Ethiopian Demographic and Health Survey 2016 extrahiert. Insgesamt wurden 6645 Mütter in die Analyse einbezogen. Es wurden mehrstufige logistische Regressionsanalysen mit gemischten Effekten und mehrstufige gemischte negative Binomialmodelle verwendet, um die Faktoren zu ermitteln, die mit dem Zeitpunkt und den Inhalten der ANC-Leistungen in Verbindung stehen. Das 95%ige Konfidenzintervall der Odds Ratio/Inzidenzrate, mit Ausnahme von einem, wurde als signifikant angegeben.
Etwa 20% der Mütter begannen die ANC innerhalb des ersten Trimesters, und nur 53% erhielten mindestens vier Elemente der Schwangerenvorsorge. Die Tatsache, dass die Mütter auf dem Land wohnten (IRR = 0,82; 95%CI: 0,75–0,90), keine weiteren Kinder wollten (IRR = 0,87; 95%CI: 0,79–0,96) und der Ehemann der alleinige Entscheidungsträger für die Gesundheitsfürsorge war (IRR = 0,88; 95%CI: 0,81–0,96), war mit einer geringeren Anzahl an erhaltenen ANC-Inhalten verbunden. Außerdem waren die Reihenfolge der Geburten von sechs oder mehr (IRR = 0,74; 95%CI: 0,56–0,96), der Wohnsitz auf dem Land (IRR = 0,0,41; 95%CI: 0,34–0,51) und der Wunsch, keine weiteren Kinder zu bekommen (IRR = 0,61; 95%CI: 0,48–0,77) mit einer verzögerten Inanspruchnahme der Schwangerenvorsorge verbunden.
Schlussfolgerungen
Ländliche Wohnorte, der geringste Wohlstand des Haushalts, kein Bildungsniveau der Mütter oder Partner, keine Exposition gegenüber Massenmedien, ungewollte Schwangerschaft, Mütter ohne Entscheidungsbefugnis und eine große Entfernung zur nächsten Gesundheitseinrichtung haben in Äthiopien einen signifikanten Einfluss auf die Verzögerung von ANC-Besuchen und die Verringerung der Anzahl der erhaltenen ANC-Posten. Die Mütter sollten frühzeitig mit der Schwangerenvorsorge beginnen, um sicherzustellen, dass sie während ihrer Schwangerschaft alle notwendigen Bestandteile der ANC-Behandlung erhalten.
Plain language summary
The third Sustainable Development Goals prioritizes maternal mortality reduction, intending to lower the worldwide maternal mortality rate to 70 per 100,000 live births by 2030. Regular antenatal care from a skilled provider reduces maternal mortality by 20%. The overall quality of ANC service is determined collectively by the timing of ANC, and the contents of ANC received. Though there is an increase in ANC visits and the quality of services received, only 74% of women who gave birth in 2019 received antenatal care from a skilled provider, ranging from 85% in the urban to 70% in the rural. Thus, the quality and content of care might remain poor while the coverage of ANC visits is high. Therefore, it is necessary to analyze the levels and risk factors that affect the timing of ANC visits and contents to assess the quality of ANC services. This is the focus of the current study's research. In this study, nationally representative data from the 2016 Ethiopian Demographic and Health Survey was employed. Our study shows that rural residences, the poorest wealth quintile, no education level, unexposed to mass media, unwanted pregnancy, without decision-making power, and being far from the nearest health facility were found to be factors that hinder early initiation of ANC visits and reduce the number of items of ANC received. In conclusion, we ought to initiate an ANC visit early for a frequent antenatal care visit so that a mother will receive the necessary ANC components.
Peer Review reports
Introduction
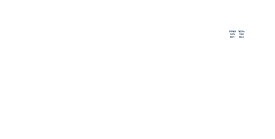
Maternal mortality reduction and enhancements in women’s health care are priorities of the third Sustainable Development Goal (SDGs) aimed to reduce the global maternal mortality ratio (MMR) to 70 per 100,000 live births by 2030 [ 1 ]. Between 2000 and 2017, the global maternal mortality rate (MMR) was reduced by 38% [ 2 ]. In Ethiopia, despite a 71.8% decline in MMR between 1990 and 2015, 1 in 64 women are at risk of dying from maternal-related causes, which is a big gap compared with MMR of 199 per 100, 000 live births plan 2020 [ 3 ]. It shows that more effort is needed to achieve the SGDs after ten years. Regular antenatal care from a skilled provider reduces maternal mortality by 20% [ 4 , 5 ]. According to the 2019 Ethiopian mini Demographic and Health Survey, 74% of women who gave birth in the five years before the survey received antenatal care (ANC) from a skilled provider, ranging from 85% in urban areas to 70% in rural areas [ 6 ]. Further, Ethiopia’s DHS 2016 revealed 75% of pregnant women had their blood pressure measured, 73% had a blood sample taken, 66% had a urine sample taken, and 66% received nutritional counseling during their ANC visits [ 7 ].
The use of health facilities is significantly associated with ANC visits, and sufficient ANC involves both the use of services and the sufficiency of the content within the services [ 8 , 9 ]. The 2016 Ethiopia DHS reports that only 20% of women had their first ANC visits in the first trimester, which calls for more ANC attendance [ 7 ]. Furthermore, concerning the type of skilled provider, doctors (5.7%), nurses/midwives (42%), health officers (1.4%), and health extension workers (13.2%) received ANC service.
Previous studies regarding antenatal care in Ethiopia and elsewhere recognized that women’s autonomy [ 10 , 11 , 12 ], birth order and the number of children born [ 13 , 14 , 15 ], husband’s attitude and support [ 10 , 16 ], lack of money [ 17 ] were the main reasons for lower health care utilization. Some studies reported that the education level of mother or husband/partner [ 10 , 11 , 12 , 13 , 15 , 17 , 18 , 19 , 20 ], age [ 10 , 11 , 14 , 19 ], woman’s occupation [ 10 , 17 ], place of residence [ 11 , 12 , 13 , 14 , 15 , 17 , 20 ], place of receiving [ 15 , 19 ], access to mass media [ 10 , 11 , 12 , 13 , 15 , 17 , 18 ], wealth quintile [ 10 , 11 , 12 , 13 , 14 , 15 , 17 , 18 , 19 ], and ANC provider [ 15 ] were the most important factors that affected the utilization of antenatal care services. According to the literature, wanted pregnancy [ 12 , 15 , 17 , 19 , 20 ], a lack of health care services such as a long distance to the health facility [ 10 , 17 , 19 ], health insurance [ 10 ], and permission to visit a health facility [ 17 ] were significant factors associated with antenatal care utilization and service quality.
The World Health Organization (WHO) recommends the first visit received before 12 weeks of pregnancy and the necessary contents of ANC visits to improve women’s care experience and reduce perinatal mortality [ 21 ]. Even though there is an increase in ANC visits and the quality of services received, many women are still not timely initiating the first ANC visit in Ethiopia. As a result, they have not received the critical contents of ANC. Though several studies in the past year in Ethiopia have explicitly examined associated factors of antenatal care utilization and completion of four or more visits during pregnancy [ 11 , 14 , 16 , 17 , 18 , 19 ], these studies did not investigate the actual number of components of ANC service a woman has received. Besides, these studies revealed that the contents of ANC visit highly influence the effectiveness of the ANC service. Thus, the quality and content of care might remain poor while the coverage of ANC visits is high. The overall quality of ANC service is determined collectively by the timing of ANC, and the contents of ANC received. Therefore, it is necessary to analyze the levels and risk factors that affect the timing of ANC visits and contents to assess the quality of ANC services. This is the focus of the current study's research.
Study setting, data and population
We used population based, nationally representative data from 2016 Ethiopian Demographic and Health Survey (DHS) [ 7 ]. The survey was conducted by the Central Statistical Agency (CSA) in collaboration with the Federal Ministry of Health (FMOH) and the Ethiopian Public Health Institute with technical assistance from ICF International and financial support from USAID, the government of the Netherlands, the World Bank, Irish Aid, and UNFPA from January 18, 2016, to June 27, 2016. The 2007 Ethiopia Population and Housing Census sampling frame with 84,915 enumeration areas (EAs), each EAs covering 181 households, was used. The respondents were selected using a stratified two-stage cluster design, each region stratified into urban and rural areas.
First was selecting 645 clusters (202 urban areas and 443 rural areas) with probability proportional to enumeration area size and independent selection within each stratum. In all the selected EAs, the household listing was done from September to December 2015. At the second stage, 28 households were selected per cluster with an equal probability systematic selection involving eligible women aged 15–49 years. Thus, a sample of 16,650 households and 15,683 women aged 15–49 years was identified with a response rate of 94.6%. Furthermore, details of the survey design and methodology have been reported in the 2016 EDHS [ 7 ].
Our analysis was based on the records of 6645 (54.3%) women who have complete information on the number of ANC visits, the timing of their first ANC visits, the contents of their ANC visits, and who gave birth in the five years preceding the survey. The latest deliveries were referred to all women.
This study has two response variables: Timing of first ANC visits; binary outcome categorized into 1 if a mother starts her first ANC visits within the first trimester (early initiation, or 12 weeks after the onset of pregnancy) and 0 elsewhere. Second, the contents of ANC received during pregnancy (a discrete outcome measured as the number of items WHO recommended and recognized as the contents of ANC) in Ethiopia received by a mother during pregnancy.
Standard guidelines for ANC in Ethiopia recognize that every pregnant woman should receive ANC from a skilled provider that consists of iron supplements, intestinal parasite drugs, at least two doses of Tetanus Toxoid injections, malaria intermittent preventive treatment in pregnancy, and health education on danger signs and complications during pregnancy; blood pressure measurement; urine tests; blood tests; health education on prevention of mother-to-child transmission of HIV/AIDS and HIV/AIDS counseling, testing, and collection of results. The composite index comprises a simple count of items received from skilled providers during the ANC visits. The variable had a minimum value of zero, indicating that the mother had not taken any items or received ANC. A maximum value of ten indicates that she has received all the nationally recommended and recognized content of the ANC. The important explanatory variables explored from previously available literature [ 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 ] are presented in Table 1 .
The wealth index was coded as: 1 = poorest, 2 = poorer, 3 = middle, 4 = richer, and 5 = richest. The wealth quintile of women’s households in EDHS is a composite indicator that scores were derived using principal component analysis based on housing characteristics and ownership of household durable goods [ 7 ]. National wealth quintiles are compiled by assigning the household score to each usual (de jure) household member, ranking each person in the household population by their score, and dividing the distribution into five equal categories, each comprising 20% of the population.
In EDHS 2016, birth order is a discrete variable ranging from 1 to 20. The proportion of birth orders two versus three and four versus five is nearly equal, so birth orders two and three and four and five were merged for this analysis. Further, the proportion of children with higher birth orders is relatively small, and birth orders of six and higher have been merged since the percentage distribution. The same categories were also used in the earlier study by Muchie [ 14 ]. Similarly, the percentage of women working in professional, technical, managerial, clerical, or unskilled manuals after screening for missing variables is too small, and the authors merge these two categories for this analysis. These too-few frequencies may, in turn, affect the parameter estimation.
Statistical methods of data analysis
Data analysis was done using the “R programming” version 4.0.3. Descriptive statistics of the subjects were summarized using frequency tables. A Chi-square test was performed to observe any association between the timing of the first ANC visit and the independent variables. An F-test based on analysis of variance (ANOVA) was used to examine the mean difference in the numbers of components of ANC received. Furthermore, the multilevel mixed-effects logistic regression was fitted to identify variables associated with the timing of first ANC visits. Meanwhile, multilevel mixed-effects count models were performed to identify factors associated with the number of ANC components received from a skilled provider during pregnancy.
First, a Poisson regression model with a log link was performed [ 22 ]. Then fitted Poisson regression checked for the problem of overdispersion (variance can be larger than the mean) or under dispersion (variance can be smaller than the mean) using the likelihood test. It was found that this test was significant. Therefore, the negative binomial (NB) regression model was considered the immediate solution for data analysis [ 23 ]. Moreover, the data experiencing excess zeros and overdispersion might be due to these excess zeros. Thus, we performed both the zero-inflated models (Zero Inflated Poisson and Zero Inflated Negative Binomial (ZINB)) and the Hurdle models (Hurdle Poisson (HP) and Hurdle Negative Binomial (HNB)) to check if overdispersion is accounted for due to excess zeros [ 24 ].
To account for the correlation between measurements (intra-cluster correlation (ICC)), we used the multilevel mixed-effects models (cluster/region-specific random effects). The use of a multilevel modeling approach accounts for the hierarchical nature of the EDHS data, where households were selected within EA clusters. There could be unobserved characteristics of cluster influencing women’s decision to timely initiate ANC and the number of ANC visits, such as the availability and accessibility of health services, cultural norms, and prevailing health beliefs. The outcomes of households within the same cluster are likely to correlate. Ignoring this correlation can underestimate variability (producing biased standard errors) and present falsely narrow confidence intervals [ 25 , 26 , 27 ].
Further, disregarding the hierarchical structure of the data and analyzing it as single-level data leads to incorrect inferences (i.e., high type I errors or loss of power) [ 28 ]. Finally, based on the Vuong statistic [ 29 ], likelihood ratio test, the Deviance, AIC, and BIC for model comparison, the multilevel mixed-effects negative binomial model best-fit factors associated with the number of items of ANC received from a skilled provider (see Additional file 1 ). Variables with a 95% confidence interval for the incidence risk ratio (IRR) excluding one were considered statistically significant determinants.
Socioeconomic and demographic characteristics of respondents
This study included 6645 women who had given birth within the five years preceding the survey. The background characteristics of women with respect to the timing of ANC visits are given in Table 2 . Most women (70.3%) were from rural areas, while only 29.7% were from urban areas. Concerning regions, a slightly higher percentage were from Tigray (14.6%), SNNPR (13.3%), Oromia (11.2%), and Amhara (10.7%), while the smallest percent of women were from Afar (6.1%), Gambela (6.8%), and Harari (6.8%). The median age was 27 years. Around 32% were from the richest, and 23% were from the poorest wealth quintile. The majority (49.5%) of women had no education, 32.8% had primary education, and only 6.6% had a higher education level. Regarding media access, only 2.8%, 16.3%, and 21.2% have read a newspaper or magazine, listened to the radio, and watched television at least once a week during their recent pregnancy.
On the other hand, concerning decision-making power over women’s health care, about two-thirds (65%) reported that both women and husbands/partners usually decide on respondents’ health care. Further, about 26% said they had a big problem getting permission to seek medical care, 50.1% had a big problem getting money for treatment in seeking medical care, and 44.2% had a far distance to a health facility in seeking medical care. In comparison, 33.7% reported a big problem in not wanting to go alone to seek medical care. In addition, the majority (80%) of women reported that their last child was wanted at the time of pregnancy. In comparison, 14.7% said the pregnancy was wanted later, and 5.3% reported they wanted no more.
Timing of first ANC visit by some characteristics of women
Only 20.1% of women started their ANC visit within the first trimester, with a median of four months for the first ANC visit. The proportion starting first ANC within the first trimester was lower in the SNNPR (22.2%), Benishangul-gumuz (23.1%), and Somali regions (32.1%), whereas it was higher in Dire Dawa (68.6%) and Addis Ababa (62.5%) cities. More than half (56.2%) of women from urban areas started their first ANC visit within the first trimester compared to 31.1% of rural women. Women who had higher levels of education (63.6%) and primary education (40%) started first ANC within the first trimester compared to uneducated women (31%). Further, women whose husbands/partners had higher education had the highest proportion (57%) of their first ANC visit within the first trimester.
The time to early initiate the first ANC visit was almost uniform among women’s age and occupation. The majority of women who read newspapers or magazines at least once a week (52%), who listen to the radio at least once a week (46%), and who watch television at least once a week (58%) started their ANC visits for their recent pregnancy within the first trimester. On the other hand, the proportion of women who began their first ANC visit within the first trimester increases with women’s autonomy concerning decisions about health care. Most women whose pregnancy was wanted (40%) started their first ANC visit within the first trimester and wanted no more children (25%). Moreover, 43% of women who had no problem getting money, 42.3% of women with a short distance to the nearest health facility, and 41% who had no difficulty going alone in seeking medical care had started their first ANC visit within the first trimester.
The number of items of ANC content received by some characteristics of mothers
Of all women who received ANC at least once, 79.9% had their blood pressure measured, 73.8% had a urine sample taken, and 79.5% had a blood sample taken. Further, 46.3% had been told about pregnancy complications, 45.4% received iron supplementation for at least 180 days, and 5.8% of women received treatment for an intestinal parasite. Additionally, 69.1% received counseling after testing AIDS, 53.7% were informed about birth preparedness, 67% received nutritional counseling, and 42.5% received two or more doses of tetanus toxoid vaccine from a skilled provider during their ANC visits (Fig. 1 ). The mean number of ANC contents received by a woman was 3.5 items and a standard deviation of 2.2, indicating that the distribution is overdispersed. Figure 2 presents a further detailed examination of the relationship between the frequency of ANC visits and the number of items of ANC contents received. It revealed that the likelihood of receiving the highest number of items of ANC content increases with the frequency of ANC visits. The proportion of women who received six items has monotonically increased from 4.2 to 37.3%, increasing ANC visits from one visit to at least five ANC visits (Fig. 2 ).
