Free Standard UK Delivery for orders over �35
Click & Collect now available!

4.7 out of 5 on Trustpilot from over 85,000 reviews

Kwells Travel Health Care
- Travel Sickness (2)
- Travel Medicines (1)
- Childrens Medicines (1)
- Stomach & Bowel Medicines (2)
- Pharmacy Medicines (2)
- Children's Medicine (1)
- Summer Wellness (2)
- Summer Shop (2)
Kwells medicines are indicated to prevent travel sickness. Kwells can be used by both kids (above 4 years) and adults.
Kwells is used to prevent all types of Travel Sickness (car, coach, plane, train and ship) and is suitable for use in adults and children over the age of 4 years, (dose adjustments are needed for children between 4-12 yrs of age).
Kwells travel sickness prevention contains the active ingredient Hyoscine Hydrobromide (0.3mg) and does not contain caffeine (a stimulant) or Dimenhydrinate (may cause drowsiness), which are found in other travel sickness treatments.
Kwells is the No.1 selling treatment for travel sickness prevention.
Kwells should be taken at least 30 minutes before commencing your journey as travel sickness is more easily prevented than treated - once vomiting occurs it is almost impossible for oral medication to be absorbed into the body.
FAQ’s Q: Are there preservatives in Kwells? A: There are no preservatives present in Kwells. Q: What active ingredients are in Kwells? A: The active ingredient is Hyoscine hydrobromide. Kwells does not contain caffeine or dimenhydrinate. Q: I get nervous prior to flying and feel airsick when the plane is flying. What can I do? A: The best solution is to take travel sickness prevention 30 minutes prior to flying and when checking ask to be seated over a wing. When on the plane also open the air vent to allow fresh air to flow over your face.
Q: When traveling by car the kids frequently become air sick. What can I do? A: The best solution is to treat them with travel sickness prevention 30 mins prior to the journey. Kwells can be used for children 4 years and up (refer to pack for dosage instructions). In addition ensure they have eaten 2-3 hours before travelling and drink water during the journey. When driving they should be safely elevated to allow them to see where they are going.
Sign up to our newsletter and get the latest deals, exclusive offers, health advice from our online doctor and much more.
- Child Health
- Heart Health
- Men's Health
- Mental Health
- Sexual Health
- Skin Conditions
- Travel Vaccinations
- Treatment and Medication
- Women's Health
- View all categories
- Bones and Joints
- Digestive Health
- Healthy Living
- Signs and Symptoms
Try our Symptom Checker Got any other symptoms?
- Nervous System
- Heart Disease
- Inflammation
- Painkillers
- Muscle Pain
- View all Medicines and Drugs
- Type 2 Diabetes
- Bacterial Vaginosis
- View all Treatments
- BMI Calculator
- Pregnancy Due Date Calculator
- Screening Tests
- Blood Tests
- Liver Function Tests
- Am I Pregnant?
- Am I Depressed?
- View all Tools
- Latest Features
- Health Videos
- Bronchiolitis
- Molluscum Contagiosum
- Actinic Keratosis
- Abdominal Pain in Children
- Subdural Haematoma
- Obesity in Adults
- View all Pro Articles
- View all Medical Calculators
- Login / Register
- Patient Access
- Health Info
- Health Advice for Travel Abroad
How to manage motion sickness
Remove from Saved
Have you ever felt sick or dizzy in a moving vehicle? Perhaps you've also broken out in a cold sweat, felt weak, or developed a headache at the same time? Motion sickness may be common, but this doesn't mean you can't prevent or treat it.
Why am I getting motion sickness?
Motion sickness - also called travel sickness - can affect anyone, and most people have experienced it at some point in their lives. This is especially true during childhood. In fact, some studies suggest that more than 40% of children get motion sick in a car or on a bus 1 .
Why does this happen? It's all to do with the signals that are sent to your brain while you're in motion. The unusual movements you feel while travelling send lots of messages to the brain, including from mechanisms in your inner ear that send information about your position.
However, your eyes can contradict these messages if they're focused on objects that aren't moving, like the inside of a car. This results in a confusing mix of messages, and it's this confusion that causes motion sickness.
How to stop motion sickness
You might be particularly vulnerable to motion sickness. Scientists aren't clear why it can affect some more than others, but this doesn't mean that you can't prevent, ease, or eradicate this unpleasant and inconvenient sensation. The techniques below are usually highly effective and most are non-medical.
1. Eat light before your travel
If you know that you're heading on a car journey, catching the bus, boarding a plane or boat, or riding a fairground ride, be mindful of what you eat and when. Alcohol and heavy meals - especially fatty and spicy food - can upset your stomach, making motion sickness worse. Instead, opt for light meals at least an hour before travelling to give your food time to digest.
2. Plan where you sit
In a vehicle, where you position yourself matters. Always try and face forward and sit as far away as possible from the jittering movements and potent smells of an engine.
To keep motion to a minimum in a:
- Car - sit in the front.
- Bus - sit by a window.
- Train - sit forward-facing by a window.
- Boat - sit on the upper deck in the middle.
- Plane - sit over the wing.
3. Break long car journeys up
If you're planning a long car journey, it's a good idea to take regular breaks. Getting out the car and taking a short walk in the fresh air gives your brain a break from the mixed signals its receiving about your movement and balance.
4. Put down that book or electronic screen
Focussing your eyes on something that isn't moving while other mechanisms are sensing that you're in motion is a big trigger for motion sickness. This is why many people find they can't read books or watch films for long before feeling sick. Avoid too much electronic screen time - even when you're not travelling, screen scrolling can trigger something similar to motion sickness called cybersickness 2 .
5. Find different stimulants in the vehicle
How else can you entertain yourself? Looking forward at a fixed point, like a horizon, may help prevent motion sickness, but if you need more mental stimulation, you could try listening to music, a podcast, or an audio book with your eyes closed. Not only will this avoid sending confusing signals from your eyes to your brain, but sounds may also distract your brain and reduce sensitivity to these signals.
6. Rest your eyes
If you find resting easy while on the move, keeping your eyes closed is one of the most effective ways to halt the symptoms of motion sickness. Sleeping is even better - alongside shutting off signals from your eyes to your brain, a sleeping brain may also be able to ignore some of the disruptive motion signals it's receiving.
