
TYLER S. ROGERS, MD, MBA, FAAFP, AND BRENDAN LUSHBOUGH, DO, Martin Army Community Hospital, Fort Benning, Georgia
Am Fam Physician. 2023;107(2):187-190
Author disclosure: No relevant financial relationships.

Key Clinical Issue
What are the risks and benefits of less frequent antenatal in-person visits vs. traditional visit schedules and televisits replacing some in-person antenatal appointments?
Evidence-Based Answer
Compared with traditional schedules of antenatal appointments, reducing the number of appointments showed no difference in gestational age at birth (mean difference = 0 days), likelihood of being small for gestational age (odds ratio [OR] = 1.08; 95% CI, 0.70 to 1.66), likelihood of a low Apgar score (mean difference = 0 at one and five minutes), likelihood of neonatal intensive care unit (NICU) admission (OR = 1.05; 95% CI, 0.74 to 1.50), maternal anxiety, likelihood of preterm birth (nonsignificant OR), and likelihood of low birth weight (OR = 1.02; 95% CI, 0.82 to 1.25). (Strength of Recommendation [SOR]: B, inconsistent or limited-quality patient-oriented evidence.) Studies comparing hybrid visits (i.e., televisits and in-person) with in-person visits only did not find differences in rates of preterm births (OR = 0.93; 95% CI, 0.84 to 1.03; P = .18) or rates of NICU admissions (OR = 1.02; 95% CI, 0.82 to 1.28). (SOR: B, inconsistent or limited-quality patient-oriented evidence.) There was insufficient evidence to assess other outcomes. 1
Practice Pointers
Antenatal care is a cornerstone of obstetric practice in the United States, and millions of patients receive counseling, screening, and medical care in these visits. 2 , 3 There is clear evidence supporting the benefits of antenatal care; however, the number of appointments needed and setting of visits is less understood.
The American College of Obstetricians and Gynecologists recommends antenatal visits every four weeks until 28 weeks' gestation, every two weeks until 36 weeks' gestation, and weekly thereafter, which typically involves 10 to 12 visits. 4
Expert consensus and past meta-analyses have favored fewer antenatal care visits given similar maternal and neonatal outcomes. In 1989, the U.S. Public Health Service suggested a reduction in the antenatal visit schedule based on a multidisciplinary panel and expert opinion in conjunction with a literature review; however, the American College of Obstetricians and Gynecologists has not updated its guidelines, and practices have not changed. 5 A 2010 Cochrane review found no differences in perinatal mortality between patients randomized to higher vs. reduced antenatal care groups in high-income countries, and a 2015 Cochrane review showed no difference in neonatal outcomes for women in high-income countries. 6 , 7
The Agency for Healthcare Research and Quality (AHRQ) review showed moderate- and low-strength evidence and did not find significant differences between traditional and abbreviated schedules when looking at many outcomes, such as gestational age at birth, low birth weight, Apgar scores, NICU admission, preterm birth, and maternal anxiety. The review was limited by a small evidence base with studies that are difficult to compare. The randomized controlled trials that were eligible were adjusted for confounding, whereas the nonrandomized controlled studies were not adjusted and were at high risk for confounding.
Telemedicine, defined as the use of electronic information and telecommunication to support health care among patients, clinicians, and administrators, is a new option for antenatal care delivery. 8 Televisits, the real-time communication between patients and clinicians via phone or the internet, are the specific interactions that encompass telemedicine. Recent literature suggests that supplementing in-person visits with televisits in low-risk pregnancies resulted in similar clinical outcomes and higher patient satisfaction scores. 9 The AHRQ review found no significant differences between rates of preterm births or NICU admissions for a hybrid model of televisits and in-person visits compared with in-person visits only. The review was limited due to the lack of adjustments for potential confounders in the study. For example, some of the studies were conducted during the COVID-19 pandemic, which adds multiple confounders and potential for bias.
The AHRQ review offers limited opportunity for conclusions to suggest changes in current practice. The current evidence supports past evidence, suggesting that fewer visits are not associated with neonatal or maternal harm, and televisits may have a role in antenatal care. Many of the other outcomes of interest had insufficient evidence to generate conclusions.
Editor's Note: American Family Physician SOR ratings are different from the AHRQ Strength of Evidence ratings.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army, the U.S. Department of Defense, or the U.S. government.
For the full review, go to https://effectivehealthcare.ahrq.gov/sites/default/files/product/pdf/cer-257-antenatal-care.pdf .
Balk EM, Konnyu KJ, Cao W, et al. Schedule of visits and televisits for routine antenatal care: a systematic review. Comparative effectiveness review no. 257. (Prepared by the Brown Evidence-Based Practice Center under contract no. 75Q80120D00001.) AHRQ publication no. 22-EHC031. Agency for Healthcare Research and Quality; June 2022. Accessed October 1, 2022. https://effectivehealthcare.ahrq.gov/sites/default/files/related_files/cer-257-antenatal-care-evidence-summary.pdf
Kirkham C, Harris S, Grzybowski S. Evidence-based prenatal care: part I. General prenatal care and counseling issues. Am Fam Physician. 2005;71(7):1307-1316.
Zolotor AJ, Carlough MC. Update on prenatal care. Am Fam Physician. 2014;89(3):199-208.
Kriebs JM. Guidelines for perinatal care, sixth edition: by the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. J Midwifery Womens Health. 2010;55(2):e37.
Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. 1991;77(5):782-787.
Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2010(10):CD000934.
Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015(7):CD000934.
Fatehi F, Samadbeik M, Kazemi A. What is digital health? Review of definitions. Stud Health Technol Inform. 2020;275:67-71.
Cantor AG, Jungbauer RM, Totten AM, et al. Telehealth strategies for the delivery of maternal health care: a rapid review. Ann Intern Med. 2022;175(9):1285-1297.
The Agency for Healthcare Research and Quality (AHRQ) conducts the Effective Health Care Program as part of its mission to produce evidence to improve health care and to make sure the evidence is understood and used. A key clinical question based on the AHRQ Effective Health Care Program systematic review of the literature is presented, followed by an evidence-based answer based on the review. AHRQ’s summary is accompanied by an interpretation by an AFP author that will help guide clinicians in making treatment decisions.
This series is coordinated by Joanna Drowos, DO, MPH, MBA, contributing editor. A collection of Implementing AHRQ Effective Health Care Reviews published in AFP is available at https://www.aafp.org/afp/ahrq .
Continue Reading