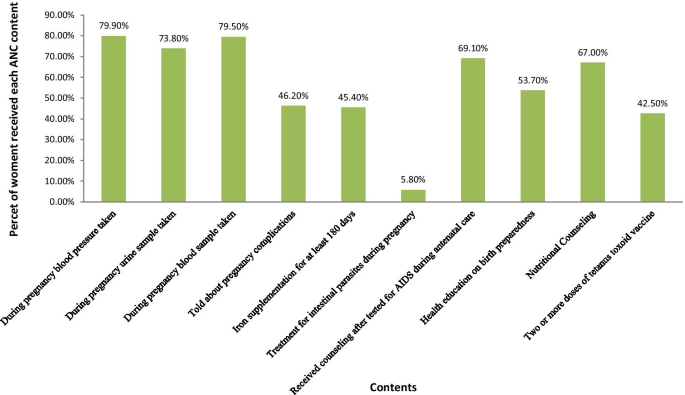
Types of items of ANC Contents received during pregnancy in Ethiopia, EDHS 2016, n = 6645
Percentage distribution of number of items of ANC contents received by frequency of ANC visits in Ethiopia, EDHS 2016
Conversely, the pattern showed a declining trend of the likelihood of receiving only one item or two items, or three items, with an increase in the number of ANC visits. In addition, the timing of the first ANC visit showed a positive association with the mean number of items of ANC contents received. For instance, a woman who started her first ANC visit within the first trimester received, on average, 6.2 items. In comparison, women who had received only one ANC visit had received an average of 3.8 items, compared to virtually six items on average among women with four or more ANC visits (Table 3 ).
Factors associated with the timing of the first ANC visits: multilevel mixed-effects logistic regression analysis
The multivariable multilevel logistic regression analysis of factors associated with the timing of the first ANC visit is given in Table 4 . The likelihood of timely initiating the first ANC visit was lower among six or more birth orders (AOR = 0.74; 95%CI: 0.56–0.96) than the first birth order. Moreover, rural women were 59% less likely to start their first ANC visit within the first trimester (AOR = 0.41; 95%CI: 0.31–0.54) than urban counterparts.
The log odds of timely initiating the first ANC visit were higher among the richest wealth quintile (AOR = 2.17; 95%CI: 1.61–2.92), the 4 th (AOR = 2.29; 95%CI: 1.87–2.81), and the 3 rd (AOR = 2.02; 95%CI: 1.68–2.42) wealth quintile, respectively, as compared to the poorest wealth quintile. The odds of starting the first ANC visit within the first trimester was 5.2 times (AOR = 5.20; 95%CI: 2.25–12.03), 2.14 times (AOR = 2.14; 95%CI: 1.50–3.06) and 1.73 times (AOR = 1.73; 95%CI: 148–2.02), higher among women with a higher, secondary and primary level of education, respectively, as compared to uneducated women after controlling for other variables in the model. Similarly, women whose husbands had higher education levels were 45% (AOR = 1.45; 95%CI: 1.08–1.95) more likely to start their ANC within the first trimester than those whose husbands had not been educated. Women aged 40–44 years old were 34% (AOR = 0.66; 95%CI: 0.44–0.99) less likely to start their first ANC visit on time than women aged 15–19 years old.
Furthermore, women who listened to the radio less than once a week (AOR = 1.56; 95%CI: 1.25–1.93), at least once a week (AOR = 1.49; 95%CI: 1.20–1.85) and watched television at least once a week (AOR = 1.58; 95%CI: 1.11–2.23), respectively, were more likely than those who did not listen to the radio or watch television to start their first ANC in the first trimester. Pregnant women who want no more children were 39% (AOR = 0.61; 95%CI: 0.48–0.77) less likely to start their first ANC visit within the first trimester than those whose pregnancies were wanted. Furthermore, a woman who reported a short distance to a health facility seeking medical care was 55% (AOR = 1.55; 95%CI: 1.35–1.78) more likely to start her first ANC visit within the first trimester (Table 4 ).
Factors associated with the number of ANC content items received by a woman: Multilevel mixed-effects Negative binomial analysis
The estimated incidence rate ratio (IRR) indicates that women from rural areas (IRR = 0.82; 95%CI: 0.75–0.90) and female heads (IRR = 0.91; 95%CI: 0.85–0.97) were significantly associated with lower numbers of items of ANC content received. Further, women who wanted no more children (IRR = 0.87; 95%CI: 0.79–0.96), whose husbands/partners decided alone, were significantly associated with lower numbers of items of ANC content received. In contrast, women from the richest wealth quintile (IRR = 1.51; 95%CI: 1.36–1.67), 4 th wealth quintile (IRR = 1.62; 95%CI: 1.49–1.75) and 3 rd wealth quintile (IRR = 1.47; 95%CI: 1.37–1.59), women who had primary education (IRR = 1.24; 95%CI: 1.17–1.32), secondary education (IRR: 1.22, CI: 1.10–1.34) and higher education (IRR = 1.21; 95%CI: 1.05–1.39) as well as women whose partners had primary education (IRR = 1.17; 95%CI: 1.01–1.24), secondary education (IRR = 1.21; 95%CI: 1.11–1.34) and higher education (IRR = 1.16; 95%CI: 1.04–1.30) were more likely to receive a higher number of items of ANC contents. Additionally, women who have no problem of getting permission (IRR = 1.10; 95%CI: 1.03–1.17), who reported short distance to health facilities (IRR = 1.19; 95%CI: 1.12–1.26), who listen to the radio less than once a week (IRR = 1.12; 95%CI: 1.04–1.19) and at least once a week (IRR = 1.15; 95%CI: 1.07–1.23), who watch television less than once a week (IRR = 1.09; 95%CI: 1.01–1.19), who had received 1–3 ANC (IRR = 5.12; 95%CI: 4.68–5.59) and at least four ANC (IRR = 6.08; 95%CI: 5.56–6.65) from a skilled provider were significantly more likely to have a higher number of items of ANC contents during their pregnancy.
The study found that 53% of women received at least four ANC items, while 20% started their first ANC visit within the first trimester. The multilevel negative binomial regression analysis revealed that the covariates of rural residents and an unwanted child at the time of pregnancy were significantly associated with the lower incidence rate ratio of the number of ANC contents received. Further, the frequency of ANC visits during pregnancy was significantly associated with a higher incidence rate ratio of ANC contents received. In contrast, female heads were significantly associated with a lower incidence rate ratio of ANC contents received. The multilevel logistic regression analysis revealed that having six or more birth orders, living in a rural area, being between the ages of 40 and 44, and wanting no more children were all significantly associated with a lower likelihood of initiating ANC visits on time. Higher wealth quintile, higher education level of women and partners, access to mass media, and a short distance to the health facility in seeking medical care, on the other hand, were significantly associated with increased odds of initiating an ANC visit for a recent pregnancy within the last five years before the survey.
This study showed that higher birth order was inversely associated with the timing of the ANC visit, i.e., women were less likely to start their ANC visit within the first trimester of their sixth or higher birth order. A similar study in Uganda [ 30 ] found mothers with third birth orders, compared to those with the first, are about 6–7% less likely to attain the four antenatal visits, and mothers with at least the third birth order are 4–5% less likely to initiate the first visit in the first trimester. Muchie [ 14 ], using Ethiopian Mini DHS 2014, also found 38 and 36% lower odds of completing four or more visits of ANC utilization for birth orders of children four or five, and six or more, respectively. One possible reason for this might be mainly in the first pregnancy when women wanted lots of contact with their care provider. Some women would have liked more communication between appointments and were worried about having to deal with pregnancy complications and pain.
Rural mothers are less likely to receive higher ANC content from skilled providers and start ANC visits within the first trimester than urban mothers. This finding is congruent with that of Beeckman et al. [ 10 ], who reported higher odds of delaying first ANC visits and ANC visits of less than four among rural mothers. Further, a study done in Bangladesh, [ 12 ] found rural mothers are 17% less likely to attend a higher number of ANC visits than urban mothers. Another similar finding from Bangladesh [ 8 ] reported that urban mothers were 1.35 times more likely to receive more items of ANC services from a skilled provider than their rural counterparts. In Ethiopia’s rural areas, there is a lack of skilled health care providers, lack of information on antenatal care services, lack of infrastructure, and long distances from health facilities.
Moreover, most mothers in rural Ethiopia were uneducated. Contrary to our findings, Gebremeskel et al. [ 31 ] and Weldearegawi et al. [ 32 ] reported residence was not associated with the timing of the first ANC visit. This inconsistency might be due to the statistical methodology used and the smaller sample size used by Gebremeskel et al. [ 31 ] (n = 409) and Weldearegawi et al. [ 32 ] ( n = 402), whereas the EDHS 2016 used (n = 6645).
Furthermore, we found that women with at least primary education levels are more likely to start the first ANC visit within the first trimester and receive the highest number of items of ANC content from skilled providers. Similarly, women whose partners had at least a primary education were more likely to receive higher ANC content from skilled providers than the uneducated category. Additionally, women whose partners had higher education were more likely to start ANC visits within the first trimester than those without. Further analysis of the 2011 Ethiopian DHS showed that women who had primary education (79%), secondary education (62%), and higher education were 45% times less likely to delay their first ANC visit [ 10 ]. Consistent with our finding, Islam [ 8 ] also found that there is a 1.12, 1.26, and 1.39 incidence rate ratio of receiving higher numbers of ANC content among women having primary, secondary, and higher education in Bangladesh. But, partners’ primary education level has not significantly increased the incidence of receiving the items of ANC content. In contrast, partners having a secondary or higher education significantly increased the incidence of receiving the items of ANC content [ 8 ].
In contrast, in Ghana, Manyeh et al. [ 33 ] found no significant effect of husband/partner education level on the timing of ANC visits. Additionally, a systematic review analysis in sub-Saharan Arica found that husband education was significantly associated with uptake, frequency, and timing of first ANC visits [ 10 ]. Most likely, this could be because educated women have more access to information and make their own decisions on their health care, which empowered them to exercise, and changed traditional attitudes about using the ANC service. This study suggests that there is an urgent need to focus on mothers’ education. Advocating primary education for girls and encouraging them to pursue secondary or higher education is essential to achieve a tangible change to achieve the sustainable development goals of maternal and infant mortality reduction through effective implementation of maternal health care services [ 14 , 34 ].
The result also suggests women who listened to the radio and watched television at least once a week were more likely to start their first ANC early and received more items of ANC content from skilled providers. This result agrees with the findings of Yaya et al. [ 11 ], where women who watch television at least once a week were 40% less likely to delay their first ANC visit than those who do not watch television at all. But they did not find an association between listening to the radio and the timing of the first antenatal care visit. This variation might be due to a difference in the methodology used. In Bangladesh [ 8 , 12 ], mass media access was associated with increased ANC content received.
Women whose pregnancies were unwanted or wanted later were more likely to delay their first ANC visit and less likely to receive the highest number of ANC content items than wanted pregnancies. A similar study of the Bangladeshi DHS found that wanted pregnancy was associated with a higher incidence of receiving higher items of ANC contents [ 8 ]. Another study from Bangladesh [ 12 ], Southern Ethiopia [ 31 ], Bahir Dar [ 35 ], and Eastern Tigray [ 32 ] found unwanted pregnancy significantly associated with delayed initiation of ANC service utilization. This might be that mothers with unwanted pregnancies have anxiety and poor psychological well-being [ 36 ] and less attention to pregnancy-related complications, and do not use supplements such as folic acid, vaccinations, health information, and nutritional counseling [ 37 ]. Thus, women ought to be encouraged to use modern contraceptives to prevent unwanted pregnancies.
Furthermore, women’s health decision-making power is significantly associated with the content of ANC services received. Women without decision-making power or whose husband/partner alone decides on their health care are strongly associated with lower ANC contents received. This result was congruent with those of northwest Ethiopia [ 38 ], Bangladesh [ 12 ], the systematic review of sub-Saharan Africa [ 10 ], and Tanzania [ 39 ]. However, unlike our findings, Gebresilassie et al. [ 40 ] found that decision-making on self-care seeking was not significantly associated with the timing of the first ANC visit.
Mothers with a shorter distance to the nearest health facility had better odds of initiating their first ANC visit and receiving items of ANC content from skilled providers. Similar findings are reported in a study in Bahir Dar, Ethiopia [ 35 ]. In the Eastern Tigray zone in Northern Ethiopia, distance to the nearest health facility was not a significant predictor of late antenatal care follow-up [ 32 ] . In Rwanda, distance to the health facility was not a significant predictor of poor quality of antenatal utilization [ 41 ]. Likewise, mothers who had permission to seek medical care were more likely to receive more ANC content.
Lastly, the results indicated that the frequency of ANC visits and timing of the first ANC visit during pregnancy was positively associated with the number of items of ANC contents a woman received from a skilled provider. Women who started antenatal care within the first trimester were more likely to receive more ANC contents items than those who delayed their visit. Likewise, the number of items of ANC content monotonically increases with frequent ANC visits. The findings are consistent with those of [ 42 , 43 ].
Findings of this study suggest that rural residences, the poorest wealth quintile, no education level of mothers or partners, unexposed to mass media, unwanted pregnancy, mothers without decision-making power, and a long distance to the nearest health facility have significant impacts on delaying the timing of ANC visits and reducing the number of items of ANC received in Ethiopia. Further, timely initiation of the ANC and the number of ANC visits were significantly associated with the increase in the number of items ANC received during pregnancy. Therefore, this study recommends that women initiate ANC visits timely and frequent antenatal care visits during pregnancy for the quality of ANC received from a skilled provider. Another implication of this study is that educating and empowering girls, particularly in the rural areas, are vital ingredients in all policies aiming to reduce maternal and neonatal deaths through improved quality of antenatal care utilization, particularly in the rural areas. Furthermore, encouraging women to use modern contraceptives, expanding health education in the media, and expanding health facilities are vital inputs that should be included in policies to improve the quality of antennal care utilization, particularly in rural areas. Moreover, women at low economic levels should be given special emphasis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Antenatal care
Confidence interval
Central Statistics Agency
Demographic and Health Survey
Ethiopia Demographic and Health Survey
Enumeration areas
Federal Ministry of Health
Hurdle Poisson
Hurdle negative binomial
Incidence rate ratio
Likelihood ratio test
Maternal Mortality Ratio
Negative Binomial
Sustainable Development Goals
United Nations Population Fund
United States Agency for International Development
World Health Organization
Zero Inflated Poisson
Zero Inflated Negative Binomial
United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. New York: United Nations; 2015. https://sustainabledevelopment.un.org/.pdf
WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division. Trends in maternal mortality: 2000 to 2017. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division; World Health Organization. Geneva: WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division; 2019. https://www.unfpa.org/featured-publication/trends-maternal-mortality-2000-2017 .
Ministry of Health (MOH), Health Sector Transformation plan, 2015/16–2019/20. Addis Ababa, Ethiopia: MOH; 2015 https://www.worldcat.org/title/hstp-health-sector-transformation-plan-201516-201920-2008-2012-efy .
Testa J, OueÂdraogo C, Prual A, et al. Determinants of risk factors associated with severe maternal morbidity: application during antenatal consultations. J GyneÂcol Obste t Biol Reprod (Paris). 2002;31:44–50.
CAS Google Scholar
Prual A, et al. The quality of risk factor screening during antenatal consultations in Niger. Health Policy Planning. 2000;15(1):11–6.
Article CAS Google Scholar
Central Statistical Agency. Ethiopia Mini Demographic and Health survey 2019. Addis Ababa, Ethiopia: Central Statistics Agency; 2019. https://www.unicef.org/ethiopia/Mini/Demographic/and/Health/Survey.pdf
Central Statistics Agency (CSA) [Ethiopia] and ICF International. Ethiopia demographic and health survey 2016. Addis Ababa and Rockville: Central Statistical Agency (CSA) and ICF International; 2016. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf .
Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the WHO recommendations. PLoS ONE. 2018;13(9):e0204752.
Article Google Scholar
Beeckman K, et al. The development and application of a new tool to assess the adequacy of the content and timing of antenatal care. BMC Health Serv Res. 2011;11(1):213.
Okedo-Alex IN, Akamike IC, Ezeanosike OB, et al. Determinants of antenatal care utilization in sub-Saharan Africa: a systematic review. BMJ Open. 2019;9(10):e031890.
Yaya S, et al. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS ONE. 2017;12(9):e0184934.
Bhowmik KR, Das S, Islam MA. Modelling the number of antenatal care visits in Bangladesh to determine the risk factors for reduced antenatal care attendance. PLoS ONE. 2020;15(1):e0228215.
Adhikari M, et al. Sociodemographic correlates of antenatal care visits in Nepal: results from Nepal Demographic and Health Survey 2016. BMC Pregn Childbirth. 2020;20:513.
Kindie Fentahun Muchie. Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: a finding based on a demographic and health survey. BMC Pregn Childbirth. 2017;17:300.
Birmeta K, Dibaba Y, Woldeyohannes D. Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC Health Serv Res. 2013;13:256.
Mekonnen T, et al. Trends and determinants of antenatal care service use in Ethiopia between 2000 and 2016. Int J Environ Res Public Health. 2019;16:748.
Tsegaye B, Ayalew M. Prevalence and factors associated with antenatal care utilization in Ethiopia: an evidence from demographic health survey 2016. BMC Pregn Childbirth. 2020;20:528.
Tegegne TK, et al. Antenatal care use in Ethiopia: a spatial and multilevel analysis. Pregn Childbirth. 2019;19:399.
Tiruaynet K, Muchie KF. Determinants of utilization of antenatal care services in Benishangul Gumuz Region, Western Ethiopia: a study based on demographic and health survey. BMC Pregn Childbirth. 2019;19:115.