7. Locate fixed points outside the vehicle
When looking out a window or on a boat deck, fix your gaze on something that isn't moving. Watching trees and other cars go by outside a window - or waves roll by on a boat deck - can make motion sickness worse. That isn't to say that you should avoid gazing out altogether - if you feel seasick inside a boat, stepping out onto the deck and finding a fixed point on the horizon can help rectify the mismatch of signals in your brain that tell you you're moving without a visual reference 3 .
LGBTQ+ travel: how to stay safe
Whether you're choosing your next holiday destination, planning a backpacking route, or attendin...

Will Brexit affect my travel insurance?

How to have a healthy flight
8. breathe in fresh air.
When travelling by road, rail, or seadrink in fresh air as often as possible. Usually, this means sitting by an open window - but be careful to avoid strong petrol or diesel fumes.
9. Focus on your breathing
Some studies show that diaphragmic breathing - taking deep and slow breathes in and out - can help ease the unpleasant side effects of travelling 4 . It's a simple enough technique, but you can learn the most effective way to do it here .
10. Soothe an unsettled tummy
When it comes to treating motion sickness, what you feed your tummy matters. Taking small sips of cold water can help. Some natural food flavourings can also settle your stomach and relieve symptoms:
- Ginger flavoured snacks or drinks - effective for all symptoms of motion sickness 5 .
- Peppermint flavoured snacks or drinks - have a numbing and calming effect that helps ease nausea and headaches 6 .
11. Try over-the-counter medicines
If these natural techniques aren't enough, your local pharmacy will have motion sickness medicine. This ranges from homeopathic remedies, like acupressure wrist bands, to tablets and patches that usually contain the ingredients hyoscine and antihistamines . Hyoscine is considered the most effective medicine for motion sickness.
If you're getting medicine for your child, ask your pharmacist which brands are suitable for children, and about any side effects.
When to see a doctor for motion sickness
In nearly all cases, motion sickness naturally stops once your journey is over. You should visit your doctor if:
- You're still experiencing symptoms long after the journey has ended.
- You feel like you have motion sickness when you haven't been moving.
- You're experiencing other symptoms like chest pain or hearing loss.
Your doctor can work out if your motion sickness is particularly severe and may be able to prescribe stronger medicines . They can also investigate if your symptoms are a sign of another health problem that needs addressing.
Further reading
- Henriques et al: Motion sickness prevalence in school children .
- Iowa State University: Screentime can maje you feel sick – here are ways to manage cybersickness .
- The Vision Therapy Center: The surprising reason why you suffer from motion sickness .
- Stromberg et al: Diaphragmatic breathing and its effectiveness for the management of motion sickness .
- Nunes et al: Clinical evaluation of the use of ginger extract in the preventive management of motion sickness .
- Mohr et al: Peppermint essential oil for nausea and vomiting in hospitalized patients: incorporating holistic patient decision making into the research design .
Are you protected against flu?
See if you are eligible for a free NHS flu jab today.
Join our weekly wellness digest
from the best health experts in the business
Related Information
- What jet lag really does to your body
- Altitude Sickness
- Travelling to Remote Locations
- Ears and Flying (Aeroplane Ear)

Hi i have broken my Left wrist which was plated and also have screws in it i had a cast on for 6 weeks and have been out of a full cast for 2weeks my fingers are swollen i cannot make a fist and my... joanna01501
Feeling unwell?
Assess your symptoms online with our free symptom checker.
Disclaimer: This article is for information only and should not be used for the diagnosis or treatment of medical conditions. Egton Medical Information Systems Limited has used all reasonable care in compiling the information but make no warranty as to its accuracy. Consult a doctor or other health care professional for diagnosis and treatment of medical conditions. For details see our conditions .
We earn a commission for products purchased through some links in this article.
Sea-legs (discontinued in the UK)
This antihistamine can be bought without a prescription for travel sickness - read on for advice on its use, warnings and side effects
What is Sea-legs used for?
- Preventing and treating travel sickness in adults and children aged two years and over.
How does Sea-legs work?
Sea-legs tablets contain the active ingredient meclozine hydrochloride, which is a type of medicine called an antihistamine.
Meclozine works by stopping histamine from binding to its receptors in an area in the brain known as the vomiting centre. The vomiting centre is responsible for causing feelings of sickness and for the vomiting reflex. It is activated when it receives nerve messages from the vestibular apparatus in the middle ear.
The vestibular apparatus provides constant feedback to the brain about the position of our body. When something disturbs the vestibular apparatus, such as movements of the head when travelling by boat or car, nerve signals are sent from the vestibular apparatus to the vomiting centre. This can cause the symptoms of motion sickness, such as nausea, dizziness or spinning sensations (vertigo) and vomiting.
By blocking the histamine receptors in the vomiting centre, meclozine prevents disturbances in the middle ear from activating the vomiting centre.
How do I take Sea-legs?
- Sea-legs tablets can help prevent travel sickness for up to 24 hours. A dose can be taken either an hour before travelling, or the evening before. Alternatively you can wait until feelings of sickness start before taking a dose, but this is likely to be less effective.
- The dose for adults and adolescents over 12 years of age is two tablets.
- The dose for children aged 6 to 12 years is one tablet.
- The dose for children aged 2 to 6 years is half a tablet.
- Don't use more than one dose in 24 hours.
- The tablets can be taken either with or without food. They should be swallowed with a drink.
What should I know before using Sea-legs?
- Sea-legs tablets can cause drowsiness and this may reduce your ability to drive or operate machinery safely. Do not drive or operate machinery until you know how this medicine affects you and you are sure it won't affect your performance. If your child is affected in this way they should avoid potentially hazardous activities such as riding bikes. You should not leave your child unattended after giving them this medicine.
- Avoid drinking alcohol while taking Sea-legs because this is likely to make any drowsiness worse.
- Children and elderly people are more likely to experience side effects such as drowsiness with this medicine.
- If you experience persistent vomiting that is not due to travel sickness, it is important to see a doctor. You should not continue to take Sea-legs, because vomiting is a symptom of various conditions and the tablets could delay early diagnosis.
Who shouldn't take Sea-legs?
- Children under two years of age.
- Women who are pregnant or breastfeeding.
- People with hereditary blood disorders called porphyrias.
- People who are allergic to any ingredients of the tablets.
Who should get medical advice before taking Sea-legs?
- People with asthma , bronchitis , or a condition called bronchiectasis in which there is persistent and progressive widening of the airways due to lung infections or lung disease, such as cystic fibrosis .
- People with closed angle glaucoma .
- People with kidney or liver problems.
- People who suffer from epilepsy .
- People with a blockage of the opening from the stomach into the intestines (pyloro-duodenal obstruction).
- People with problems passing urine, for example men with an enlarged prostate gland .
Can I take Sea-legs while pregnant or breastfeeding?
- You should not take Sea-legs tablets if you are pregnant or breastfeeding.
What are the possible side effects of Sea-legs?
Medicines and their possible side effects can affect individual people in different ways. The following are some of the side effects that are known to be associated with meclozine. Just because a side effect is stated here, it does not mean that all people using this medicine will experience that or any side effect.
- Drowsiness.
- Blurred vision.
- Difficulty passing urine.
- Constipation .
- Stomach acid reflux (heartburn).
- Thickened mucus in the airways.
Talk to your doctor, nurse or pharmacist or read the leaflet provided with the medicine if you want any more information about the possible side effects of Sea-legs. If you think you have experienced a side effect, did you know you can report this using the yellow card website ?
Can I take Sea-legs with other medicines?
If you are already taking any medicines, including those bought without a prescription and herbal medicines, you should check with your pharmacist before taking this medicine as well, to make sure that the combination is safe .
You are more likely to feel drowsy if you take Sea-legs with any of the following (which can also cause drowsiness):
- antipsychotics, eg haloperidol
- barbiturates, eg phenobarbital , amobarbital
- benzodiazepines, eg diazepam , temazepam
- sedating antihistamines, eg chlorphenamine , hydroxyzine
- sleeping tablets, eg zopiclone
- strong opioid painkillers, eg codeine , dihydrocodeine , morphine
- tricyclic antidepressants, eg amitriptyline .
There may be an increased risk of side effects such as dry mouth, blurred vision or difficulty passing urine, if you take Sea-legs with other medicines that can have antimuscarinic effects, such as the following:
- antiarrhythmic medicines for irregular heartbeats, eg disopyramide , propafenone , quinidine
- antihistamines, eg promethazine , brompheniramine , chlorphenamine , diphenhydramine , triprolidine (some of these are often found in over-the-counter cough and cold remedies)
- antimuscarinic medicines for Parkinson's symptoms, eg procyclidine , orphenadrine , trihexiphenidyl
- antimuscarinic medicines for urinary incontinence, eg oxybutynin , trospium , tolterodine
- antipsychotics, eg chlorpromazine , clozapine , thioridazine
- antispasmodics, eg atropine , propantheline , hyoscine butylbromide
- MAOI antidepressants, eg phenelzine
- muscle relaxants, eg baclofen
- tricyclic antidepressants, eg amitriptyline , clomipramine .
If you experience a dry mouth as a side effect of this medicine you may find that medicines that are designed to dissolve and be absorbed from under the tongue, eg sublingual glyceryl trinitrate (GTN) tablets, become less effective. This is because the tablets do not dissolve properly in a dry mouth. To resolve this, drink a mouthful of water before taking sublingual tablets.
Sea-legs tablets may oppose the effect of betahistine taken for Ménière's disease.
Antihistamines may also oppose the effect of histamine (used to treat leukaemia) and are not recommended for people having this treatment.
Other medicines containing the same active ingredient
- Traveleeze pastilles .
Last updated 04.07.2016

Travel Health
Travel vaccines, travel illnesses, nhs vaccination schedule, things to remember, illnesses and conditions, your health, reciprocal healthcare, travelling with children.
From pool safety to sun protection, these simple steps will help your children stay safe and healthy on holiday.
Pool safety
Children need to be watched constantly. Don’t depend on a lifeguard, who may not be trained to UK standards.
What to pack - Swimming aids, such as armbands, are great for playing in the water but can easily slip off. Therefore, you still need to keep an eye on your child.
- Actively supervise all young children near water.
- Choose pools that are fenced with locking gates.
- Even if a pool has a lifeguard, make sure you know where your children are and what they're doing in the water.
- Let children take swimming classes while on holiday. They're a great way of gaining water confidence and learning essential water safety skills.
Take the RoSPA Water Wise quiz .
Sun protection
Studies have found that sunburn during childhood can increase the risk of skin cancer later in life.
What to pack - Use at least a factor 15 sunscreen and choose a "broad-spectrum" brand that has a four- or five-star rating. Apply it to areas that cannot be protected by clothing, such as the face, ears, feet and backs of the hands. Choose sunscreens that are formulated for children and babies' skin.
- Apply sunscreen before children go outdoors.
- Sunscreen can easily be washed, rubbed or sweated off, so reapply it often throughout the day.
- Keep babies in complete shade, such as under trees, umbrellas, canopies or indoors.
- Protect a baby’s skin with loose-fitting clothes and a wide-brimmed hat that shades their face and neck.
- Make sure children drink regularly.
Travel sickness
Children often get motion sickness more than adults. Early symptoms of motion sickness include hot flushes, dribbling and paleness.
What to pack - Several medicines are available to reduce or prevent symptoms of motion sickness. You can buy them from pharmacies or get them on prescription. Anti-sickness remedies containing hyoscine are the most effective medicines for motion sickness. There are several brands of medicines containing hyoscine and they come as a soluble form for children.
- Avoid staring at moving objects, such as waves or other cars. Instead, look ahead a little above the horizon at a fixed place.
- Keep motion to a minimum. For example, sit over the wing of a plane or on deck in the middle of a boat.
- Avoid heavy meals before and during travelling. It may be a good idea to avoid spicy or fatty food.
- On long journeys, it may help to have a break and get some fresh air, drink some cold water and take a short walk.
- Ginger can improve motion sickness in some people. It can be taken in ginger biscuits, ginger tea or as tablets before a journey.

Related Links

- Resources for health professionals
- Medicines information
- Advice and guides
Travelling with medicines
This page provides general information to help you prepare for a trip and to give medicines whilst travelling.
- If your child is on a course of treatment or needs to take medicines regularly, it is important that you continue to give these whilst travelling or on holiday. This may be difficult while you are away from home and your usual routine, so you need to plan ahead.
- If you are going on a long trip, discuss this with your doctor, as you may need to make special arrangements for prescriptions and supplies of medicines.
- If your child has complex health needs and takes several medicines, talk to your healthcare professional before travelling.