Ochako R, Gichuhi W. Pregnancy wantedness, frequency and timing of antenatal care visit among women of childbearing age in Kenya. Reprod Health. 2016;13:51.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: WHO; 2016. http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf .
McCullagh P, Nelder JA. Generalized Linear Models. 2nd ed. London: Chapman and Hall; 1986.
Google Scholar
Cameron AC, Trivedi PK. Essentials of count data regression. A companion to theoretical econometrics. 2001; 331.
Cameron AC, Trivedi PK. Regression analysis of count data. 2nd edition, Econometric Society Monograph. No. 53. Cambridge: Cambridge University Press; 2013.
Book Google Scholar
Goldstein H. Multilevel statistical models. London: Edward Arnold; 1995.
Domnner A, Klar N. Design and analysis of cluster randomization trials in health research. London: Arnold; 2000.
Klar N. A practical guide to cluster randomized trials in health services research. J Biopharm Stat. 2013;23:711–3.
Austin PC, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. 2017;36(20):3257–77.
Voung QH. Likelihood ratio test for model selection and non-nested hypothesis. Econometrica. 1989;57(2):307–33.
Bbaale E. Factors influencing timing and frequency of antenatal care in Uganda. Australian Medical Journal. 2011;4(8):431–8.
Gebrehiwot GW, et al. Determinants of late antenatal care follow up among pregnant women in Easter zone Tigray, Northern Ethiopia, 2018: unmatched case–control study. BMC Res Notes. 2019;12:752.
Gebremeskel F, Dibaba Y, Admassu B. Timing of first antenatal care attendance and associated factors among pregnant women in Arba Minch Town and Arba Minch District, Gamo Gofa Zone, South Ethiopia. J Environ Public Health. 2015;2015:971506.
Manyeh AK, et al. Factors associated with the timing of antenatal clinic attendance among firsttime mothers in rural Southern Ghana. BMC Pregn Childbirth. 2020;20:47.
Warri D, George A. Perceptions of pregnant women of reasons for late initiation of antenatal care: a qualitative interview study. BMC Pregn Childbirth. 2020;20:70.
Alemu Y, Aragaw A. Early initiations of first antenatal care visit and associated factor among mothers who gave birth in the last six months preceding birth in Bahir Dar Zuria Woreda North West Ethiopia. Reprod Health. 2018;15:203.
Gupta S, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS ONE. 2014;9(7):e101893.
Stern J, et al. Is pregnancy planning associated with background characteristics and pregnancy planning behavior? Acta Obstet Gynecol Scand. 2016;95(2):182–9.
Gudayu TW, Woldeyohannes SM, Abdo AA. Timing and factors associated with first antenatal care booking among pregnant mothers in Gondar Town; North West Ethiopia. BMC Pregn Childbirth. 2014;14:287.
Abdon GR, et al. Trends and factors associated with the utilisation of antenatal care services during the Millennium Development Goals era in Tanzania. Trop Med Health. 2020;48:38.
Gebresilassie B, et al. Timing of first antenatal care attendance and associated factors among pregnant women in public health institutions of Axum town, Tigray, Ethiopia, 2017: a mixed design study. BMC Pregn Childbirth. 2019;19:340.
Rurangirwa AA, et al. Determinants of poor utilization of antenatal care services among recently delivered women in Rwanda; a population based study. BMC Pregn Childbirth. 2017;17:142.
Mihret MS, Limenih MA, Gudayu TW. The role of timely initiation of antenatal care on protective dose tetanus toxoid immunization: the case of northern Ethiopia post natal mothers. BMC Pregn Childbirth. 2018;18:235.
Agha S, Tappis H. The timing of antenatal care initiation and the content of care in Sindh Pakistan. BMC Pregn Childbirth. 2016;16:190.
Download references
Acknowledgements
We are grateful to ICF macro (Calverton, USA) for providing the 2016 DHS data of Ethiopia.
Declaration
The authors declare that the research is our original work, and all sources of materials used have been duly acknowledged.
The author has no support or funding to report.
Author information
Authors and affiliations.
Salale University, Fitche, Oromiya, Ethiopia
Berhanu Teshome Woldeamanuel & Tadesse Ayele Belachew
You can also search for this author in PubMed Google Scholar
Contributions
TAB involved from the inception to design, acquisition of data, analysis and interpretation, drafting the manuscript, BT involved from the inception to design, acquisition of data, analysis and interpretation and drafting the manuscript and editing the manuscript for the final submission. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Berhanu Teshome Woldeamanuel .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for this study was not required since the data is secondary and is available in the public domain. Anyone can download datasets after registering as a DHS data user at https://dhsprogram.com/data/new-user-registration.cfm .
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table s1..
AIC, BIC, Log-likelihood and Deviance based Model comparison for mixed effects models. Table S2. Vuong Tests for the non-nested models Poisson, negative-binomial (NB), zero-inflated Poisson (ZIP), hurdle Poisson (HP), zeroinflated NB (ZINB), and hurdle NB (HNB) models. Table S3. Akaike’s information criteria (AIC), log-likelihood, and likelihood-ratio for Poisson, negative-binomial regression (NB), mixed Poison (MP) and Mixed NBR (MNBR) models.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Woldeamanuel, B.T., Belachew, T.A. Timing of first antenatal care visits and number of items of antenatal care contents received and associated factors in Ethiopia: multilevel mixed effects analysis. Reprod Health 18 , 233 (2021). https://doi.org/10.1186/s12978-021-01275-9
Download citation
Received : 02 July 2021
Accepted : 25 October 2021
Published : 17 November 2021
DOI : https://doi.org/10.1186/s12978-021-01275-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Contents of antenatal care
- Timing of antenatal care

Schlüsselwörter
- Schwangerenvorsorge
- Inhalte der Schwangerenvorsorge
- Zeitplan der Schwangerenvorsorge
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
- Open access
- Published: 12 October 2024
Compliance with the 2016 WHO’s antenatal care recommendation and its determinants among women in Sub-Saharan Africa: a multilevel-analysis of population survey data
- Kusse Urmale Mare 1 ,
- Kebede Gemeda Sabo 1 ,
- Yordanos Sisay Asgedom 2 ,
- Zufan Alamrie Asmare 3 ,
- Tsion Mulat Tebeje 4 ,
- Abdu Hailu Shibeshi 5 ,
- Afework Alemu Lombebo 6 ,
- Bezawit Melak Fente 7 ,
- Bizunesh Fantahun Kase 8 ,
- Hiwot Altaye Asebe 8 &
- Beminate Lemma Seifu 8
BMC Health Services Research volume 24 , Article number: 1223 ( 2024 ) Cite this article
Metrics details
Despite the positive impact of adhering to the new antenatal care model on pregnancy outcomes and maternal health service uptake, women in resource-limited settings exhibit low levels of compliance with this recommendation. Previous studies on women’s adherence to the new antenatal care recommendation have been limited to individual countries, with no evidence available at Sub-Saharan Africa (SSA) level. Therefore, this study sought to investigate compliance with the 2016 WHO’s recommendation of at least eight antenatal care contacts among women in SSA countries and identify its determinants.
The study utilized a weighted sample of 101,983 women who had received antenatal care during their index pregnancy, drawn from recent DHS data of sixteen SSA countries. A multilevel mixed-effect analysis was conducted to identify factors that influence compliance with new antenatal care recommendations. Model comparison was performed using deviance and log-likelihood values, and statistical significance was determined at a P -value of less than 0.05.
The level of compliance with the recommended antenatal care contacts among women in SSA was 9.9% (95% CI: 9.7-10.1%), with the highest rate in Sierra Leone (26.1%) and lowest in Rwanda (< 1%). A multivariable logistic regression analysis showed that age, education, employment status, household wealth, healthcare decisions, the timing of antenatal contacts, consumption of nutritional supplements, residence, community-level women illiteracy, and media exposure were the significant determinants of compliance.
Only one in ten pregnant women in SSA countries had attended the recommended number of antenatal contacts, with Sierra Leone having the highest compliance rate and Rwanda and Senegal having the lowest. Therefore, policymakers should focus on improving access to education, especially for women and their partners, and providing exempted services for pregnant women from low-income households. Interventions that target communities with low levels of literacy and media exposure could also be effective in improving the uptake of the services.
Peer Review reports
According to the 2023 estimate, about 287,000 mothers died due to pregnancy and childbirth complications and the majority (95%) of these deaths occurred in low- and middle-income countries, with sub-Saharan Africa (SSA) accounting for 70% of deaths [ 1 ]. Although evidence has underlined the significance of maternal health interventions in reducing maternal mortality and pregnancy and birth complications, only one-quarter of women in SSA optimally used these services [ 2 ]. A secondary analysis of demographic and health survey (DHS) data showed that utilization of antenatal, skilled childbirth, and postnatal care among young women in SSA was 55%, 79%, and 40%, respectively [ 3 ].
Quality antenatal care (ANC) during play a crucial role in significantly reducing the risk of morbidity and mortality for both the mother and the child [ 4 ]. In 2016, the World Health Organization (WHO) introduced an updated ANC model, covering five essential areas: routine antenatal nutrition, maternal and fetal assessment, preventive measures, interventions for managing common pregnancy-related symptoms, and health system-level strategies intended to enhance the accessibility and quality of ANC [ 5 ]. According to this recommendation, pregnant women should attend a minimum of eight contacts, with one, two, and five contacts scheduled during the three consecutive trimesters, respectively. The main rationale for increasing antenatal care contacts from four contacts to at least eight in 2016 was to improve prenatal outcomes and increase maternal satisfaction throughout the subsequent care [ 5 , 6 ]
Studies conducted in different settings have examined women’s compliance with WHO’s new antenatal care recommendation. Accordingly, it was found that the level of compliance with the recommendation in Bangladesh [ 7 ] and Myanmar [ 8 ] was 6% and 18%, respectively. In Africa, the coverage varied from 31% [ 9 ] to 42% in Ghana [ 10 ], 28% in Cameroon [ 11 ] 25% in Sierra Leone [ 12 ], 2.5% in Ethiopia [ 13 ], and 17% in Nigeria [ 14 ]. Furthermore, studies have unveiled diverse factors that have been found to influence women’s adherence to the updated WHO antenatal care contacts. These include age [ 12 ], enrollment in health insurance and women’s education [ 12 , 15 ], wealth index [ 7 , 8 , 16 , 17 , 18 ], educational attainment [ 12 , 14 , 16 , 17 , 18 ], parity [ 7 , 12 ]), media exposure [ 7 , 14 , 16 ]), frequency of ANC contacts, place of residence, consultation with health care provider, and planned pregnancy [ 7 ], initiation month/time of ANC [ 8 , 14 ]), quality of antenatal care and women’s employment status [ 17 ], and distance to health facilities and associated costs [ 16 ]. These variables have been documented as significant influencers impacting women’s adherence to the newly recommended WHO antenatal care contacts.
Globally, efforts have been made to reduce maternal and child complications associated with pregnancy. These efforts include the implementation of the focused antenatal care model in 2002 [ 19 ] and the introduction of a newly recommended antenatal care model in 2016, which was endorsed by the World Health Organization [ 5 ]. The revised ANC model has been reported to be more effective in reducing infant morbidity and mortality [ 20 , 21 , 22 ], lowering perinatal death and stillbirth rates [ 23 , 24 , 25 ], facilitating early detection and prevention of adverse pregnancy-related outcomes [ 12 , 23 ], and promoting institutional deliveries and the utilization of postnatal care services [ 26 ].
However, despite the positive outcomes of measures taken by the WHO [ 12 , 20 , 21 , 22 , 23 , 24 , 25 , 26 ], evidence shows that women from developing countries still struggle to adhere to recommended ANC contacts due to cultural barriers, lack of knowledge, and limited accessibility and associated costs [ 7 , 16 ]. Consequently, many women continue to experience pregnancy and childbirth complications leading to mortality [ 27 , 28 ]. Furthermore, existing studies assessing women’s adherence to newly recommended ANC contacts were either specific to a single country [ 8 , 11 , 13 , 14 , 18 , 29 ] or included only a few countries [ 12 ]. Therefore, this study aims to examine women’s compliance with the newly recommended WHO ANC model and its determinants in SSA countries.
Data source and participants
This study utilized data from the recent DHS conducted in 16 SSA between 2017 and 2022. The selection of these countries was based on the availability of a standardized and unrestricted DHS dataset that contained the outcome and necessary explanatory variables. DHS is a nationally representative survey conducted every five years to collect data on basic sociodemographic characteristics and various health indicators. The surveys in all countries utilized a standardized methodology and a two-stage stratified cluster sampling technique to select study participants. In the first stage, enumeration areas were randomly selected based on recent population data, and households were randomly selected in the second stage using the housing census as a sampling frame. For the final analysis, a total weighted sample of 101,983 women of reproductive age who had attended antenatal care during their index pregnancy was considered. Further information regarding the countries and sample sizes included in the analysis is presented below (Table 1 ).
Dependent variable
This study defined the dependent variable as compliance with the WHO’s updated antenatal care guidelines. This was assessed by determining the number of antenatal care contacts attended during the most recent pregnancy. Women who attended a minimum of eight contacts were classified as being compliant with the recommendation, while those who attended fewer than eight contacts were classified as non-compliant.
Independent variables
Individual-level variables were grouped into sociodemographic and obstetric variables. Socio-demographic variables included current age, marital status, woman’s and partner’s education, women’s employment status, media exposure, household head, wealth index, coverage by health insurance, and family size. Obstetric variables were age at marriage, number of under-5 children, birth order, birth interval, timing of ANC, decision on health care, use of iron supplements, and history of pregnancy loss. While, residence, community-level media exposure, and community-level women illiteracy were the community-level variables.
Exposure to mass media was computed using three variables (frequency of watching television, listening to the radio, and reading newspapers) that have three response options (i.e. not at all, less than once a week, and at least once a week). Thus, women who reported watching television, listening to the radio, or reading the newspaper at least once a week were considered as having media exposure and otherwise labeled as not having exposure to mass media.
Other community-level variables (i.e. community-level women illiteracy and media exposure) were generated by aggregating the individual-level observations at the cluster level and the aggregates were computed using the average values of the proportions of women in each category of a given variable and median values were used to categorize the aggregated variables into two groups (i.e. low and high).
Data management and statistical analysis
Stata software version 17 was used for data cleaning and analysis. Before analysis, the availability of the outcome variable in the DHS dataset of each country was confirmed and all variables considered in the study were checked for missing values. Then, the datasets of 16 SSA countries were appended and sample weight was applied to compensate for the non-representativeness of the sample and obtain reliable estimates and standard errors.
To account for the clustering effects, a multilevel logistic regression analysis was applied to determine the effects of independent variables on women’s compliance with the recommended antenatal care contacts. Bivariable multilevel logistic regression analysis was done and all variables with a p-value of less than 0.25 in this analysis were considered for multivariable multilevel logistic regression analysis.
In our analysis, four models were fitted to select the model that best fits the data: model I (a model without independent variables to test random variability in the intercept), model II (a model with only community-level variables), model III (a model with individual-level variables), and model IV (a model with both individual and community-level predictor variables). Then, log-likelihood (LL) and deviance (i.e. -2*LL) values were used for model selection and the model with the lowest deviance and highest LL values was considered as a best-fitted model for the final analysis. The presence of multi-collinearity between explanatory variables was checked using generalized variance inflation factor values and this value was less than five for all variables, suggesting the non-existence of multi-collinearity. Finally, in the multivariable analysis, a p-value less than 0.05 and an adjusted odds ratio with the corresponding 95% confidence interval were used to identify the factors associated with compliance with antenatal care recommendations. Moreover, the random variability in the level of compliance across clusters was estimated by intra-class correlation coefficient (ICC), proportion change in variance (PCV), and median odds ratio (MOR).
Ethical approval
Data used in this study were obtained from a demographic and health survey, and permission to access it was granted through an online request process available at http://www.dhsprogram.com . The accessed data were solely utilized for this registered study and can be publicly accessed from the program’s official database.
Socio-demographic characteristics
Of the 101,982 women included in the study, 46,920 (46%) were between the ages of 25-35 years, 86,628 (84.9%) were married, and more than one-third (34.9%) had never attended formal schooling. Furthermore, over three-quarters (79.6%) of the participants were from male-head households, about half (50.1%) had exposure to the media, and 62,090 (60.9%) were living in rural areas.
Regarding compliance with at least eight ANC contacts across women’s characteristics, the study found that women with higher education had a compliance rate of 16.2%, while women with no formal education had a compliance rate of 6.5%. Similarly, women from rich households and rural areas had a compliance rate of 15.2% and 15.5%, respectively (Table 2 ).
Obstetric and reproductive characteristics
Of the women included in the study, over half (57.4%) were married at the age of eighteen or older, and about three-quarters (74.2%) had 1 to 2 children under the age of five. Additionally, 30% of the participants had a preceding birth interval of less than 33 months. The study also found that 34% of women didn’t have ANC in the first trimester, 50.7% took iron-folic acid supplements for at least 90 days, and about 33% collaborated with their partners to make healthcare decisions. The study also indicated that 12.8% of women with early ANC booking, 12.2% of women who received nutritional supplements for the recommended period, and 11.3% of women with a history of pregnancy termination had attended the recommended eight antenatal care contacts (Table 3 ).