- Information on individual medicines is available on the Medicines Information pages.
Travelling with medicines (116.9KB pdf)
View this leaflet as a PDF
Sharing health evidence you can trust

Treatments to prevent travel sickness: a quick look
In this short blog, Dr Robert Walton looks at the evidence on treatments to prevent travel sickness (motion sickness).
Take-home points
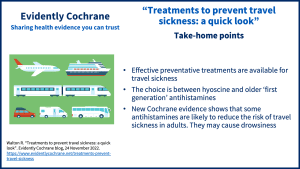
The new evidence on antihistamines comes from the Cochrane Review Antihistamines for motion sickness (published in October 2022) and is relevant to adults.
Travel sickness (motion sickness) is a common problem, and many people experience nausea for example on boats, planes or in the car. Lots of treatments which aim to prevent travel sickness are available to buy in UK pharmacies, including medicines. Here is the evidence on these medicines and some things you may want to think about when making your choices.
Making a choice? Think BRAIN!
It can be helpful to think BRAIN : What are the B enefits, R isks, A lternatives, what do I want and what if I do N othing? These can be good questions to talk about with a health professional when making a health decision.
Medicines to prevent travel sickness
The choice is between hyoscine (or scopolamine as it is sometimes called) and antihistamines such as cinnarizine.
Most of the Cochrane evidence Cochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. is focused on hyoscine which is probably better than placebo An intervention that appears to be the same as that which is being assessed but does not have the active component. For example, a placebo could be a tablet made of sugar, compared with a tablet containing a medicine. (dummy treatment Something done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. ) at preventing travel sickness. It comes from the Cochrane Review Scopolamine (hyoscine) for preventing and treating motion sicknes s (published June 2011).
The new Cochrane evidence about antihistamines, from the Cochrane Review Antihistamines for motion sickness (published October 2022) finds that they are likely to reduce the risk A way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. of travel sickness in adults who tend to get it, compared with taking a placebo.
It’s worth bearing in mind that there is evidence to support using older or ‘first generation’ antihistamines but none for the newer medicines such as loratadine and cetirizine which are more commonly used now for hay fever now. These newer antihistamines are not used to prevent or treat motion sickness and are unlikely to be effective.
There are few studies comparing the two types of medicines. There is little information about whether either are useful for treating motion sickness after it has started so prevention may be better than cure.
What are the risks?
Hyoscine and antihistamines both work in the same way for preventing travel sickness and they also share the same side effects which include drowsiness in some people.
What are the other options?
Many other options are available but there is no Cochrane evidence about their potential benefits and harms.
What do I want?
What matters (most) to you, and past experiences of a problem – and of treatments, is important when making treatment choices. If you usually get travel sickness and want to prevent it then there are medicines that can help and are backed up by Cochrane evidence. But it may be important to you to avoid the risk of side effects (such as drowsiness, if you have to drive for example). You could discuss your options and experience of treatments with a pharmacist.
What if I do nothing?
Travel sickness is usually not usually a big problem although some people can be quite severely affected. If you have had it once in a particular situation then you are likely to get it again.
Find out more
NHS pages on motion sickness
The Cochrane Reviews Cochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. :
Karrim N, Byrne R, Magula N, Saman Y. Antihistamines for motion sickness. Cochrane Database of Systematic Reviews In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. 2022, Issue 10. Art. No.: CD012715. DOI: 10.1002/14651858.CD012715.pub2.
Spinks A, Wasiak J. Scopolamine (hyoscine) for preventing and treating motion sickness. Cochrane Database of Systematic Reviews 2011, Issue 6. Art. No.: CD002851. DOI: 10.1002/14651858.CD002851.pub4.
Why you can trust this information
Join in the conversation on Twitter with @CochraneUK @rtwalton123 or leave a comment on the blog.
Please note, we cannot give specific medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact-check – or endorse – readers’ comments, including any treatments mentioned.
Robert Walton has nothing to disclose.

About Robert Walton
Robert Walton is a Cochrane UK Senior Fellow in General Practice. Robert qualified in medicine in London in 1983, having taken an intercalated degree in human pharmacology and immunology. He trained at St Georges Hospital, London and became a member of the Royal College of Physicians in 1986. His work applying computerised decision support to prescribing drugs in the Department of Public Health and Primary care in Oxford led to a doctoral thesis in 1998. Robert was elected a Fellow of the Royal College of General Practitioners in 1999 and the Royal College of Physicians in 2001. He became a Senior Investigator in the National Institute for Health Research (NIHR) in 2016. Robert is Clinical Professor of Primary Medical Care at Queen Mary and was joint lead of the NIHR Research Design Service east London team. His research interests are in primary care, genetics, clinical trials and personalised medicine. Robert led a five-year NIHR funded programme developing a novel training intervention to promote smoking cessation in pharmacies in east London which included a substantive Cochrane review and meta analysis on behaviour change interventions in community pharmacies and a large scale cluster-randomised clinical trial. His research team is also developing a smartphone game to promote smoking cessation and researching a personalised/stratified medicine approach to tobacco dependence using computerised decision support. He sat on the NIHR Programme Grants for Applied Research sub panel A and worked as an evaluator for the European Union Horizon 2020 programmes Global Alliance for Chronic Diseases and New Therapies for Rare Diseases and as a monitor for EU projects. Robert contributes to UK national guidance, and has served on the National Institute for Health and Care Excellence (NICE) Outcome Indicator and Technology Appraisals Committees.
is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International
1 Comments on this post
Dr. Walton, thank you for sharing your review. For children and those children with epilepsy, I have looked at their sensory processing to help prevent some of their motion sickness. There is a book “Understanding your Child’s Sensory Signals” by Angie Voss, OTR that helps families. I can also share with you my poster from the British Paediatric Neurology Association event in 2020 titled ” What are the perspectives and understanding of healthcare professionals including occupational therapists on treatment and care of babies with infantile spasms and early onset epilepsy- A qualitative design” if I have your email address.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Evidently Cochrane
Who can and cannot take hyoscine hydrobromide - Brand names: Kwells, Joy-Rides, Kwells Kids, Travel Calm, Scopoderm
Who can take hyoscine hydrobromide.
Hyoscine hydrobromide travel sickness tablets can be taken by most adults and children from the age of 3 years.
Patches for travel sickness can be used by most adults and children from the age of 10 years.