Level of compliance with at least eight antenatal care contacts
The study found that the pooled level of compliance with the recommended antenatal care contacts among pregnant women in sub-Saharan African countries was 9.9% (95% CI: 9.7% - 10.1%). Sierra Leone had the highest compliance level, with 26.1% of women attending the recommended eight antenatal care contacts. In contrast, Rwanda and Senegal had the lowest compliance levels, with less than 1% of women attending the recommended eight antenatal care contacts. The analysis also showed that only three countries (Liberia (24.9%), Nigeria (25.5%), and Senegal (26.1%)) had relatively better performance in the implementation of the new antenatal care model (Fig. 1 ).

Pooled and country-level estimates of compliance with newly recommended antenatal care contacts in sub-Saharan African Countries
Random effect analysis
In this study, 101,982 pregnant women were nested within 1692 clusters across 16 countries. The result of the random effects analysis indicated that 30% (ICC values of model I) of the variation in the receipt of the recommended antenatal contacts was attributed to cluster-level differences, and 26% (ICC values of model IV) of the variation was accounted for by both individual and community-level aspects. The PCV value of the final model implies that the collective effect of individual and community-level variables accounted for 50% of the variation in maternal compliance with the recommended antenatal care contacts. Furthermore, the MOR of 1.94 in the empty model indicates the presence of heterogeneity in the receipt of at least eight antenatal care contacts between clusters. This implies that compared to women in the clusters with a low level of compliance to the recommended antenatal care contacts, women in the clusters with a higher compliance level had a 94% higher likelihood of attending the recommended contacts (Table 4 ).
Determinants of compliance with at least eight antenatal care contacts
The study found that both individual and community-level characteristics had a significant relationship with the receipt of the recommended ANC contacts in the multivariable multilevel binary logistic regression model. For instance, compared to younger women, women in the ages of 25-34 [AOR (95% CI): 1.11 (1.02, 1.21)] and 35-49 [AOR (95% CI):1.26 (1.12, 1.41)] had a higher likelihood of attending the recommended contacts. The odds of attending the recommended eight ANC contact was higher among women with higher education [AOR (95% CI): 1.28 (1.16, 1.42)], those whose husbands had attended higher education [AOR (95% CI):1.40 (1.26, 1.55)], working women [AOR (95% CI): 1.89 (1.75, 2.05)], those from middle-class [AOR (95% CI): 1.21 (1.10, 1.34)] and wealthy [AOR (95% CI): 1.37 (1.22, 1.54)] households. Furthermore, making joint healthcare decision [AOR (95% CI): 1.36 (1.22, 1.51), early initiation of ANC contacts [AOR (95% CI): 3.91 (3.56, 4.29)], taking of iron-folic acid supplement for at least 90 days [AOR (95% CI): 1.62 (1.49, 1.77)], residing in urban area [AOR (95% CI): 1.71 (1.52, 1.92)], living in a community with low women illiteracy [AOR (95% CI): 1.84 (1.64, 2.07)], and community with low non-exposure to media [AOR (95% CI): 1.33 (1.17, 1.52)] favored women’s attendance of the recommended eight antenatal care contacts (Table 5 ).
This study aimed to assess compliance with the 2016 WHO’s recommended eight antenatal care contacts and its determinants among pregnant women in SSA countries. Our finding showed that the level of compliance with the recommended antenatal care contacts was 9.9% (95% CI: 9.7%- 10.1%), which was higher than the rates reported in Southern Nigeria (2.2%) [ 16 ], Bangladesh (6%) [ 7 ], SSA countries (7.7%) [ 12 ], and Cameroon (8.9%) [ 11 ], but lower than those reported in Myanmar (18%) [ 8 ], Nigeria (17.5%-20%) [ 14 , 18 , 29 ], and Ghana (42%) [ 10 ]. The variation in compliance rates across studies could be attributed to differences in participant characteristics and the countries included in the analysis. Notably, previous studies were mostly based on data from a single country, whereas our study used data from sixteen countries.
Consistent with the findings of a study in Nigeria [ 18 ], the current study found that women aged 25 years and above were more likely to attend the recommended antenatal contacts compared to those younger than 25 years. In addition, this finding is supported by the result of a study in SSA, which reported a reduced odds of non-compliance among older women [ 12 ]. This could be attributed to the possibility that younger women may exhibit poor health-seeking behavior due to inadequate awareness regarding maternal healthcare services.
This study found a significant relationship between women’s literacy both at the individual and community level and their partner’s education with the completion of the recommended antenatal care contacts. In this regard, women with higher education had a 28% higher likelihood of attending optimal antenatal care contacts, while those whose partners had completed higher education had a 40% increased chance of attending these contacts. Furthermore, living in a community with low women’s illiteracy was associated with a higher likelihood of attending adequate antenatal care contacts. This finding is consistent with the previous studies in SSA [ 12 ], Nigeria [ 16 , 18 ], and Uganda [ 17 ]. The possible explanation for this finding is that educated women have a better understanding of the importance of frequent antenatal care and are therefore more likely to adhere to the recommendation than uneducated women.
In this study, women’s employment status was also identified as a significant predictor for attending adequate antenatal care contacts. For instance, employed women were 1.89 times more likely to receive the recommended contacts compared to unemployed women. Consistent with this finding, a study in Uganda revealed that employed women had a 26% increased odds of attending antenatal care contacts as per the recommendation than their counterparts [ 17 ]. This might be because employed women tend to be financially empowered and more autonomous on decisions regarding health service utilization than non-working women and thus likely to receive the service optimally.
According to this study, women belonging to middle-class and wealthy households had a greater chance of receiving the recommended antenatal care contacts, with a 21% and 37% higher likelihood respectively than those from poor families. This result aligns with previous studies in Africa [ 12 , 15 , 16 , 17 , 18 ] and Asia [ 7 , 8 ], which consistently reported a positive association between socioeconomic status and receiving adequate antenatal care contacts. This finding implies that women from economically disadvantaged households may have limited access to healthcare services and thus less likely to receive adequate care.
In addition, our study revealed that women who were involved in healthcare decision-making had a higher likelihood of attending at least eight antenatal care contacts. This finding is supported by a study conducted by Fagbamigbe and colleagues in Nigeria, which demonstrated that women who made healthcare decisions on their own were more likely to attend frequent antenatal care contacts [ 18 ]. This might be because women who are involved in healthcare decision-making may feel more empowered and in control of their health, leading to a greater sense of responsibility and commitment to use maternal healthcare services [ 30 ].
The timing of the initial antenatal care contact was also identified as a significant factor influencing maternal attendance of frequent contacts. Women who booked early for antenatal care were 3.9 times more likely to attend the recommended contacts than those who sought care after the first trimester. In line with this finding, a study conducted in Nigeria also found a negative association between the timing and frequency of antenatal care contacts [ 14 ]. This might be because, with the first ANC contact happening later in pregnancy, there is less time for follow-up contacts. It also implies that women who book early for antenatal care are more likely to be aware of the importance of regular check-ups and may be more motivated to attend subsequent contacts.
According to our analysis, women who took iron-folic acid supplements for at least 90 days were more likely to attend the recommended eight antenatal care contacts compared to those who took the supplement for less than 90 days. This might be because women who receive high-quality antenatal care services are more inclined to adhere to the recommended and subsequent care [ 7 , 17 ].
Compared to women who lived in rural settings, those who resided in urban areas were 1.7 times more likely to attend at least eight antenatal care contacts. This finding is consistent with the results of the previous studies [ 7 , 8 , 14 , 18 ]. The possible reasons for this could be that women in urban areas have better access to healthcare facilities, compared to those in rural areas. Furthermore, geographic barriers in terms of limited transportation options, low health literacy, and socioeconomic status of the rural areas might have contributed to this disparity.
This study also identified community-level media exposure as a significant factor for compliance with the recommended antenatal care contacts. Women from communities with low non-exposure status to mass media were 33% more likely to attend the recommended contacts than those from communities with high non-exposure. This finding aligns with earlier studies that demonstrated the positive effect of media exposure on the uptake of adequate prenatal contacts [ 7 , 16 , 18 ]. This could be because media exposure enhances women’s understanding and perception of maternal healthcare, which ultimately influences their healthcare-seeking behavior.
Strengths and limitations
This study has several notable strengths, including the utilization of a larger sample size, nationally representative data from sixteen countries, and advanced statistical methods. Nonetheless, the cross-sectional nature of the survey’s design precludes establishing a causal relationship between the independent and dependent variables. Furthermore, there is a possibility of recall bias since women were required to recall events that happened two or five years before the survey. Additionally, differences in the survey years across countries may have either overestimated or underestimated the pooled estimate of the outcome variables.
The study found that the compliance rate to the recommended antenatal care contacts among pregnant women in sub-Saharan African countries was very low, with Sierra Leone having the highest compliance rate and Rwanda and Senegal having the lowest. It was also found women’s and partner’s literacy, wealth status, healthcare decision maker, timing of antenatal contacts, consumption of iron-folic acid supplements, residence, and communities-level women’s illiteracy and media exposure were the determinants for the attendance of the recommended eight antenatal care contacts. Therefore, policymakers should focus on improving access to education, especially for women and their partners, and providing exempted services for pregnant women from low-income households. Interventions that target communities with low levels of literacy and media exposure could also be effective in improving the uptake of the services.
Availability of data and materials
The raw dataset used and analyzed in this study can be accessed from the DHS website (https://dhsprogram.com/data/dataset_admin/index.cfm).
Abbreviations
Antenatal care
Adjusted odds ratio
Crude odds ratio
Demographic and health survey
Intra-class correlation coefficient
Log-likelihood
Median odds ratio
Proportion change in variance
Sub-Saharan Africa
World health organization
World Health Organization. Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. World Health Organization; 2023.
Alem AZ, Shitu K, Alamneh TS. Coverage and factors associated with completion of continuum of care for maternal health in sub-Saharan Africa: a multicountry analysis. BMC Pregnancy Childbirth. 2022;22(1):422.
Article PubMed PubMed Central Google Scholar
Bain LE, Aboagye RG, Dowou RK, Kongnyuy EJ, Memiah P, Amu H. Prevalence and determinants of maternal healthcare utilisation among young women in sub-Saharan Africa: cross-sectional analyses of demographic and health survey data. BMC Public Health. 2022;22(1):647.
Awotunde OT, Amole IO, Adesina SA, Adeniran A, OlaOlorun DA, Durodola AO, et al. Pattern of antenatal care services utilization in a mission hospital in Ogbomoso South-west Nigeria. J Adv Med Pharmaceut Sci. 2019Aug 20;21(2):1–1.
Google Scholar
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. World Health Organization; 2016. Available on: https://iris.who.int/bitstream/handle/10665/250796/97892415?sequence=1 .
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience: summary: highlights and key messages from the World Health Organization's 2016 global recommendations for routine antenatal care. BMC J Dis. 2018;10:1–0.
Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: Assessing the extent of compliance with the WHO recommendations. PloS one. 2018;13(9).
Mugo NS, Mya KS, Raynes-Greenow C. Country compliance with WHO-recommended antenatal care guidelines: equity analysis of the 2015–2016 Demography and Health Survey in Myanmar. BMJ global health. 2020;5(12):e002169.
Kumbeni MT, Apanga PA, Yeboah EO, Kolog JT, Awuni B. The relationship between time spent during the first ANC contact, home visits and adherence to ANC contacts in Ghana. Global Health Action. 2021;14(1):1956754.
Ekholuenetale M, Nzoputam CI, Barrow A. Prevalence and socioeconomic inequalities in eight or more antenatal care contacts in Ghana: findings from 2019 population-based data. Int J Womens Health. 2021:349–60.
Boah M, Issah AN, Yeboah D, Kpordoxah MR, Sira J. Association Between Compliance With the New WHO-Recommended Frequency and Timing of Antenatal Care Contacts and Receiving Quality Antenatal Care in Cameroon. SAGE Open. 2022;12(3):21582440221117810.
Article Google Scholar
Odusina EK, Ahinkorah BO, Ameyaw EK, Seidu AA, Budu E, Zegeye B, et al. Noncompliance with the WHO’s Recommended Eight Antenatal Care Visits among Pregnant Women in Sub-Saharan Africa: A Multilevel Analysis. BioMed Res Int. 2021;2021(1):6696829.
PubMed PubMed Central Google Scholar
Roro M, Deressa W, Lindtjørn B. Antenatal care utilization and compliance with national and WHO guidelines in rural Ethiopia: a cohort study. BMC Pregnancy Childbirth. 2022;22(1):849.
Ekholuenetale M, Benebo FO, Idebolo AF. Individual-, household-, and community-level factors associated with eight or more antenatal care contacts in Nigeria: Evidence from Demographic and Health Survey. Plos One. 2020;15(9).
Article CAS PubMed PubMed Central Google Scholar
Dickson KS, Boateng EN, Adde KS, Ameyaw EK, Munro-Kramer ML. Non-adherence to WHO’s recommended 8-contact model: geospatial analysis of the 2017 Maternal Health Survey. BMC Pregnancy Childbirth. 2023;23(1):192.
Sui Y, Ahuru RR, Huang K, Anser MK, Osabohien R. Household socioeconomic status and antenatal care utilization among women in the reproductive-age. Front Public Health. 2021;9:724337.
Towongo MF, Ngome E, Navaneetham K, Letamo G. A secondary analysis of the factors associated with women´ s adequate utilization of antenatal care services during their last pregnancy in Uganda. BMC Pregnancy Childbirth. 2023;23(1):692.
Fagbamigbe AF, Olaseinde O, Setlhare V. Sub-national analysis and determinants of numbers of antenatal care contacts in Nigeria: assessing the compliance with the WHO recommended standard guidelines. BMC Pregnancy Childbirth. 2021;21(1):402.
World Health Organization. WHO antenatal care randomized trial: manual for the implementation of the new model. World Health Organization; 2002. Available on: https://iris.who.int/bitstream/handle/10665/42513/W?sequence=1 .
Afulani PA. Determinants of stillbirths in Ghana: does quality of antenatal care matter? BMC Pregnancy Childbirth. 2016;16:1–7.
Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. 2017;7(11):e017122.
Nimi T, Fraga S, Costa D, Campos P, Barros H. Prenatal care and pregnancy outcomes: a cross-sectional study in Luanda, Angola. Int J Gynecol Obstetr. 2016;135:S72-8.
African Institute for Development Policy‑AFIDEP. Implications of new WHO antenatal guidelines on maternal mortality. Accessed Jan 2024 from. https://www.afdep.org/implicationsnew‑antenatal‑guidelines‑maternal‑mortality/ .
Obago IT. The role of antenatal care in predicting health facility delivery among women in Kenya: further analysis of data from the 2008-09 KDHS. ICF International; 2013.
Wanjira C, Mwangi M, Mathenge E, Mbugua G, Ng’ang’a Z. Delivery practices and associated factors among mothers seeking child welfare services in selected health facilities in Nyandarua South District, Kenya. BMC public health. 2011;11:1–9.
Chilot D, Aragaw FM, Belay DG, Asratie MH, Merid MW, Kibret AA, et al. Effectiveness of eight or more antenatal contacts on health facility delivery and early postnatal care in low-and middle-income countries: a propensity score matching. Front Med. 2023;10:1107008.
Tamirat KS, Sisay MM, Tesema GA, Tessema ZT. Determinants of adverse birth outcome in Sub-Saharan Africa: analysis of recent demographic and health surveys. BMC Public Health. 2021;21:1.
Tadese M, Dagne K, Wubetu AD, Abeway S, Bekele A, Misganaw Kebede W, et al. Assessment of the adverse pregnancy outcomes and its associated factors among deliveries at Debre Berhan Comprehensive Specialized Hospital, Northeast Ethiopia. Plos One. 2022;17(7):e0271287.
Esan OT, Adeomi AA, Afolabi OT. Health insurance coverage and access to maternal healthcare services by women of reproductive age in Nigeria: a cross-sectional study. BMJ Public Health. 2023;1(1).
Imo CK. Influence of women’s decision-making autonomy on antenatal care utilisation and institutional delivery services in Nigeria: evidence from the Nigeria Demographic and Health Survey 2018. BMC Pregnancy Childbirth. 2022;22(1):141.
Download references
Acknowledgements
The authors thank ICF International for granting access to the dataset used in this study.
No specific fund was received for this work.
Author information
Authors and affiliations.
Department of Nursing, College of Medicine and Health Sciences, Samara University, Samara, Ethiopia
Kusse Urmale Mare & Kebede Gemeda Sabo
Department of Epidemiology and Biostatistics, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
Yordanos Sisay Asgedom
Department of Ophthalmology, School of Medicine and Health Science, Debre Tabor University, Debre Tabor, Ethiopia
Zufan Alamrie Asmare
School of Public Health, College of Health Science and Medicine, Dilla University, Dilla, Ethiopia
Tsion Mulat Tebeje
Department of Statistics, College of Natural and Computational Science, Samara University, Samara, Ethiopia
Abdu Hailu Shibeshi
School of Medicine, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
Afework Alemu Lombebo
Department of General Midwifery, School of Midwifery, College of Medicine & Health Sciences, University of Gondar, Gondar, Ethiopia
Bezawit Melak Fente
Department of Public Health, College of Medicine and Health Sciences, Samara University, Samara, Ethiopia
Bizunesh Fantahun Kase, Hiwot Altaye Asebe & Beminate Lemma Seifu
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: Kusse Urmale Mare, Beminate Lemma Seifu, Kebede Gemeda Sabo, Yordanos Sisay Asgedom, Zufan Alamrie Asmare, Tsion Mulat Tebeje, Abdu Hailu Shibeshi, Afework Alemu Lombebo, Bezawit Melak Fente, Bizunesh Fantahun Kase, and Hiwot Altaye Asebe. Data curation: Kusse Urmale Mare, Beminate Lemma Seifu, Kebede Gemeda Sabo, Yordanos Sisay Asgedom, Zufan Alamrie Asmare, Tsion Mulat Tebeje, Abdu Hailu Shibeshi, Afework Alemu Lombebo, Bezawit Melak Fente, Bizunesh Fantahun Kase, and Hiwot Altaye Asebe. Formal analysis: Kusse Urmale Mare, Beminate Lemma Seifu, Kebede Gemeda Sabo. Investigation: Kusse Urmale Mare, Beminate Lemma Seifu, Kebede Gemeda Sabo, Yordanos Sisay Asgedom, Zufan Alamrie Asmare, Tsion Mulat Tebeje, Abdu Hailu Shibeshi, Afework Alemu Lombebo, Bezawit Melak Fente, Bizunesh Fantahun Kase, and Hiwot Altaye Asebe. Methodology: Kusse Urmale Mare, Beminate Lemma Seifu, Kebede Gemeda Sabo, Yordanos Sisay Asgedom, Zufan Alamrie Asmare, Tsion Mulat Tebeje, Abdu Hailu Shibeshi, Afework Alemu Lombebo, Bezawit Melak Fente, Bizunesh Fantahun Kase, and Hiwot Altaye Asebe. Software: Kusse Urmale Mare, Beminate Lemma Seifu, Kebede Gemeda Sabo. Validation: Kusse Urmale Mare, Beminate Lemma Seifu, Kebede Gemeda Sabo, Yordanos Sisay Asgedom, Zufan Alamrie Asmare, Tsion Mulat Tebeje, Abdu Hailu Shibeshi, Afework Alemu Lombebo, Bezawit Melak Fente, Bizunesh Fantahun Kase, and Hiwot Altaye Asebe. Writing – original draft: Kusse Urmale Mare and Beminate Lemma Seifu. Writing – review & editing: Kusse Urmale Mare and Beminate Lemma Seifu.
Corresponding author
Correspondence to Kusse Urmale Mare .
Ethics declarations
Ethics approval and consent to participate.
Since we used secondary data, permission to access the data was granted from the Measure Demographic and Health Survey official Database via an online request at http://www.dhsprogram.com . The survey procedures were also approved by the Institutional Review Board of the host country and ICF International. Additionally, written informed consent was obtained from the study participants during the collection of the survey data.
Consent for publication
Not applicable
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mare, K.U., Sabo, K.G., Asgedom, Y.S. et al. Compliance with the 2016 WHO’s antenatal care recommendation and its determinants among women in Sub-Saharan Africa: a multilevel-analysis of population survey data. BMC Health Serv Res 24 , 1223 (2024). https://doi.org/10.1186/s12913-024-11716-3
Download citation
Received : 21 March 2024
Accepted : 07 October 2024
Published : 12 October 2024
DOI : https://doi.org/10.1186/s12913-024-11716-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Recommended antenatal care
- Pregnant women
- Determinants
- Sub-saharan Africa
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 11 October 2024
Employing machine learning techniques for prediction of micronutrient supplementation status during pregnancy in East African Countries
- Habtamu Setegn Ngusie 1 ,
- Ermias Bekele Enyew 2 ,
- Agmasie Damtew Walle 3 ,
- Bayou Tilahun Assaye 4 ,
- Mulugeta Desalegn Kasaye 2 ,
- Getanew Aschalew Tesfa 5 &
- Alemu Birara Zemariam 6
Scientific Reports volume 14 , Article number: 23827 ( 2024 ) Cite this article
71 Accesses
Metrics details
- Health care
- Medical research
Micronutrient deficiencies, known as “hidden hunger” or “hidden malnutrition,” pose a significant health risk to pregnant women, particularly in low-income countries like the East Africa region. This study employed eight advanced machine learning algorithms to predict the status of micronutrient supplementation among pregnant women in 12 East African countries, using recent demographic health survey (DHS) data. The analysis involved 138,426 study samples, and algorithm performance was evaluated using accuracy, area under the ROC curve (AUC), specificity, precision, recall, and F1-score. Among the algorithms tested, the random forest classifier emerged as the top performer in predicting micronutrient supplementation status, exhibiting excellent evaluation scores (AUC = 0.892 and accuracy = 94.0%). By analyzing mean SHAP values and performing association rule mining, we gained valuable insights into the importance of different variables and their combined impact, revealing hidden patterns within the data. Key predictors of micronutrient supplementation were the mother’s education level, employment status, number of antenatal care (ANC) visits, access to media, number of children, and religion. By harnessing the power of machine learning algorithms, policymakers and healthcare providers can develop targeted strategies to improve the uptake of micronutrient supplementation. Key intervention components involve enhancing education, strengthening ANC services, and implementing comprehensive media campaigns that emphasize the importance of micronutrient supplementation. It is also crucial to consider cultural and religious sensitivities when designing interventions to ensure their effectiveness and acceptance within the specific population. Furthermore, researchers are encouraged to explore and experiment with various techniques to optimize algorithm performance, leading to the identification of the most effective predictors and enhanced accuracy in predicting micronutrient supplementation status.
Similar content being viewed by others

Employing supervised machine learning algorithms for classification and prediction of anemia among youth girls in Ethiopia

Machine learning analysis for the association between breast feeding and metabolic syndrome in women
Prediction of gestational diabetes mellitus using machine learning from birth cohort data of the Japan Environment and Children's Study
Introduction.
Micronutrients, such as vitamins and minerals, are essential for the human body in micrograms or milligrams per day 1 , 2 . They play a crucial role in bodily functions, and deficiencies in any of these micronutrients can lead to severe, and potentially fatal, illnesses 3 . “Hidden hunger” or “hidden malnutrition,” which refers to micronutrient deficiencies, remains a significant global public health challenge, affecting one out of every four people worldwide, totaling more than two billion individuals 4 , 5 . Common micronutrient deficiencies include vitamin A, folate, iron, iodine, and zinc 6 . Low-income countries in Africa and Asia bear a disproportionate burden of micronutrient deficiencies, with vulnerable groups such as pregnant women and children being particularly affected 7 .
Pregnancy-related micronutrient deficiencies have implications for the health of pregnant women and the development of their children 6 , 7 . Micronutrient supplementation is essential to prevent pregnancy complications and reduce the risk of adverse outcomes 8 . Of particular concern is iron-folic acid deficiency, as it contributes significantly to anemia among pregnant women and is the most prevalent micronutrient deficiency worldwide during pregnancy 7 , 9 . Globally, anemia affects up to 36% of pregnant women aged 15–49 years and is estimated to be the cause of 22% of maternal deaths 10 . Low-income countries bear the highest burden of anemia, with East Africa accounting for 39% of global pregnant anemia cases 10 .
The World Health Organization (WHO), in collaboration with member states and other partners, invests significant efforts to address all forms of malnutrition. These initiatives encompass high-folic acid and iron supplementation and fortification of food with micronutrients 2 . As the reduction of all forms of malnutrition is a key agenda of the Sustainable Development Goals (SDGs) for 2030, WHO member states strive to achieve the target level of reducing micronutrient malnutrition 11 . However, despite these efforts, the risks of death due to micronutrient malnutrition remain high among pregnant women and children in Eastern Africa 10 , 12 .
Existing literature on micronutrient intake and deficiency has identified several potential factors contributing to these deficiencies 14 , 15 , 16 . These factors include educational level 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , age 14 , sex 22 , residency 23 , wealth status 13 , 15 , 16 , 18 , 24 , number of children 14 , access to health facilities 25 , media exposure 14 , marital status 26 , working status 26 , and antenatal care (ANC) visits 18 , 27 , 28 .
Machine learning technologies have witnessed widespread adoption and achieved remarkable advancements in various fields. However, their application in the realm of public health and medicine has been relatively limited 29 , 30 . Traditional analytical techniques have predominantly been employed in prior studies investigating the supplementation status of pregnant women in East African countries 31 . However, utilizing machine learning models for predicting micronutrient supplementation can enhance empirical evidence. Machine learning algorithms can capture complex relationships, handle high-dimensional data, adapt to non-linear patterns, and provide robust and efficient analysis of large-scale datasets 32 , 33 . Therefore, in this study, we employed eight state-of-the-art machine learning algorithms, including association rule mining, to predict the status of micronutrient supplementation using recent DHS data from East African countries.
Data source
This study utilized secondary data from the most recent DHS conducted in 12 East African countries, namely Ethiopia (2016), Kenya (2014), Uganda (2016), Tanzania (2016), Burundi (2017), Rwanda (2015), Madagascar (2009), Mozambique (2011), Zimbabwe (2015), Zambia (2018), Malawi (2016), and Comoros (2012). The data sets from these countries were extracted from the official DHS program database, which can be accessed at https://dhsprogram.com/data/available-datasets.cfm.We obtained ethical approval from the Institutional Review Board for the DHS program to access the data.
The DHS Program has conducted standardized surveys in over 90 countries, collecting representative data on population, health, human immunodeficiency virus (HIV), and nutrition. The surveys used a multi-stage stratified sampling method, selecting participants from households within clusters. Sampling strata were created based on rural and urban sectors, and enumeration areas were chosen using probability proportional to size. Within the selected enumeration areas, households were chosen using equal probability systematic sampling. The study specifically examined women aged 15 to 49 residing in East Africa, focusing on those who had been pregnant within the preceding five years of data collection. The research sample included a total of 138,426 individuals from 12 countries in East Africa. The dataset utilized in the study comprised 13 features 34 .
Study variables and measurements
The dependent variable in this study was micronutrient supplementation, defined as the usage of iron folic acid tablets or syrup for at least ninety days or the usage of deworming medicine during a previous pregnancy 35 . Pregnant women meeting these criteria were classified as “supplemented” (coded as 1), while those who did not receive this supplementation were classified as “not supplemented” (coded as 0) 31 . The study considered various independent variables, including place of residence, age group, religion, number of living children, ANC visit, working status, media exposure, marital status, educational status, wealth status, birth interval, and distance from health facility. The selection of these independent variables was based on a comprehensive review of previous literature 13 , 31 .
Data preprocessing
The process of machine learning begins with data pre-processing, which involves modifying or encoding the data to make it suitable for computer interpretation 36 . In our machine learning workflow, we employed a continuous improvement process for our models. This process included selecting and engineering relevant features, balancing the data, splitting the data, model training, model evaluation, model optimization, choosing the top performer model, and deploying the selected model for prediction. Through an iterative approach, we refined our models. Figure 1 provides a visual representation of the steps in our workflow; however, it does not encompass certain tasks that were iteratively performed throughout the process.

Study work flow diagram.
Data cleaning
During the data analysis process, we manually examined the data for redundancy and determined that no redundant data were present in our dataset. To handle missing values, we utilized the K-nearest neighbors (KNN) imputation technique 41 . We employed various visualization techniques such as scatter plots, box plots, and histograms to identify outliers. Additionally, we assessed multicollinearity by examining the correlation matrix and considering a correlation value above 0.8 between two pairs of variables as indicative of high correlation 37 , 38 .
Feature engineering
Feature engineering involves identifying, acquiring, and modifying the most relevant characteristics from the available data to construct machine learning models that are more accurate and efficient 39 . We employed one-hot encoding for nominal categorical variables and label encoding for ordinal categorical variables to encode the data 40 .
Dimensionality reduction
We employed various techniques for dimensionality reduction in our study, aiming to optimize model performance and reduce the complexity of our dataset. These techniques included univariate selection, recursive feature elimination (RFE), random forest feature elimination, principal component analysis (PCA), lasso regression, and a feature selection method based on Boruta 41 .
Through repeated experiments, we found that the Boruta-based feature selection method outperformed other techniques in terms of accuracy and robustness. The Boruta-based feature selection method assesses feature importance by comparing their performance against randomly generated shadow features that simulate noise. Features consistently outperforming the shadow features are deemed significant and incorporated into our predictive model 42 .
Data balancing
Data imbalance poses a common challenge in data mining and machine learning, often leading to decreased classification accuracy for instances belonging to the minority class 43 . To tackle this issue, we utilized four data balancing methods: under-sampling, over-sampling, adaptive synthetic sampling (ADASYN), and synthetic minority oversampling technique (SMOTE). Each of these techniques has distinct characteristics and aims to address class imbalance effectively.
Under-sampling involves reducing the number of instances from the majority class to achieve a more balanced dataset. By randomly removing instances from the majority class, under-sampling aims to align the number of instances in the minority class with that in the majority class. This approach prevents classifier bias towards the majority class, but it may result in the loss of potentially valuable information 44 , 45 , 46 .
On the other hand, over-sampling increases the number of instances in the minority class by replicating or generating new instances. This technique ensures a balanced dataset by ensuring that the number of instances in the minority class is comparable to that in the majority class. Over-sampling can be achieved through methods such as random duplication, bootstrapping, or synthetic data generation 46 , 47 .
ADASYN extends the SMOTE technique to address its limitation in handling datasets with varying densities within the minority class. ADASYN synthesizes new instances in the minority class by considering the distribution of instances in the feature space. It focuses on generating more synthetic examples for the minority class instances that are harder to classify, thereby adapting the sampling strategy to the local characteristics of the data 48 .
SMOTE, on the other hand, is a popular over-sampling technique that creates synthetic instances in the minority class by interpolating between existing instances. It randomly selects a minority class instance and identifies its k nearest neighbors. It then generates synthetic instances by randomly selecting a neighbor and creating a new instance along the line segment between the original instance and the chosen neighbor. SMOTE helps balance the dataset and introduces diversity in the minority class 48 , 49 .
To enhance the performance of our predictive model, we initially trained our machine learning algorithms using unbalanced data. Subsequently, we explored and applied the aforementioned balancing techniques to train the models using balanced datasets. To evaluate the performance of each model across each data balancing technique, we conducted a comprehensive analysis using five performance metrics: accuracy, precision, recall, F1-score, and AUC.
While accuracy is suitable for evaluating models with balanced classes, AUC becomes particularly valuable when dealing with imbalanced datasets or when the relative costs of false positives and false negatives are uncertain. However, it is advisable to consider both accuracy and AUC, along with other relevant metrics, to obtain a comprehensive evaluation of model performance and make informed comparisons between different machine learning algorithms 50 , 51 , 52 . Based on these considerations, we selected the data balancing technique that demonstrated superior performance for the final prediction.
Model selection and development
In our study, the dependent variable, micronutrient supplementation status, required a classification approach, as it was divided into “supplemented” and “not supplemented” categories. To make predictions, we needed to select appropriate classifiers. We utilized the Scikit-learn version 1.3.2 packages in Python, implemented within Jupyter Notebook, to employ machine learning algorithms.
To evaluate the predictive capabilities of machine learning algorithms for predicting micronutrient supplementation status, we employed eight state-of-the-art algorithms. Each algorithm has its unique approach and characteristics. Here are brief definitions for each of the algorithms we utilized:
Support Vector Machines (SVM) with Kernel Methods: SVM is a powerful algorithm used for both classification and regression tasks. It constructs a hyperplane or a set of hyperplanes in a high-dimensional space to separate different classes 53 .
Gaussian Naive Bayes: This algorithm is based on Bayes’ theorem, assuming that features are conditionally independent. It is particularly effective when dealing with high-dimensional data 54 , 55 .
Logistic Regression: Logistic regression is a statistical model that is used for binary classification. It estimates the probability of an instance belonging to a particular class based on the input features 56 , 57 .
Decision Tree Classifier: Decision trees are hierarchical structures that make decisions based on the values of input features. The decision tree classifier uses a tree-like model of decisions and their possible consequences to predict the class label of instances 58 .
Random Forest Classifier: Random forest is an ensemble learning method that combines multiple decision trees. It generates a set of decision trees and makes predictions by averaging the outputs of individual trees 59 .
Gradient Boosting Machines: Gradient boosting is another ensemble learning method that combines multiple weak prediction models, typically decision trees, to create a strong predictive model. It trains new models to correct the mistakes made by previous models 60 , 61 .
eXtreme Gradient Boosting (XGBoost): XGBoost is an optimized implementation of gradient boosting that provides better performance and scalability. It employs a variety of regularization techniques to prevent overfitting and enhance the overall predictive power 62 .
KNN: KNN is a non-parametric algorithm that classifies instances based on their similarity to neighboring instances. It assigns a class label to an instance by considering the labels of its k nearest neighbors in the feature space 63 .
The selection of these algorithms was based on their suitability for classification tasks and their compatibility with the characteristics of our dataset 64 , 65 , 66 .
Model training and evaluation
In order to construct a reliable predictive model within machine learning, it is essential to perform model training and evaluation 67 , 68 . In this particular study, a straightforward approach was employed, where the data was divided into an 80% training set and a 20% testing set. This division allowed us to assess the performance of each predictive model effectively.
To evaluate the performance of the predictive models, several metrics were utilized, including accuracy, precision, recall, F1-score, and AUC. Each of these metrics provides valuable insights into different aspects of the model’s performance.
Accuracy: Accuracy measures the overall correctness of the model’s predictions. It is calculated as the ratio of the number of correct predictions to the total number of predictions.
Precision: Precision evaluates the accuracy of positive predictions made by the model. It quantifies the proportion of true positive predictions out of the total predicted positives. The formula for precision is:
Precision = TP / (TP + FP) where TP represents true positive and FP represents false positive.
Recall: Recall, also known as sensitivity or true positive rate, assesses the model’s ability to identify all positive instances. It measures the proportion of true positive predictions out of the total actual positives. The formula for recall is:
Recall = TP / (TP + FN) where TP represents true positive and FN represents false negative.