Who may not be able to take hyoscine hydrobromide
Hyoscine hydrobromide is not suitable for some people. To make sure it's safe for you, tell a pharmacist or doctor before taking it if you:
- have ever had an allergic reaction to hyoscine hydrobromide or any other medicine
- have an eye problem called primary angle closure glaucoma
- have difficulty peeing or a bowel blockage
- have myasthenia gravis , a condition that causes muscle weakness
- have heart problems, including a very fast heart rate
- have thyroid, kidney or liver problems
- have epilepsy (seizures)
- have digestive problems, such as acid reflux or severe constipation
- have ulcerative colitis
- have a high temperature
- are pregnant or trying to get pregnant, as hyoscine hydrobromide is not recommended in pregnancy
Page last reviewed: 5 October 2022 Next review due: 5 October 2025
This website uses cookies to ensure you get the best experience on our website. Learn more

Information on how to stay safe and healthy abroad. About us.
- General Travel Health Advice
Advice for Child Travellers
Vaccinations, food and water hygiene, accident prevention, medical services.
Travelling with children requires practical consideration and careful planning. It is advisable to consult a travel health practitioner at least 6-8 weeks in advance of departure. The risks to health vary and many factors need to be taken into account such as destination, length of stay, planned activities, age and the general health of your child.
Vaccinations may be advisable for some destinations. The age of your child often determines which vaccines they may be able to receive and should have already received as per the UK Vaccination Schedule . Parents should be aware that some children may be too young to receive the vaccinations recommended for their chosen destination. Your health care practitioner can discuss additional preventative measures to reduce the chance of disease transmission in these circumstances, however you may be advised to change your travel plans.
The timing of vaccinations is important, some vaccines may offer disease protection within two weeks, whereas others may require over a month. Some vaccine schedules require two or more doses given over weeks or months before adequate protection is obtained.
Some vaccines are available free on the NHS, however, there may be a charge for some recommended vaccines. This should be taken into consideration when planning and budgeting for travel.
Children are at particular risk of severe and fatal malaria; parents are therefore advised to avoid taking infants and children to malarious areas. If travel is unavoidable it is imperative that infants and children are well protected against mosquito bites and receive appropriate chemoprophylaxis (antimalarials) .
A) Awareness of Risk
Malaria is now predominantly a disease affecting Africa, South America, Southeast Asia, the Indian sub-continent and less so in Central America and the Middle East:
- individual country pages should be checked to determine the risk at the destination
- for further information see the malaria advice pages.
B) Mosquito Bite Prevention
- Parents and children must be aware of the risk and take precautions to avoid mosquito bites , including the use of repellents, nets and suitable clothing.
C) Chemoprophylaxis (antimalarials)
It is important to discuss antimalarial suitability with a qualified doctor, nurse or pharmacist:
- the choice of antimalarial is determined by the destination, age and weight of the child
- parents must supervise their child's antimalarial consumption and be careful not to exceed the recommended dose, overdosing antimalarials can be particularly toxic for children
- it is preferable to avoid crushing or breaking tablets, however, it may be necessary to crush some tablets in order to administer the correct dose. Qualified pharmacists should be able to offer further advice; tablet cutters can be purchased to help facilitate correct dosage
- infants and young children may resist taking medications, mixing tablets with jam, honey, chocolate spread or similar foods may make administration easier
- no antimalarial is 100% effective and should always be used in combination with mosquito bite avoidance
D) Diagnosis and Treatment
- Prompt diagnosis and treatment of malaria is essential and the importance of this should be stressed to all parents visiting malarious regions. Fever, occurring at least 7 days after exposure, is the most common symptom of malaria, but infection can develop even up to one year later.
- Symptoms in young children may be difficult to determine. Parents must be aware that any child returning from a malarious zone who seems ‘off colour’ or just ‘not their normal self’ should be screened for malaria promptly.
Rabies is spread through the saliva of an infected animal (particularly dogs, cats, monkeys and bats) via a bite, scratch or lick of mucous membranes or broken skin. There is no specific treatment available for rabies once symptoms develop and those that develop symptoms will die.
Children can be more likely than adults to be exposed to rabies. Natural curiosity and exploration may entice them to approach animals; fear of being chastised may make them conceal an exposure.
- It is important that children are aware of the need to avoid animal contact during travel and equally the importance of reporting any exposure that does occur.
Pre-travel rabies vaccination should be considered for children travelling to countries that are considered high risk for rabies. Please see the Rabies advice page for further information.
Children, especially young children may be more likely to be exposed to food and water borne illness during travel due to their natural exploratory nature and hand to mouth habits.
Risk can be reduced by frequent hand washing (or use of alcohol based hand cleansing gel when hand washing is not an option). Children should eat freshly cooked, hot food when possible and avoid raw food that cannot be peeled or cooked and unpasteurised dairy products.
Water for drinking, making up formula milk, diluting drinks and cleaning teeth should be bottled or boiled; see the Breastfeeding and Bottle-feeding advice page for further information.
Children and infants should be discouraged from drinking shower, bath or swimming pool water. Parents of toddlers may decide to take pre-packaged food with them.
Children suffering diarrhoeal illnesses can become dehydrated quickly, rehydration is a priority:
- clear fluids such as diluted fruit juices or oral rehydration solutions should be drunk liberally
- all rehydrating drinks must be prepared with safe water
- children with severe or blood/mucous stained diarrhoea, high fever or severe abdominal pain should receive medical attention immediately
Babies and children are particularly vulnerable to sunburn and over exposure to the sun can increase their risk of skin cancer later in life. Sunburn may also cause considerable pain and discomfort in the short term.
The safest way to protect children from sunburn is to use a combination of shade, clothing and sunscreen.
- use a sunscreen of at least SPF 15 which also has high UVA protection
- ensure sunscreens are applied generously to ALL sun exposed areas. Sunscreen should be applied 20 - 30 minutes before sun exposure
- remember that showering, swimming and sweating may remove sunscreen; ensure frequent application and consider water resistant sunscreens
- cover children up using clothing such as wide brimmed hat and long sleeved tops, closed weaved fabrics may offer better sun protection
- protect eyes from sun exposure, use sunglasses with a CE mark, UV400 label or that offer 100% UV protection
- seek shelter; avoid sun exposure between 11am and 3pm when sun is typically stronger
See the Sun Exposure advice page for further information.