F1-score: The F1-score provides a balanced measure of a model’s performance by considering both precision and recall. It is the harmonic mean of precision and recall, and it is calculated using the following formula:
F1-score = 2 * (Precision * Recall) / (Precision + Recall).
AUC: AUC is a metric calculated from the area under the receiver operating characteristic (ROC) curve. The ROC curve represents the true positive rate (TPR) plotted against the false positive rate (FPR) at various classification thresholds. AUC indicates the algorithm’s ability to discriminate between classes, where a higher AUC value suggests better discrimination.
In summary, by utilizing these metrics, we were able to comprehensively evaluate the performance of each predictive model in terms of overall correctness, accurate positive predictions, identification of positive instances, balanced measure, and discriminatory ability 69 .
In order to further evaluate the performance of the model, tenfold cross-validation techniques were employed. Prior to this, different k-fold validation techniques, including three-fold, five-fold, and ten-fold, were compared to determine the most suitable approach 70 .
The study also conducted a thorough analysis of hyperparameters to refine and improve the model’s performance. Grid search, random search, and Bayesian optimization were systematically explored to find the best hyperparameter settings. Comparing the outcomes from these techniques helped identify the configurations that provided the highest performance. In order to improve the accuracy and dependability of the model used in this study, we conducted model calibration. Through fine-tuning the model via calibration, we enhanced its performance in accurately predicting the desired outcome.
In our study, we conducted an extensive comparison of different kernel methods for the SVM model, with the main goal of identifying the most suitable kernel function to maximize the model’s performance. We carefully evaluated and compared various kernel functions, including linear, polynomial, radial basis function (RBF), and sigmoid. Through meticulous analysis, our objective was to select the kernel method that produced the most favorable outcomes and achieved optimal performance for the SVM model 71 .
Model interpretability
In our comprehensive approach to understanding the data and exploring the factors influencing the prediction of micronutrient supplementation, we employed various techniques including the Apriori algorithm. Firstly, we calculated the mean SHAP (Shapley Additive exPlanations) values to assess the average impact of each feature on the model’s predictions, providing insights into the relative significance of different variables. This allowed us to understand the individual contributions of each feature.
Additionally, we utilized the Apriori algorithm, a popular algorithm for association rule mining. By applying the Apriori algorithm, we were able to uncover hidden patterns and relationships among the variables in the dataset. The algorithm allowed us to discover frequent item sets and association rules based on measures such as lift and confidence. Lift helped us determine the strength of the associations between different variables, indicating the degree to which the presence of one variable influences the likelihood of another variable occurring. Confidence, on the other hand, provided us with a measure of reliability or certainty in the association rules, indicating how often the consequent variable appeared when the antecedent variable was present 72 , 73 , 74 .
By incorporating mean SHAP values and the Apriori algorithm into our analysis, we gained a deeper understanding of the dataset and the factors influencing the prediction of micronutrient supplementation. These techniques allowed us to uncover concealed patterns and relationships, leading to robust predictions and identification of influential factors. In summary, our approach involved calculating mean SHAP values to determine feature importance and utilizing the Apriori algorithm for association rule mining. This comprehensive methodology provided us with valuable insights into the dataset, enhancing model interpretability and facilitating a better understanding of the factors impacting micronutrient supplementation predictions 75 , 76 , 77 .
Descriptive results of the background characteristics
The study encompassed a comprehensive analysis of descriptive and socio-demographic characteristics among a weighted sample of 138,426 pregnant women. Among the participants, the largest proportion, comprising 57,174 (41.30%), fell within the age group of 26 to 34 years. In terms of residence, the majority, accounting for 105,613 (76.30%) of the study participants, hailed from rural areas. Regarding employment status, a significant number of respondents, totaling 101,407 (73.26%), were employed (See Table 1 for more detailed information).
Micronutrient supplementation status in east African countries
According to the specified DHS dataset, the pooled prevalence of micronutrient supplementation status among pregnant women in East Africa was found to be 28.90% (95% CI: 28.68, 29.12). Ethiopia had the lowest rate of micronutrient supplementation among pregnant women, with only 7.80% receiving supplementation. On the other hand, Zambia had the highest prevalence of micronutrient supplementation, with 66.94% of pregnant women receiving supplementation (See Fig. 2 for more detailed information).

Prevalence of micronutrient supplementation status among pregnant women in East Africa countries using forest tree plot.
Machine learning analysis of micronutrient status
Feature selection.
Upon evaluating various feature selection methods, we observed that the Boruta algorithm exhibited strong performance. As depicted in Fig. 3 , the algorithm effectively visualized the importance of variables, with significant variables highlighted in green, unimportant variables in red, and tentative variables in yellow. Tentative variables are those that require further investigation 78 .
In our comprehensive analysis, we decided to exclude birth interval and marital status from consideration, as the Boruta algorithm deemed them unimportant. No tentative variables were identified. Consequently, we proceeded with utilizing the variables selected by the Boruta algorithm to predict the micronutrient supplementation status and explore data patterns through association rule mining.

Feature selection using Boruta algorithm (Note: v218 = number of children, v025 = residence).
In Table 2 , various data balancing techniques, such as under-sampling, over-sampling, ADASYN, and SMOTE, were compared. Among the evaluated techniques, SMOTE demonstrated the highest performance, with the random forest classifier achieving an AUC of 0.878 and an accuracy of 91%. The results indicated that SMOTE outperformed other data balancing methods.
Development and performance comparisons of machine learning-based models
By utilizing these performance metrics such as accuracy, precision, recall, F1 score, and AUC, we conducted a comprehensive evaluation to determine how effectively the algorithms could predict micronutrient supplementation. Table 3 presents the performance measures of multiple selected algorithms after data balancing and calibrated tuning processes had been applied. Based on the evaluation results, the top three machine learning algorithms for classifying micronutrient supplementation status were found to be the random forest classifier, decision tree classifier, and XGBoost with excellent ROC value ( See Table 3 ).
Figure 4 illustrates the ROC curve analysis conducted on selected machine learning algorithms. These algorithms were trained on balanced data using the SMOTE data balancing technique and underwent optimized hyperparameter tuning. Among the different hyperparameter tuning techniques experimented with, grid search proved to be the most suitable for our dataset. The application of hyperparameter tuning resulted in a significant enhancement in the performance of our model. For a detailed comparison, please refer to Figs. 4 and 5 , which respectively present the ROC curve analysis before and after hyperparameter tuning.
As depicted in Fig. 5 , the final ROC curve for the tuned model showcased that the random forest classifier outperformed all other machine learning algorithms, exhibiting an AUC of 0.892. The decision tree classifier and XGBoost followed closely behind with AUC values of 0.862 and 0.856, respectively, which can be considered excellent. The KNN, Gradient boosting classifier, and SVM achieved reasonably acceptable ROC values of 0.797, 0.739, and 0.721, respectively. However, the logistic regression and Gaussian Naïve Bayes algorithms displayed lower AUC values of 0.683 and 0.651, respectively, indicating suboptimal discrimination.
We also provided a comprehensive comparison of model performance using various performance metrics. In cases where the machine learning algorithms exhibited similar performance and distinguishing the superior algorithm became challenging, we used a comprehensive analysis. For further details, please refer to Fig. 6 .

ROC curve analysis of selected machine learning algorithms with balanced data using SMOTE data balancing technique.

ROC curve analysis of selected machine learning algorithms after optimized Hyperparameter tuning using balanced data.

Overall model performance of selected machine learning algorithms after optimized hyperparameter tuning of a balanced data.
SHAP value interpretation
Based on the findings presented in Fig. 7 , the mean SHAP value report provided insights into the relative importance of different features in the classification model. ANC visits, number of living children, and media exposure emerged as the most influential factors and exhibited high mean SHAP values. This indicated that these features had high significant impact on the model’s predictions.
Additionally, religion, working status, education status, age group, and wealth status displayed minimal influence on the classification outcome, as evidenced by their low mean SHAP values. These features contribute less to the model’s decision-making process and have limited importance on the model prediction. On the other hand, residence and perceived distance were positioned at the bottom of the graph, with a mean SHAP value of zero. This suggests that these features do not contribute to the model prediction.

A mean SHAP value report.
Association rule mining
Using the Apriori algorithm, our research identified the most influential association rules based on their lift values and confidence. These rules provided valuable insights into the probability of micronutrient supplementation during pregnancy in East African countries. Remarkably, the recurring presence of factors such as maternal education level, employment status, ANC visit, media accessibility, number of living children, and religion in these association rules indicated their consistent association with the likelihood of receiving micronutrient supplementation.
The top five association rules and their corresponding lift values are as follows:
1. If the mother has a secondary education, is employed, has more than four ANC visits, and has media exposure, the probability of being supplemented with micronutrients is 86.3% (Confidence = 0.863 and lift = 2.36).
2. If the mother is in the age group of 21 to 25, has less than three children, has more than four ANC visits, and follows the catholic religion, the probability of being supplemented with micronutrients is 85.9% (Confidence = 0.859 and lift = 2.04).
3. If the mother has less than three children, access to media, follows the Catholic religion, and has higher education, the probability of being supplemented with micronutrients is 81.4% (Confidence = 0.814 and lift = 1.64).
4. If the mother has less than three children, is employed, in the age group of 26 to 34, has higher education, and follows the traditional or animist religion, the probability of being supplemented with micronutrients is 78.4% (Confidence = 0.784 and lift = 1.83).
5. If the mother has four ANC visits, is employed, has access to media, belongs to a high-income wealth status, and has a primary education, the probability of being supplemented with micronutrients is 74.3% (Confidence = 0.743 and lift = 1.25).
The study demonstrated the potential of machine learning algorithms in accurately predicting the status of micronutrient supplementation among pregnant women in East Africa. The random forest classifier, decision tree classifier, and XGBoost were identified as the most effective models for classifying supplementation status. Specifically, the random forest classifier outperformed other algorithms, with an AUC value of 0.892 and an accuracy of 94.0%. Similar studies conducted in Rwanda 33 , Zambia 79 , Ethiopia 80 , Mozambique, and Nigeria 81 also found the random forest model to be superior in predicting various health outcomes.
We used association rule mining to identify the top predictors in our data set. Accordingly, we built five top rules using association rule mining and implied that the mother’s education level consistently appeared in association rules and had a significant impact on the likelihood of receiving micronutrient supplementation. The justification for this impact was supported by the existing research literature. Similar to our findings studies conducted in Central Ethiopia 21 , Kenya 19 , and Bangladesh 20 , and elsewhere in the world 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 noticed the importance of education for enhancing micronutrient supplementation status. One possible justification for this finding could be that education empowers individuals to make informed decisions regarding their health and encourages adherence to prenatal care.
Based on the finding of the association rule mining, ANC visits were a strong predictor that influenced the likelihood of receiving micronutrient supplementation. This finding was supported by global studies highlighting the significance of ANC visits in enhancing supplementation status 18 , 27 , 28 . The possible justification could be ANC visits may serve as a platform for healthcare providers to educate pregnant women about the importance of proper nutrition and micronutrient supplementation, addressing misconceptions and providing information on the specific benefits of supplementation through counseling sessions.
Association rule mining consistently demonstrated that religion played a significant role in determining the likelihood of receiving micronutrient supplementation. This finding underscores the importance of considering religious factors in public health interventions and highlights the need for culturally sensitive strategies to address micronutrient deficiencies in diverse religious communities 82 .
The association rule mining consistently demonstrated that an increase in the number of children had a negative association with the likelihood of receiving micronutrient supplementation. This association was supported by the literature, which underscores the significance of family size as a determinant of access to and utilization of health services 14 . The possible reason for this finding is that the added responsibilities of raising a larger family may pose challenges for parents, especially busy mothers, in prioritizing and accessing healthcare, including attending antenatal care visits and receiving the necessary micronutrient supplements.
The association rule mining consistently provided evidence that individuals with media exposure had a higher probability of receiving adequate micronutrient supplementation. This finding was further supported by the literature, which emphasized the role of media in influencing health-related behaviors 14 . The justification for this finding could be media platforms provide opportunities to educate individuals about the benefits of adequate nutrition and the availability of supplementation programs.
The consistent findings from association rule mining indicate that individuals who had primary, secondary, and higher levels of education are more likely to receive micronutrient supplementation. Previous studies conducted worldwide supported this relationship 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 . This could be attributed to the fact that individuals with higher education levels may possess a deeper understanding of the significance of proper nutrition and the specific advantages of taking micronutrient supplements during pregnancy.
The association rule mining consistently revealed the significant impact of employment status on the likelihood of receiving micronutrient supplementation. This finding was consistent with a study conducted in Northwest Ethiopia 26 . One possible justification is that employed women may have greater exposure to health-related information through workplace wellness programs, employee benefits, or interactions with colleagues.
Strength and limitations of the study
The study demonstrates its strength by employing a comprehensive analysis of predictive capabilities through the use of eight supervised machine-learning algorithms. This approach enhances the reliability and credibility of the findings by revealing hidden patterns and relationships within the data. However, it is important to acknowledge certain limitations associated with the study. The retrospective data collection and reliance on secondary data introduce potential drawbacks, including the possibility of incomplete or missing data, which may impact the accuracy and introduce biases in the results.
Additionally, the study only explores four data balancing techniques, which may limit the ability to fully harness the potential power of each machine learning algorithm. Another limitation is the absence of exploring the performance of each algorithm through ensembling, a technique that combines multiple models to enhance predictive accuracy. Lastly, it is worth noting that the study shares the inherent limitation of building association rules solely based on the Apriori algorithm.
The study highlights the effectiveness of machine learning in accurately predicting the status of micronutrient supplementation among pregnant women in East Africa. Notably, the random forest classifier demonstrated exceptional performance, achieving excellent evaluation scores with an AUC of 0.892 and an accuracy of 94.0% in predicting the supplementation status. This emphasizes the potential of machine learning algorithms as valuable tools for policymakers and healthcare providers to develop targeted strategies aimed at improving the uptake of micronutrient supplementation among pregnant women.
Based on the study’s findings, several key intervention components are recommended to enhance the utilization of micronutrient supplementation. Strengthening educational initiatives can provide vital information on the importance and benefits of supplement intake. Improving antenatal care services ensures proper screening, monitoring, and guidance for pregnant women regarding their nutritional needs. Comprehensive media campaigns can effectively raise awareness and emphasize the significance of micronutrient supplementation during pregnancy. It is also crucial to consider cultural and religious sensitivities when designing interventions to ensure their acceptance and effectiveness within the specific population.
Furthermore, researchers are encouraged to explore and experiment with various techniques to optimize algorithm performance, leading to the identification of the most effective predictors and enhanced accuracy in predicting micronutrient supplementation status.
Data availability
To access the data used in the study, it is necessary to log in to the official website of the DHS: http://www.dhsprogram.com .
Abbreviations
Adaptively generating minority data
Antenatal care
Area under the ROC curve
Confidence interval
Demographic and Health Survey
False positive rate
Human immunodeficiency virus
K-nearest neighbor
Principal component analysis
Radial basis function
Recursive feature elimination
Receiver operating characteristic curve
Shapley Additive exPlanations
Sustainable Development Goals
Synthetic minority over-sampling technique
Support vector machine
True positive rate
World Health Organization
eXtreme Gradient Boosting
Corvallis Minerals Micronutrient Information Center, Oregon State University: Linus Pauling Institute; updated Nov 21, 2023. (2018). https://lpi.oregonstate.edu/mic
WHO. Ambition and action in nutrition 2016–2025 Geneva: WHO. (2016). https://www.who.int/health-topics/micronutrients#tab=tab_1
Godswill, A. G., Somtochukwu, I. V., Ikechukwu, A. O. & Kate, E. C. Health benefits of micronutrients (vitamins and minerals) and their associated deficiency diseases: a systematic review. Int. J. Food Sci. 3 (1), 1–32 (2020).
Google Scholar
Punia, S. & Kumar, M. Functionality and Application of Colored Cereals: Nutritional (Elsevier, 2022).
Von Grebmer, K. et al. Synopsis: 2014 Global Hunger Index: The Challenge of Hidden Hunger (Intl Food Policy Res Inst, 2014).
Bailey, R. L., West, K. P. Jr. & Black, R. E. The epidemiology of global micronutrient deficiencies. Ann. Nutr. Metab. 66 (Suppl. 2), 22–33 (2015).
Article PubMed Google Scholar
Gernand, A. D., Schulze, K. J., Stewart, C. P., West, K. P. Jr. & Christian, P. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat. Rev. Endocrinol. 12 (5), 274–289 (2016).
Article PubMed PubMed Central Google Scholar
Haider, B. A., Yakoob, M. Y. & Bhutta, Z. A. Effect of multiple micronutrient supplementation during pregnancy on maternal and birth outcomes. BMC Public. Health . 11 , 1–9 (2011).
Article Google Scholar
Karami, M., Chaleshgar, M., Salari, N., Akbari, H. & Mohammadi, M. Global prevalence of anemia in pregnant women: a comprehensive systematic review and meta-analysis. Matern. Child Health J. 26 (7), 1473–1487 (2022).
Stevens, G. A. et al. National, regional, and global estimates of anaemia by severity in women and children for 2000–19: a pooled analysis of population-representative data. Lancet Global Health . 10 (5), e627–e39 (2022).
Article MathSciNet PubMed Google Scholar
Redón Lago, A. Hidden hunger in the current world: causes, consequences and solutions to a global public health challenge and a particular look at Spain. (2021).
Galani, Y., Orfila, C. & Gong, Y. A review of micronutrient deficiencies and analysis of maize contribution to nutrient requirements of women and children in Eastern and Southern Africa. Crit. Rev. Food Sci. Nutr. 62 (6), 1568–1591 (2022).
Brunst, K. J. et al. Racial/ethnic and sociodemographic factors associated with micronutrient intakes and inadequacies among pregnant women in an urban US population. Public Health. Nutr. 17 (9), 1960–1970 (2014).
Serra-Majem, L. et al. Determinants of nutrient intake among children and adolescents: results from the enKid Study. Ann. Nutr. Metab. 46 (Suppl. 1), 31–38 (2002).
Cembranel, F., Wagner, K. J. P., González-Chica, D. A. & d’Orsi, E. Education and income levels are associated with energy and micronutrient intake. Int. J. Vitam. Nutr. Res. (2019).
Liu, F-L. et al. Nutrient intakes of pregnant women and their associated factors in eight cities of China: a cross-sectional study. Chin. Med. J. 128 (13), 1778–1786 (2015).
Article ADS PubMed PubMed Central Google Scholar
Shalini, T. et al. Micronutrient intakes and status assessed by probability approach among the urban adult population of Hyderabad city in South India. Eur. J. Nutr. 58 , 3147–3159 (2019).
Yeneabat, T. et al. Maternal dietary diversity and micronutrient adequacy during pregnancy and related factors in East Gojjam Zone, Northwest Ethiopia, 2016. BMC Pregnancy Childbirth . 19 (1), 1–9 (2019).
Kiboi, W., Kimiywe, J. & Chege, P. Determinants of dietary diversity among pregnant women in Laikipia County, Kenya: a cross-sectional study. BMC Nutr. 3 (1), 1–8 (2017).
Shamim, A. A. et al. Pregnant women diet quality and its sociodemographic determinants in southwestern Bangladesh. FoodNutr. Bull. 37 (1), 14–26 (2016).
Kebede, A. N., Sahile, A. T. & Kelile, B. C. Dietary diversity and Associated factors among pregnant women in Addis Ababa, Ethiopia, 2021. Int. J. Public Health 67 , 1605377 (2022).
Thillan, K. et al. Micronutrient status and associated factors of adiposity in primary school children with normal and high body fat in Colombo municipal area, Sri Lanka. BMC Pediatr. 21 (1), 1–14 (2021).
Gebremedhin, T., Aschalew, A. Y., Tsehay, C. T., Dellie, E. & Atnafu, A. Micronutrient intake status and associated factors among children aged 6–23 months in the emerging regions of Ethiopia: a multilevel analysis of the 2016 Ethiopia demographic and health survey. PloS One . 16 (10), e0258954 (2021).
Nguyen, P. H. et al. Micronutrient intakes among women of reproductive age in Vietnam. PLoS One . 9 (2), e89504 (2014).
Article ADS MathSciNet PubMed PubMed Central Google Scholar
Tzioumis, E., Kay, M. C., Bentley, M. E. & Adair, L. S. Prevalence and trends in the childhood dual burden of malnutrition in low-and middle-income countries, 1990–2012. Public Health Nutr. 19 (8), 1375–1388 (2016).
Awoke, M. et al. Micronutrient intake inadequacy and its associated factors among lactating women in Bahir Dar City, Northwest Ethiopia, 2021. Plos One . 17 (7), e0271984 (2022).
Nguyen, P. H. et al. Integrating nutrition interventions into an existing maternal, neonatal, and child health program increased maternal dietary diversity, micronutrient intake, and exclusive breastfeeding practices in Bangladesh: results of a cluster-randomized program evaluation. J. Nutr. 147 (12), 2326–2337 (2017).
Haileslassie, K., Mulugeta, A. & Girma, M. Feeding practices, nutritional status and associated factors of lactating women in Samre Woreda, South Eastern Zone of Tigray, Ethiopia. Nutr. J. 12 , 1–11 (2013).
Sarker, I. H. Machine learning: algorithms, real-world applications and research directions. SN Comput. Sci. 2 (3), 160 (2021).
Jordan, M. I. & Mitchell, T. M. Machine learning: Trends, perspectives, and prospects. Science . 349 (6245), 255–260 (2015).
Article ADS MathSciNet PubMed Google Scholar
Enyew, E. B. et al. Micronutrient intake and associated factors among pregnant women in East Africa: Multilevel logistic regression analysis. Plos One . 18 (4), e0281427 (2023).
Tesfaye, B., Atique, S., Azim, T. & Kebede, M. M. Predicting skilled delivery service use in Ethiopia: dual application of logistic regression and machine learning algorithms. BMC Med. Inf. Decis. Mak. 19 (1), 1–10 (2019).
Mfateneza, E., Rutayisire, P. C., Biracyaza, E., Musafiri, S. & Mpabuka, W. G. Application of machine learning methods for predicting infant mortality in Rwanda: analysis of Rwanda demographic health survey 2014–15 dataset. BMC Pregnancy Childbirth . 22 (1), 388 (2022).
Guide to DHS Statistics DHS-7 (version 2) [Internet]. USAID. [cited November 24, 2023]. (2020). https://dhsprogram.com/data/Guide-to-DHS-Statistics/index.cfm
WHO. World Health Organization recommendations on antenatal care for a positive pregnancy experience Geneva2018 [ https://www.who.int/publications/i/item/9789241549912
Kadhim, A. I. An evaluation of preprocessing techniques for text classification. Int. J. Comput. Sci. Inform. Secur. (IJCSIS) . 16 (6), 22–32 (2018).
Liu, X. et al. Machine learning-based correlation study between perioperative immunonutritional index and postoperative anastomotic leakage in patients with gastric cancer. Int. J. Med. Sci. 19 (7), 1173 (2022).
Article MathSciNet PubMed PubMed Central Google Scholar
Anand, H. & Vinodchandra, S. (eds) Applying correlation threshold on Apriori algorithm. 2013 IEEE International Conference ON Emerging Trends in Computing, Communication and Nanotechnology (ICECCN); : IEEE. (2013).
Zheng, A. & Casari, A. Feature Engineering for Machine Learning: Principles and Techniques for data Scientists ( O’Reilly Media, Inc., 2018).
Al-Shehari, T. & Alsowail, R. A. An insider data leakage detection using one-hot encoding, synthetic minority oversampling and machine learning techniques. Entropy . 23 (10), 1258 (2021).
Rawat, S., Rawat, A., Kumar, D. & Sabitha, A. S. Application of machine learning and data visualization techniques for decision support in the insurance sector. Int. J. Inform. Manag. Data Insights 1 (2), 100012 (2021).
Pudjihartono, N., Fadason, T., Kempa-Liehr, A. W. & O’Sullivan, J. M. A review of feature selection methods for machine learning-based disease risk prediction. Front. Bioinf. 2 , 927312 (2022).
Arafat, M. Y., Hoque, S., Xu, S. & Farid, D. M. Machine learning for mining imbalanced data. (2019).
Krawczyk, B. Learning from imbalanced data: open challenges and future directions. Progress Artif. Intell. 5 (4), 221–232 (2016).
Jadhav, A., Mostafa, S. M., Elmannai, H. & Karim, F. K. An empirical assessment of performance of data balancing techniques in classification task. Appl. Sci. 12 (8), 3928 (2022).
Bach, M., Werner, A., Żywiec, J. & Pluskiewicz, W. The study of under-and over-sampling methods’ utility in analysis of highly imbalanced data on osteoporosis. Inf. Sci. 384 , 174–190 (2017).
Shelke, M. S., Deshmukh, P. R. & Shandilya, V. K. A review on imbalanced data handling using undersampling and oversampling technique. Int. J. Recent. Trends Eng. Res. 3 (4), 444–449 (2017).
Brandt, J. & Lanzén, E. A comparative review of SMOTE and ADASYN in imbalanced data classification. (2021).
Fernández, A., Garcia, S., Herrera, F. & Chawla, N. V. SMOTE for learning from imbalanced data: progress and challenges, marking the 15-year anniversary. J. Artif. Intell. Res. 61 , 863–905 (2018).
Article MathSciNet Google Scholar
Carrington, A. M. et al. Deep ROC analysis and AUC as balanced average accuracy, for improved classifier selection, audit and explanation. IEEE Trans. Pattern Anal. Mach. Intell. 45 (1), 329–341 (2022).
Bekkar, M., Djemaa, H. K. & Alitouche, T. A. Evaluation measures for models assessment over imbalanced data sets. J. Inf. Eng. Appl. 3 (10), 156-168 (2013).
Japkowicz, N. Assessment metrics for imbalanced learning. Imbalanced learning: Foundations, algorithms, and applications. pp. 187–206. (2013).
Scholkopf, B. & Smola, A. J. Learning with Kernels: Support Vector Machines, Regularization, Optimization, and beyond (MIT Press, 2018).
Kamel, H., Abdulah, D. & Al-Tuwaijari, J. M. (eds) Cancer classification using gaussian naive bayes algorithm. 2019 international engineering conference (IEC); IEEE. (2019).
Jahromi, A. H. & Taheri, M. (eds) A non-parametric mixture of Gaussian naive Bayes classifiers based on local independent features. 2017 Artificial intelligence and signal processing conference (AISP); IEEE. (2017).
Christodoulou, E. et al. A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. J. Clin. Epidemiol. 110 , 12–22 (2019).
Zou, X., Hu, Y., Tian, Z. & Shen, K. (eds) Logistic regression model optimization and case analysis. 2019 IEEE 7th international conference on computer science and network technology (ICCSNT); IEEE. (2019).
Priyanka, K. D. Decision tree classifier: a detailed survey. Int. J. Inform. Decis. Sci. 12 (3), 246–269 (2020).
Parmar, A., Katariya, R. & Patel, V. (eds) A review on random forest: An ensemble classifier. International conference on intelligent data communication technologies and internet of things (ICICI) 2018; Springer. (2019).
Lu, H., Karimireddy, S. P., Ponomareva, N. & Mirrokni, V. (eds) Accelerating gradient boosting machines. International conference on artificial intelligence and statistics; PMLR. (2020).
Bentéjac, C., Csörgő, A. & Martínez-Muñoz, G. A comparative analysis of gradient boosting algorithms. Artif. Intell. Rev. 54 , 1937–1967 (2021).
Chen, T. et al. Xgboost: extreme gradient boosting. R Package Version 04–2 . 1 (4), 1–4 (2015).
Zhang, Z. Introduction to machine learning: k-nearest neighbors. Ann. Transl. Med. 4 (11), 382-393 (2016).
Ali, M. M. et al. Heart disease prediction using supervised machine learning algorithms: performance analysis and comparison. Comput. Biol. Med. 136 , 104672 (2021).
Dhall, D., Kaur, R. & Juneja, M. Machine learning: a review of the algorithms and its applications. Proceedings of ICRIC. : Recent Innovations in Computing. 2020:47–63. (2019).
Austin, P. C., Tu, J. V., Ho, J. E., Levy, D. & Lee, D. S. Using methods from the data-mining and machine-learning literature for disease classification and prediction: a case study examining classification of heart failure subtypes. J. Clin. Epidemiol. 66 (4), 398–407 (2013).
Luo, W. et al. Guidelines for developing and reporting machine learning predictive models in biomedical research: a multidisciplinary view. J. Med. Internet. Res. 18 (12), e323 (2016).
Bowles, M. Machine Learning in Python: Essential Techniques for Predictive Analysis (Wiley, 2015).
Jiang, T., Gradus, J. L. & Rosellini, A. J. Supervised machine learning: a brief primer. Behav. Ther. 51 (5), 675–687 (2020).
Xu, Y. & Goodacre, R. On splitting training and validation set: a comparative study of cross-validation, bootstrap and systematic sampling for estimating the generalization performance of supervised learning. J. Anal. Test. 2 (3), 249–262 (2018).
Kung, S. Y. Kernel Methods and Machine Learning (Cambridge University Press, 2014).
Kumbhare, T.A. and Chobe, S.V. An overview of association rule mining algorithms. International Journal of Computer Science and Information Technologies. 5 (1), 927-930 (2014).
Hussein, N., Alashqur, A. & Sowan, B. Using the interestingness measure lift to generate association rules. J. Adv. Comput. Sci. Technol. 4 (1), 156 (2015).
Bao, F., Mao, L., Zhu, Y., Xiao, C. & Xu, C. An improved evaluation methodology for mining association rules. Axioms . 11 (1), 17 (2021).
Council, N. R. Frontiers in Massive data Analysis (National Academies, 2013).
Council, N. R. Statistical Analysis of Massive Data Streams: Proceedings of a Workshop: National Academies Press; (2004).
Nohara, Y., Matsumoto, K., Soejima, H. & Nakashima, N. Explanation of machine learning models using shapley additive explanation and application for real data in hospital. Comput. Methods Programs Biomed. 214 , 106584 (2022).
Chen, R-C., Dewi, C., Huang, S-W. & Caraka, R. E. Selecting critical features for data classification based on machine learning methods. J. Big Data . 7 (1), 52 (2020).
Chilyabanyama, O. N. et al. Performance of machine learning classifiers in classifying stunting among under-five children in Zambia. Children . 9 (7), 1082 (2022).
Kebede, S. D. et al. Prediction of contraceptive discontinuation among reproductive-age women in Ethiopia using Ethiopian demographic and Health Survey 2016 dataset: a Machine Learning Approach. BMC Med. Inf. Decis. Mak. 23 (1), 1–17 (2023).
MathSciNet Google Scholar
Stockman, J., Friedman, J., Sundberg, J. & Harris, E. Predictive analytics using machine learning to identify ART clients at health system level at greatest risk of treatment interruption in Mozambique and Nigeria. JAIDS J. Acquir. Immune Defic. Syndr. 8 (6), 10-97 (2022).
Alonso, E. B. The impact of culture, religion and traditional knowledge on food and nutrition security in developing countries. (2015).
Download references
Acknowledgements
We would like to thank the measure DHS program for providing the dataset.
The author(s) received no specific funding for this work.
Author information
Authors and affiliations.
Department of Health Informatics, School of Public Health, College of Medicine and Health Sciences, Woldia University, PO Box 400, Woldia, Amhara, Ethiopia
Habtamu Setegn Ngusie
Department of Health Informatics, College of Medicine and Health Science, Wollo University, Desie, Ethiopia
Ermias Bekele Enyew & Mulugeta Desalegn Kasaye
Department of Health Informatics, College of Medicine and Health Science, Debre Berhan University, Debre Berhan, Ethiopia
Agmasie Damtew Walle
Department of Health Informatics, College of Health Science, Debre Markos University, Debre Markos, Ethiopia
Bayou Tilahun Assaye
School of Public Health, Dilla University, Dilla, Ethiopia
Getanew Aschalew Tesfa
Department of Pediatrics and Child Health Nursing, School of Nursing, College of Medicine and Health Science, Woldia University, Woldia, Ethiopia
Alemu Birara Zemariam
You can also search for this author in PubMed Google Scholar
Contributions
HSN, EBE, ADW, and ABZ were involved in the conception, design, data collection, supervision, investigation, data analysis, interpretation, and writing of the manuscript. BT, MDK, and GAT contributed to data extraction, preprocessing, proposal development, validation, manuscript revision, figure preparation, data analysis, visualization, and interpretation. All authors (HSN, EBE, ADW, BT, MDK, GAT, and ABZ) reviewed and approved the final manuscript.
Corresponding author
Correspondence to Habtamu Setegn Ngusie .
Ethics declarations
Competing interests.
The authors have declared that no competing interests exist.
Ethics approval and consent to participate
We obtained approval from the DHS Program to access and utilize their data for our study.
Consent for publication
Not applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ngusie, H.S., Enyew, E.B., Walle, A.D. et al. Employing machine learning techniques for prediction of micronutrient supplementation status during pregnancy in East African Countries. Sci Rep 14 , 23827 (2024). https://doi.org/10.1038/s41598-024-75455-5
Download citation
Received : 20 December 2023
Accepted : 04 October 2024
Published : 11 October 2024
DOI : https://doi.org/10.1038/s41598-024-75455-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Micronutrient supplementation
- Pregnant women
- Demographic health survey
- Machine learning algorithms
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Spike in emergency visits for life threatening pregnancy complication, study suggests
Findings suggest significant increase in emergency department utilization for hypertensive disorders of pregnancy over 14 year span.
Hypertensive disorders of pregnancy, the second leading cause of maternal deaths worldwide, may be sending a significantly higher number of pregnant people to the emergency department.
Between 2006 and 2020, researchers found a surge in emergency visits and admissions for the condition that causes serious maternal and neonatal complications and accounts for 6.3% of all pregnancy-related deaths in the United States.
The study, which appears in JAMA Network Open , also suggests greater emergency utilization for the disease among underrepresented racial and ethnic groups.
"Hypertensive disorders of pregnancy often develop suddenly, even in healthy women, and symptoms may appear without warning and progress rapidly," said senior author Erica Marsh, M.D., professor of obstetrics and gynecology at the University of Michigan Medical School and chief of the division of reproductive endocrinology and infertility at U-M Health Von Voigtlander Women's Hospital, of Michigan Medicine.
"Ideally, this risk would be detected during prenatal care and lead to early intervention. Our study indicates more people turning to the emergency department, which may reflect a higher prevalence of the condition or an increased awareness for prompt assessment and treatment."
Hypertensive disorders of pregnancy, which could include preeclampsia, gestational hypertension, and eclampsia, are serious complications that involve elevated blood pressure.