Local health and safety regulations vary between countries and may not be at the same standard as parents are used to in the UK. Parents must be aware of this and make a judgement about the safety of their child using facilities abroad.
Equipment for young children such as high chairs, microwaves for heating food and changing stations may not be available at many destinations. Parents should be advised to thoroughly research the facilities available prior to travel.
Road rules vary country to country and age appropriate child seats may not be available at the destination. Parents should check this prior to travel and consider taking their own child car seats if necessary.
- See the Accident Prevention advice page for further information.
Many countries do not provide the same access to medical facilities and treatments as the UK. Some countries may have reciprocal health care agreements with UK, see individual country pages for details.
All child travellers should be included in travel insurance policies, medical emergencies including repatriation should be included in the policy.
- See the travel insurance advice page for further details.
Medical Assistance
Parents should be aware of what to do if their child becomes ill whilst abroad including how to access emergency medical treatment. Parents should try and identify health care facilities prior to departure.
The Foreign, Commonwealth and Development Office (FCDO) provides details of the nearest British Embassy or Consulate that may be able to help locate health care facilities at the destination. Neither the FCDO or Embassy will pay for medical care even in an emergency.
- The International Society of Travel Medicine has a Global Travel Clinic Locator available on their website.
- Addresses for local medical services might also be available from larger hotels and from tour company representatives.
back to top
- Disease Prevention Advice
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How to Travel With Medication Needed for a Sick Child
When traveling with medication for a sick child, be aware of these potentially complicating factors
- Travel Tips
- Medical Kits
- Who Shouldn't Fly
- Can Airlines Refuse?
Traveling with a sick child is often manageable with the right preparations. But if your child has or is suspected to have a serious contagious illness, like whooping cough or COVID-19, or poses a health risk to others, you will need to delay your trip until your child's condition is stabilized.
Many world destinations prohibit medications, like Adderall , that are commonly used by children in the United States. Certain medications, like insulin pens and epipens, usually need to be declared, since needles are prohibited on planes. Before you leave, research your destination carefully to ensure you are compliant.
This article explains what medicines you can and cannot take when traveling. It also provides a handful of tips for navigating airports and country-specific regulations.
Tips for Traveling With a Sick Child
Whether you are traveling by land, sea, or plane, the key to navigating travel with a sick child is getting (and staying) organized.
It's a good idea to keep all medications and supplies in a separate, clear "medical kit," so that they are easy to find and can be quickly retrieved when you need them.
The following tips and Transportation Security Administration (TSA) recommendations can help you organize your medical kit and prepare for your journey with a sick child.
Organizing Medications
Although medications can be packed in checked or carry-on luggage, it's best to bring them in your carry-on. That way, they will be available if you need them on the plane or in the airport.
While organizing your medical kit, consider including:
- Solid medications (such as pills or oral powders), which are permitted in carry-on or checked luggage in unlimited quantities, but will need to be Xd-rayed at the security checkpoint
- Extra medications in case your trip is extended or your medications get lost
TSA does not require passengers to bring medications in prescription bottles, so you can bring them in a pill organizer if you like. Laws vary between states and countries regarding prescription labeling, though. Check with the embassy at your destination to learn the respective laws.
Preparing Liquids and Other Types of Medications
Liquid medications are allowed in carry-on or checked bags, but you will need to follow a few regulations when flying with them:
- Medically necessary liquid medications can be brought in your carry-on or checked luggage in reasonable quantities. Tell an officer that you have a medically necessary liquid before starting the screening process. You may be asked to open the liquid medication for additional screening.
- Insulin is allowed in carry-on or checked luggage in reasonable quantities. At the security checkpoint, place insulin in a separate bin for X-ray screening.
- Nebulizers are allowed in carry-on bags but must be removed from the carrying case and X-rayed at the security checkpoint. Liquids associated with nebulizers are permitted in reasonable quantities.
As for injectables, inhalers, pumps, and aerosols:
- EpiPens can be packed in carry-on or checked luggage in reasonable quantities but must be declared to TSA officers at the security checkpoint for inspections.
- Insulin pumps are permitted in carry-on or checked luggage but must be accompanied by insulin. Tell TSA officers if you have diabetes and are wearing an insulin pump at the start of security screening.
- Medically necessary aerosols , such as metered-dose inhalers , are allowed in carry-on or checked bags in reasonable quantities but must be presented to TSA officers at the security checkpoint.
- Glucose monitors with metal or lithium batteries should be carried in carry-on luggage and should be presented to TSA officers at the security checkpoint.
- Inhalers are permitted in carry-on or checked luggage in reasonable quantities but will need to be X-rayed at the security checkpoint.
Federal regulations prohibit passengers from bringing their own supplemental oxygen onto airplanes. If you or your child require supplemental oxygen, you will need to call the airline at least 72 hours before your flight to arrange in-flight supplemental oxygen.
If you do not want a medical item to be X-rayed, you may request a visual inspection instead. Make this request before sending your items through the X-ray tunnel.
Not Sure if You Can Bring It?
Use the TSA "What Can I Bring?" website to find specific instructions related to most medications and medical supplies. This website provides instructions for external medical devices (such as feeding tubes), mercury thermometers, personal oxygen, syringes, and more.
Readying a "Back-Up" Plan
Plan where you will go for medical attention if needed. Write important numbers and addresses down and keep them in your medical kit.
Is there a children's hospital, pediatrician, or clinic where you are staying or on your travel route? This is especially important for international travelers and when you are on a cruise.
Even facilities that promote family travel and provide licensed healthcare providers for sick travelers are not guaranteed to have a pediatrician available in case of severe illness.
The nearest children's hospital or local medical society may be able to help you find a pediatrician if you are traveling and your child gets sick.
When traveling in another country, an international clinic , your travel agency, the U.S. Embassy, or the U.S. Consulate may be able to help you locate a pediatrician.
If your child has a chronic medical problem, consider acquiring a medical alert bracelet for them to wear, just in case they get sick and you aren't around. This is especially important if your child has severe allergies, diabetes, seizures, or another condition that may require sudden and specific medical care.
Informing Your Healthcare Provider
Before leaving, schedule a checkup with a pediatrician and/or pediatric specialist to ensure your child's medical problems are stable.
Be transparent about your plans with the healthcare provider—they may be able to offer you some travel tips that are specific to your child's condition.
Depending on your destination, certain vaccinations may be recommended for you and/or your child to protect from disease. The CDC provides detailed information about recommended vaccines for every country in the world.