The American College of Obstetricians and Gynecologists recommends management of severe blood pressure in pregnancy within 30 to 60 minutes of diagnosis to prevent complications such as stroke, myocardial ischemia, seizure, placental abruption, and maternal and neonatal mortality.
Disparities in ED reliance, disease severity
Researchers analyzed nationally representative data, finding a 76% increase in emergency encounters related to the condition over the 14-year span, up from 31,623 to 55,893, and nearly 1.5 times as many ED admissions -- up from 17,338 to 43,563.
Concerns about costs, time constraints, misconceptions about the necessity of early care or barriers to accessing prenatal care may be possible factors for the increase, authors say.
"The disparities in reliance on emergency rooms for this disease may imply limited access to timely outpatient care or other health system barriers," said lead author Courtney Townsel, M.D., M.Sc., who was at Michigan Medicine at the time of the study and is now at the University of Maryland.
Black, Hispanic, and Asian or Pacific Islander groups were also more likely to both utilize emergency care and be admitted to the hospital for hypertensive disorders of pregnancy.
"The disproportionate rate of admissions among certain racial and ethnic groups suggests worse disease severity by the time people seek care," Townsel said.
"Racial differences in emergency care utilization for hypertensive disorders of pregnancy underscore the ongoing racial disparities in U.S. maternal morbidity and mortality and highlight a critical need for accessible, culturally competent community-level interventions for all."
- Today's Healthcare
- Pregnancy and Childbirth
- Diseases and Conditions
- Teen Health
- Healthy Aging
- Nutrition and pregnancy
- Fetal alcohol spectrum disorder
- Air pollution
- Whooping cough
- Emergency management
Story Source:
Materials provided by Michigan Medicine - University of Michigan . Original written by Beata Mostafavi. The original text of this story is licensed under a Creative Commons License . Note: Content may be edited for style and length.
Journal Reference :
- Courtney Townsel, LeAnn Louis, Chelsie Clark, Leah Mitchell Solomon, Charley Jiang, Martina Caldwell, Erica E. Marsh. Emergency Department Utilization for Hypertensive Disorders of Pregnancy and Post Partum, 2006-2020 . JAMA Network Open , 2024; 7 (9): e2433045 DOI: 10.1001/jamanetworkopen.2024.33045
Cite This Page :
Explore More
- Single-Atom Editing Tech Developed
- Electron 'Pinball' in Space After Lightning
- Playing Songs to Darwin's Finches: New Species
- New Tech Improves Structural Strength
- 3D Printing Method: Unique Objects Quickly
- 'Inside-Out' Galaxy Growth in Early Universe
- Dance, Gibbon, Dance!
- 19th Century Lions from Kenya Ate Humans
- Chaotic 3-Body Problem: Islands of Regularity
- Bilingualism Makes the Brain More Efficient
Trending Topics
Strange & offbeat.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
WHO antenatal care recommendations for a positive pregnancy experience: Nutritional interventions update: Multiple micronutrient supplements during pregnancy [Internet]. Geneva: World Health Organization; 2020.

WHO antenatal care recommendations for a positive pregnancy experience: Nutritional interventions update: Multiple micronutrient supplements during pregnancy [Internet].
Introduction.
The comprehensive antenatal care (ANC) guideline, WHO recommendations on antenatal care for a positive pregnancy experience , was published by the World Health Organization (WHO) in 2016 with the objective of improving the quality of routine health care that all women and adolescent girls receive during pregnancy ( 1 ). The overarching principle – to provide pregnant service users with a positive pregnancy experience – aims to encourage countries to expand their health-care agendas beyond survival, with a view to maximizing health, human rights and the potential of their populations. Recognizing that ANC provides a useful platform for important health-care functions, including health promotion and disease prevention, 14 out of the 49 recommendations in the WHO ANC guideline relate to nutrition in pregnancy ( 1 ).
In April 2019, following pre-established prioritization criteria, the Executive Guideline Steering Group (GSG) prioritized updating of the recommendation on multiple micronutrient supplements (MMS). This resulting recommendation updates and supersedes the previous recommendation on antenatal MMS issued in the 2016 WHO ANC guideline.
Pregnancy and micronutrients
Pregnancy requires a healthy diet that includes an adequate intake of energy, protein, vitamins and minerals to meet increased maternal and fetal needs. However, for many pregnant women, dietary intake of fruit, vegetables, meat and dairy products is often insufficient to meet these needs, and may lead to micronutrient deficiencies. In resource-poor countries in sub-Saharan Africa, south-central Asia and south-east Asia, maternal undernutrition is highly prevalent and is recognized as a key determinant of poor perinatal outcomes ( 5 ). However, understanding of the individual requirements and contributions of all essential vitamins and minerals to optimize maternal and fetal health during the antenatal period is limited ( 6 ).
Maternal iron deficiency is the most common known micronutrient deficiency that causes anaemia. Anaemia is estimated to affect 40% of pregnant women globally, with the highest prevalence in the WHO regions of South-East Asia (49%), Africa (46%) and the Eastern Mediterranean (41%). A lower prevalence is estimated in the WHO regions of the Western Pacific (33%), the Americas (26%) and Europe (27%) ( 7 ). Supplementation with iron during pregnancy is therefore considered essential ( 1 , 6 ). Daily folic acid is also recommended as a routine antenatal supplement to prevent fetal neural tube defects ( 1 ). Iron and folic acid (IFA) are often combined in a single tablet, such as the daily IFA supplement of the United Nations Children’s Fund (UNICEF), which may include 30 mg or 60 mg elemental iron and 0.4 mg folic acid ( 8 , 9 ). They are also included in the United Nations International Multiple Micronutrient Antenatal Preparation (UNIMMAP), an established multiple micronutrient formulation that is widely available and contains 15 micronutrients, including IFA in doses of 30 mg and 0.4 mg, respectively ( 10 ).
For populations with low dietary intake of calcium, antenatal calcium supplementation is also recommended by WHO to prevent pre-eclampsia ( 1 , 11 ). In addition, in certain populations at risk of night blindness, vitamin A supplementation during pregnancy is recommended ( 1 ).
The updated recommendation in the context of the WHO ANC guideline
- What are the effects of MMS containing at least 13 to 15 micronutrients (including IFA) compared with IFA supplements?
- What are the effects of UNIMMAP compared with IFA supplements?
The GDG also requested additional subgroup analyses according to the dose of iron in the control group because most trials in the review evaluated MMS containing 30 mg of elemental iron, and this was compared with IFA controls that employed either 30 mg or 60 mg of iron. Similarly, as the existing WHO recommendation on IFA supplements recommends a folic acid dose of 0.4 mg, the GDG requested additional analyses restricting trials to those comparing MMS to these IFA doses. The rationale for these additional analyses was that, if countries are to consider transitioning to MMS, they would most likely be switching from one of these two IFA formulations (i.e. 30 mg iron/0.4 mg folic acid or 60 mg iron/0.4 mg folic acid).
In 2016, the resulting evidence suggested that MMS (containing 13 to 15 micronutrients, including IFA) were associated with an average 11% reduction in low birthweight compared with IFA supplements. However, lack of other beneficial effects, the added cost of MMS, equivocal evidence on neonatal mortality related to the dose of iron in IFA supplements, possibility of unknown harms, lack of evidence on cost-effectiveness, and concerns about feasibility led the GDG to decide not to recommend a change from existing IFA supplements strategies at the time ( 1 ).
Since the publication of the WHO ANC guideline, the Cochrane review has been updated to include four additional trials ( 13 ). This framework presents the updated research evidence on antenatal MMS compared with IFA supplements, which supports the updated recommendation on MMS.
- Rationale and objectives
As part of the WHO’s normative work on supporting evidence-informed policies and practices and its living guidelines approach ( 14 ), the Department of Sexual and Reproductive Health and Research (SHR), the Department of Maternal, Newborn, Child, Adolescent Health and Ageing (MCA) and the Department of Nutrition and Food Safety (NFS) prioritized the updating of this recommendation on MMS following the advice of the Executive GSG 2017–2019, particularly the identification of new evidence on this intervention.
- Target audience
The recommendation in this global guideline is intended to inform the development of relevant national- and local-level health policies and clinical protocols. Therefore, the target audience of this guideline includes national and local public health policy-makers, implementers and managers of national and local maternal and child health programmes, concerned nongovernmental and other organizations, professional societies involved in the planning and management of maternal and child health services, health professionals (including obstetricians, midwives, nurses and general medical practitioners) and academic staff involved in training health professionals.
- Scope of the recommendations
This updated recommendation is relevant to all pregnant women and adolescent girls receiving ANC in any health-care facility or community-based setting, and to their unborn fetuses and newborns. The question was prioritized during the ANC guideline development process. In 2019, it was prioritized for updating in the context of WHO’s living guideline commitment ( 14 ). The authors of the Cochrane review on which the 2016 ANC guideline panel’s recommendation was based updated their review to include new studies. The outcomes of interest are therefore the same as those prioritized for the ANC guideline relevant to nutritional interventions (see Box 1 ).
Box 1 ANC nutritional interventions outcomes of interest
View in own window
Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders . To submit requests for commercial use and queries on rights and licensing, see https://www.who.int/about/who-we-are/publishing-policies/copyright .
Third-party materials. If you wish to reuse material from this work that is attributed to a third party, such as tables, figures or images, it is your responsibility to determine whether permission is needed for that reuse and to obtain permission from the copyright holder. The risk of claims resulting from infringement of any third-party-owned component in the work rests solely with the user.
Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo ).
Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”.
Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization ( http://www.wipo.int/amc/en/mediation/rules/ ).
- Cite this Page WHO antenatal care recommendations for a positive pregnancy experience: Nutritional interventions update: Multiple micronutrient supplements during pregnancy [Internet]. Geneva: World Health Organization; 2020. Introduction.
- PDF version of this title (3.7M)
In this Page
Other titles in this collection.
- WHO Guidelines Approved by the Guidelines Review Committee
Related WHO publication
- WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience
- WHO antenatal care recommendations for a positive pregnancy experience: Nutritional interventions update: Vitamin D supplements during pregnancy
- WHO antenatal care recommendations for a positive pregnancy experience: Maternal and fetal assessment update: imaging ultrasound before 24 weeks of pregnancy
- WHO antenatal care recommendations for a positive pregnancy experience: Nutritional interventions update: zinc supplements during pregnancy
Recent Activity
- Introduction - WHO antenatal care recommendations for a positive pregnancy exper... Introduction - WHO antenatal care recommendations for a positive pregnancy experience
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
recommended number of visits. Adequate prenatal care is care beginning in the first 4 months of pregnancy with at least 80%- 109% of the recommended number of visits. Adequate plus care is care beginning in the first 4 months of pregnancy with 110% or more of the recommended visits (8, 10). A prenatal care visit is defined as one in which the ...
Eight or more contacts for antenatal care can reduce perinatal deaths by up to 8 per 1000 births when compared to 4 visits. A woman's 'contact' with her antenatal care provider should be more than a simple 'visit' but rather the provision of care and support throughout pregnancy. The guideline uses the term 'contact' as it implies ...
Chapter 6 Antepartum Care 149 Prenatal Care Visits 150 Routine Antepartum Care 154 Special Populations and Considerations 205 Second-Trimester and Third-Trimester Patient Education 211 ... Medical Complications Before Pregnancy 301 Pregnancy-Related Complications 330 Chapter 10 Care of the Newborn 347 Delivery Room Care 348 ...
The percentage of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times. Due to data limitations, it is not possible to determine the type of provider for each visit. Numerator: the number of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times.
Early antenatal care visit: a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. The Lancet Global Health. 2017; 5 (10):e977-e83. 10.1016/S2214-109X(17)30325-X [PMC free article] [Google Scholar]
Antenatal care (also termed prenatal care) is one of the most common preventive health services in the United States, accessed by about 4 million women annually.1 Antenatal care aims to improve the health and wellbeing of pregnant patients and their babies through (1) medical screening and treatment; (2) anticipatory guidance; and (3) psychosocial support.2, 3 The World Health Organization's ...
In Sub-Saharan Africa, 49-53% of women received the minimum recommended number of ANC visits 35% accessed at least one visit and 13% of women had no antenatal care visits . Due to the high burden of maternal and child mortality, WHO adopted the focused antenatal care model by the year 2002, which recommends a minimum of four antenatal care ...
Antenatal care is a cornerstone of obstetric practice in the United States, and millions of patients receive counseling, screening, and medical care in these visits. 2, 3 There is clear evidence ...
Antenatal care coverage (at least four visits) is the percentage of women aged 15 to 49 with a live birth in a given time period that received antenatal care four or more times. Available survey data on this indicator usually do not specify the type of the provider; therefore, in general, receipt of care by any provider is measured.
An antenatal visit refers to pregnancy care provided by skilled health personnel (doctors, nurses or midwives). ... (Number of women aged 15-49 attended at least four times during pregnancy by any provider for reasons related to the pregnancy/total number of women aged 15-49 with a live birth) *100. The ANC4+ indicator is based on a standard ...
The number of ANC contacts with physicians, nurses, and midwives was divided into 2 groups: those who had fewer than 8 ANC contacts and those who had 8 or more ANC contacts. ... Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: a finding based on a demographic and health survey. BMC Pregnancy ...
Number of antenatal visits is grouped into categories of no antenatal visits, 1 visit, 2 visits, 3 visits, 4-7 visits, 8+ visits, and "don't know" before calculating percentages. ... "Don't know" or missing values on number of antenatal care visits and timing of first ANC are excluded from numerators but included in denominators. ...
Background. Approximately 303,000 women and adolescent girls died from pregnancy and childbirth-related complications in 2015.1 That same year, 2.6 million babies were stillborn. Almost all of the maternal deaths (99%) and child deaths (98%) occurred in low- and middle-income countries.
Background Antenatal care is one of the best strategies for maternal and neonatal mortality reduction. There is a paucity of evidence on the mean number of ANC visits and associated factors in Sub-Saharan Africa (SSA). This study aimed to investigate the mean number of ANC visits and associated factors among reproductive-age women in Sub-Saharan Africa using the Demographic and Health Survey ...
Overview . This comprehensive WHO guideline provides global, evidence-informed recommendations on routine antenatal care. The guidance aims to capture the complex nature of the issues surrounding ANC health care practices and delivery and to prioritize person-centred health and well-being, not only the prevention of death and morbidity, in accordance with a human rights-based approach.
All women-baby dyads should, as a minimum, receive all three contacts of care to receive basic antenatal, delivery and postnatal interventions. The median percentage for the 88 countries, however, was that only 57% women-baby dyads received all three: four antenatal care visits, institutional delivery care, and postnatal care visit within two ...
Antenatal care (ANC) is the care of the woman during pregnancy. The primary aim of ANC is to promote and protect the health of women and their unborn babies during ... Frequency of postpartum visits The general recommendation for Sudan is that, with limited resources, a contact with health care system at least during the first twenty-four
Background Receiving quality antenatal care (ANC) from skilled providers is essential to ensure the critical health circumstances of a pregnant woman and her child. Thus, this study attempted to assess which risk factors are significantly associated with the timing of antenatal care and the number of items of antenatal care content received from skilled providers in recent pregnancies among ...
Moderate quality evidence from 2 RCTs (N=1520) showed that there is a clinically important difference favouring standard care versus a reduced number of appointments on the number of women who reported number of antenatal visits as 'not quite enough' or 'too few': RR 6.28 (95% CI 3.66 to 10.80). Very low quality evidence from 2 RCTs (N ...
Despite the positive impact of adhering to the new antenatal care model on pregnancy outcomes and maternal health service uptake, women in resource-limited settings exhibit low levels of compliance with this recommendation. Previous studies on women's adherence to the new antenatal care recommendation have been limited to individual countries, with no evidence available at Sub-Saharan Africa ...
Method of estimation: Data represent responses from the WHO Sexual, Reproductive, Maternal, Newborn, Child and Adolescent Health Policy Survey, 2018-2019. Survey response options included: Less than 4 visits; At least 4 visits; At least 8 visits; Unknown.
Key predictors of micronutrient supplementation were the mother's education level, employment status, number of antenatal care (ANC) visits, access to media, number of children, and religion.
Between 2006 and 2020, researchers found a surge in emergency visits and admissions for the condition that causes serious maternal and neonatal complications and accounts for 6.3% of all pregnancy ...
The comprehensive antenatal care (ANC) guideline, WHO recommendations on antenatal care for a positive pregnancy experience, was published by the World Health Organization (WHO) in 2016 with the objective of improving the quality of routine health care that all women and adolescent girls receive during pregnancy (1). The overarching principle - to provide pregnant service users with a ...
1st trimester Visit 1: 8-12 weeks 1 Contact 1: up to 12 weeks 1 Contact 2: 20 weeks 2nd trimester Visit 2: 24-26 weeks 1 2 Contact 3: 26 weeks Contact 4: 30 weeks Visit 3: 32 weeks 1 Contact 5: 34 weeks 3rd trimester Contact 6: 36 weeks 5 Visit 4: 36-38 weeks 1 Contact 7: 38 weeks Contact 8: 40 weeks. Return for delivery at 41 weeks if ...
The percentage of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times. Due to data limitations, it is not possible to determine the type of provider for each visit. Numerator: the number of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times.
Association between quality of antenatal care service utilization and adverse birth outcomes among adolescent women in 22 Sub-Saharan African countries. A mixed-effects multilevel analysis ... Provision of comprehensive, essential, and minimal care packages of ANC service on each ANC visit is very crucial in mitigating unfavourable birth ...