If you are traveling internationally, take some time to review the country-specific recommendations, and make a list of any vaccines your child does not have. It may help to bring this list to your provider's office in case you have questions.
Contacting Your Pharmacist for Refills
If you lose a prescription while traveling internationally, contact your healthcare provider and explain your situation. Your provider may be able to write you a new prescription that you can bring to a pharmacy near you. You can also visit a local urgent care to see if they can help.
If you are traveling within the United States, you can:
- Find a nearby pharmacy that is in-network with your insurance provider.
- Call or visit the pharmacy and explain your situation.
- Call your home pharmacy and ask them to transfer your medication to your pharmacy of choice.
In the past, in order to have your prescription transferred, you would need to contact your healthcare provider and ask them to cancel the prescription then re-submit it to a new pharmacy. According to regulations updated in 2023, however, all you need to do is contact your home pharmacy directly and ask them to initiate the switch.
There is one important caveat to the updated regulations. Prescriptions may only be transferred between pharmacies once . So, if you want to transfer a prescription back to your original pharmacy after your trip, you will need to have it canceled and re-submitted by your healthcare provider.
Complying with Laws and Regulations
Different states and countries have different laws regarding the types and quantities of medications that travelers are permitted to bring.
For example, France permits travelers to only bring the amount of medication needed for the duration of the trip. And, if the medication is a narcotic , a written letter to customs providing the name and dosage of the medication is required.
Meanwhile, countries like Japan, Singapore, and much of Europe have banned Adderall, Ritalin, and a number of other medications that are common in the United States.
Bringing controlled drugs into a foreign country can come with steep consequences, from local fines, to jail time and deportation. In Singapore, having as little as three grams of morphine can result in the death penalty.
TSA advises international travelers to prepare "requisite medical documentation" from their prescribing physician at least two months before departure. The documentation should include:
- The prescribing physician's contact information and/or credentials
- The diagnosis and treatment
- The medication regimen, including any need for needles or syringes
Additionally, the name on the prescription, container, and traveler's passport must match.
If a medication contains narcotics, you may need to submit an application to the country's Narcotics Control Division or Food and Drug Administration for permission prior to entry.
For psychotropic medications , including antidepressants, you may need to notify the medical officer at the embassy in your home country. Do this well in advance so that all appropriate parties are aware before you arrive at customs.
What Else Should Go in a Medical Kit?
Your medical kit should contain everything you need to manage your child's health condition, as well as other medical items your child may only need on occasion.
Things to include in a travel medicine kit might include:
- A pain and fever reducer, such as ibuprofen and/or acetaminophen
- A steroid cream for itching
- An antihistamine for hives and other allergic reactions
- A cough and cold medicine for older children
- An antibiotic ointment (in a container of 3.4 ounces or less—unless medically necessary)
- A regular first aid kit
Keep in mind that if you are bringing an aerosol medication in your carry-on, it must be medically necessary. Aerosol insecticides, for example, are permitted in checked luggage only.
Is My Child Too Sick to Fly?
Do not fly if you or your child has a contagious disease that poses a serious threat to other people, such as:
- Tuberculosis
- Rubella (German measles)
- Whooping cough (pertussis)
- Meningococcal disease (meningitis)
- Severe flu or another respiratory illness
If you or your child has a history of the following conditions, see your healthcare provider for an evaluation before you travel to ensure the condition is stable:
- Cardiovascular disease
- Lung disease
- Mental illness
- Recent surgery
- Deep vein thrombosis or pulmonary embolism
- Sickle cell disease
Travel is rarely contraindicated (advised against) during a normal pregnancy. However, it's best to delay travel if your pregnancy requires close medical supervision. Reasons not to travel when pregnant include:
- You are in active or premature labor
- You have a suspected ectopic pregnancy
- You have vaginal bleeding
- You have a history of preeclampsia
Cabin air pressure changes can lead to barotrauma , recognizable by pain in the ear during take-off. Although barotrauma is rarely dangerous, it can lead to dizziness, hearing loss, or permanent tinnitus. To reduce these risks, consult with a healthcare provide before travel if your child has:
- An ear, nose, or sinus infection
- Severe congestion
- Had recent ear, nose, throat, or abdominal surgery
Will the Airline Refuse My Sick Child?
You or your child may be denied boarding if you have or are suspected to have a serious contagious illness that poses a public health threat.
Airline officials will suspect contagious illness if you or your child has one or more of the following symptoms:
- Difficulty breathing
- Persistent cough
- Decreased consciousness
- Sudden confusion
- Unexplained bruising or bleeding
- Persistent diarrhea
- Persistent vomiting
- Headache with stiff neck
- Appearing obviously unwell
- Symptoms of other contagious diseases
Less than 1% of passengers are denied boarding in the United States each year. Nonetheless, airline officials are permitted to deny boarding or remove any person from a flight who appears obviously sick, or who is believed to pose a health threat to others.
Inform the airport security screener if your child has any special needs for going through security, or if they might get upset during the security procedures because of their medical condition.
Before you travel with a sick child, give yourself plenty of time to organize a medical bag with daily medications, medical supplies, and any other extras your child may need. Most medications are permitted in carry-on or checked luggage. However, if you plan to fly with a medication that is liquid, aerosol, or involves needles, you will need to declare it to TSA officers at the security checkpoint.
Depending on your destination, you may need to prepare medical documentation, especially if you need to travel with a narcotic or psychotropic drug. There can be steep consequences for bringing controlled substances into another country, so don't take chances. If you have questions about traveling with your medications, contact a physician or use resources provided by TSA to learn more.
Centers for Disease Control and Prevention. Air travel .
Harvard Global Support Services. Tips for traveling with medication .
American Diabetes Association. What can I bring with me on the plane .
Transportation Security Administration. Can you pack your meds in a pill case and more questions answered .
Transportation Security Administration. What can I bring? .
Transportation Security Administration. Insulin .
United States Drug Enforcement Administration. Revised regulation allows DEA-registered pharmacies to transfer electronic prescriptions at a patient's request .
France in the United States. Information for private individuals - Medicine .
Transportation Security Administration. Traveling with medication .
Centers for Disease Control and Prevention. Protecting travelers' health from airport to community: Investigating contagious diseases on flights .
Centers for Disease Control and Prevention. Pregnant travelers .
Centers for Disease Control and Prevention. Preventing spread of disease on commercial aircraft: Guidance for cabin crew .
GAO. Airline consumer protections .
U.S. Department of Transportation. Bumping & oversales .
By Vincent Iannelli, MD Vincent Iannelli, MD, is a board-certified pediatrician and fellow of the American Academy of Pediatrics. Dr. Iannelli has cared for children for more than 20 years.

IMAGES
VIDEO
COMMENTS
View our range of travel sickness tablets & travel wrist bands. Shop today & collect Advantage Card points for every pound you spend. ... kids travel. festival. festival; visit festival. sunglasses. sunglasses; visit sunglasses. ... Boots.com is a trading name of Boots UK Limited. Registered office: Nottingham NG2 3AA.Registered in England ...
Motion sickness is caused by repeated movements when travelling, like going over bumps in a car or moving up and down in a boat, plane or train. The inner ear sends different signals to your brain from those your eyes are seeing. These confusing messages cause you to feel unwell. Find out more about motion sickness, an unpleasant combination of ...
Hyoscine hydrobromide (Kwells and Joy-Rides) Other brand names: Kwells Kids, Travel Calm, Scopoderm. Hyoscine hydrobromide (Kwells and Joy-Rides) Find out how hyoscine hydrobromide treats travel sickness and how to take it. NHS medicines information on hyoscine hydrobromide - what it's used for, side effects, dosage and who can take it.
Keep the car ventilated. Keep your car cool and well ventilated - open the windows if possible - and make sure your child is not too warm. 4. Eyes on the horizon. Although it can be tempting ...
Hyoscine is usually the most effective medicine for motion sickness. It is also known as scopolamine. It works by preventing the confusing nerve messages going to your brain. There are several brands of medicines which contain hyoscine - they also come in a soluble form for children.
Patches for travel sickness. The patches work like a plaster and you stick them on your skin. Stick a patch to the skin behind the ear, 5 to 6 hours before the start of your journey (or the evening before you travel). Remove the patch at the end of your journey. For long journeys, you can keep the patch on for up to 72 hours (3 days).
Hyoscine is the most effective medicine for travel sickness. It works by preventing the confusing messages going to your brain. ... For adults and children over 10 years of age: 150-300 micrograms. For those aged 4-10 years: 75-150 micrograms. ... Manufacturer's PIL, Joy-Rides® Tablets; Teva UK Limited, The electronic Medicines Compendium ...
Kwells Travel Sickness For Kids 12 Tablets. (6) £3.35. Add To Basket. Kwells medicines are indicated to prevent travel sickness. Kwells can be used by both kids (above 4 years) and adults. Kwells is used to prevent all types of Travel Sickness (car, coach, plane, train and ship) and is suitable for use in adults and children over the age of 4 ...
Preventing travel sickness in children aged four years and over. ... Children with a fever. (This medicine may reduce sweating). ... ©2024 Hearst UK is the trading name of the National Magazine ...
Some natural food flavourings can also settle your stomach and relieve symptoms: Ginger flavoured snacks or drinks - effective for all symptoms of motion sickness 5. Peppermint flavoured snacks or drinks - have a numbing and calming effect that helps ease nausea and headaches 6. 11. Try over-the-counter medicines.
Sea-legs tablets can help prevent travel sickness for up to 24 hours. A dose can be taken either an hour before travelling, or the evening before. Alternatively you can wait until feelings of ...
Travel Sickness (Motion Sickness) Motion sickness is feeling sick when you travel by car, boat, plane or train. There are things you can do to prevent it or relieve the symptoms. It is caused by repeated movements when travelling, like going over bumps in a car or moving up and down in a boat.
Hyoscine hydrobromide is a travel sickness (motion sickness) medicine that belongs to a group of medicines called anticholinergics or antimuscarinics. ... Do not use the patches on children under the age of 10 years. Do not drive a car or ride a bike if hyoscine hydrobromide makes you sleepy, gives you blurred vision, or makes you feel dizzy ...
Motion sickness is very common in children; particularly between 3 and 12 years old [6]. ... Therefore, it is advised that antimalarials are purchased in the UK before travel [20]. The first symptoms of malaria in children may be non-specific, for example fever, headache and muscle weakness. ... Committee to Advise on Tropical Medicine and ...
Travel sickness. Children often get motion sickness more than adults. Early symptoms of motion sickness include hot flushes, dribbling and paleness. What to pack - Several medicines are available to reduce or prevent symptoms of motion sickness. You can buy them from pharmacies or get them on prescription.
If you are going on a long trip, discuss this with your doctor, as you may need to make special arrangements for prescriptions and supplies of medicines. If your child has complex health needs and takes several medicines, talk to your healthcare professional before travelling. Information on individual medicines is available on the Medicines ...
Children over 10 years old Give the lower adult dose (one tablet). Children 5 - 10 years old Give half the lower adult dose (half a tablet). Children 2 - 5 years old Avomine Tablets are not suitable for children 2 - 5 years old. An oral liquid is recommended. Do not give to a child under 2 years old. Do not take Avomine for more than seven days ...
In this short blog, Dr Robert Walton looks at the evidence on treatments to prevent travel sickness (motion sickness). Take-home points. The new evidence on antihistamines comes from the Cochrane Review Antihistamines for motion sickness (published in October 2022) and is relevant to adults.. Travel sickness (motion sickness) is a common problem, and many people experience nausea for example ...
Hyoscine hydrobromide travel sickness tablets can be taken by most adults and children from the age of 3 years. Patches for travel sickness can be used by most adults and children from the age of 10 years. Who may not be able to take hyoscine hydrobromide. Hyoscine hydrobromide is not suitable for some people.
The safest way to protect children from sunburn is to use a combination of shade, clothing and sunscreen. use a sunscreen of at least SPF 15 which also has high UVA protection. ensure sunscreens are applied generously to ALL sun exposed areas. Sunscreen should be applied 20 - 30 minutes before sun exposure.
Medically necessary liquid medications can be brought in your carry-on or checked luggage in reasonable quantities. Tell an officer that you have a medically necessary liquid before starting the screening process. You may be asked to open the liquid medication for additional screening. Insulin is allowed in carry-on or checked luggage in ...
Scopolamine - the most commonly prescribed medication for motion sickness. It must be taken before symptoms start. It is available as a patch that is placed behind the ear 6-8 hours before ...