More in AFP
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
We use cookies. Read more about them in our Privacy Policy.
- Accept site cookies
- Reject site cookies
Search results:
- Afghanistan
- Africa (African Union)
- African Union
- American Samoa
- Antigua and Barbuda
- Bolivia (Plurinational State of)
- Bonaire, Sint Eustatius and Saba
- Bosnia and Herzegovina
- British Virgin Islands
- Brunei Darussalam
- Burkina Faso
- Cayman Islands
- Central Africa (African Union)
- Central African Republic
- Channel Islands
- China, Hong Kong Special Administrative Region
- China, Macao Special Administrative Region
- China, Taiwan Province of China
- Cook Islands
- Côte d'Ivoire
- Democratic People's Republic of Korea
- Democratic Republic of the Congo
- Dominican Republic
- Eastern Africa (African Union)
- El Salvador
- Equatorial Guinea
- Falkland Islands (Malvinas)
- Faroe Islands
- French Guiana
- French Polynesia
- Guinea-Bissau
- Humanitarian Action Countries
- Iran (Islamic Republic of)
- Isle of Man
- Kosovo (UNSCR 1244)
- Lao People's Democratic Republic
- Liechtenstein
- Marshall Islands
- Micronesia (Federated States of)
- Netherlands (Kingdom of the)
- New Caledonia
- New Zealand
- North Macedonia
- Northern Africa (African Union)
- Northern Mariana Islands
- OECD Fragile Contexts
- Papua New Guinea
- Philippines
- Puerto Rico
- Republic of Korea
- Republic of Moldova
- Russian Federation
- Saint Barthélemy
- Saint Helena, Ascension and Tristan da Cunha
- Saint Kitts and Nevis
- Saint Lucia
- Saint Martin (French part)
- Saint Pierre and Miquelon
- Saint Vincent and the Grenadines
- Sao Tome and Principe
- Saudi Arabia
- Sierra Leone
- Sint Maarten
- Solomon Islands
- South Africa
- South Sudan
- Southern Africa (African Union)
- State of Palestine
- Switzerland
- Syrian Arab Republic
- Timor-Leste
- Trinidad and Tobago
- Turkmenistan
- Turks and Caicos Islands
- United Arab Emirates
- United Kingdom
- United Republic of Tanzania
- United States
- Venezuela (Bolivarian Republic of)
- Virgin Islands U.S.
- Wallis and Futuna
- Western Africa (African Union)
Search countries
Search for data in 245 countries
- SDG Progress Data
- Child Marriage
- Immunization
- Benchmarking child-related SDGs
- Maternal and Newborn Health Disparities
- Continuity of essential health services
- Country profiles
- Interactive data visualizations
- Journal articles
- Publications
- Data Warehouse
- Antenatal care

- Current status
- Available data
- Recent resources
Notes on the data
Antenatal care is essential for protecting the health of women and their unborn children.
Through this form of preventive health care, women can learn from skilled health personnel about healthy behaviours during pregnancy, better understand warning signs during pregnancy and childbirth, and receive social, emotional and psychological support at this critical time in their lives. Through antenatal care, pregnant women can also access micronutrient supplementation, treatment for hypertension to prevent eclampsia, as well as immunization against tetanus. Antenatal care can also provide HIV testing and medications to prevent mother-to-child transmission of HIV. In areas where malaria is endemic, health personnel can provide pregnant women with medications and insecticide-treated mosquito nets to help prevent this debilitating and sometimes deadly disease.
Globally, while 88 per cent of pregnant women access antenatal care with a skilled health personnel at least once, only two in three (69 per cent) receive at least four antenatal care visits. In regions with the highest rates of maternal mortality, such as Western and Central Africa and South Asia, even fewer women received at least four antenatal care visits (56 per cent and 55 per cent, respectively). In viewing these data, it is important to remember that the percentages do not take into consideration the skill level of the healthcare provider or the quality of care, both of which can influence whether such care succeeds in bringing about improved maternal and newborn health.
Historical data show that the proportion of women receiving at least four antenatal care visits has increased globally over the last decade. The scale and pace of this progress, however, differs greatly by region. In Western and Central Africa, for example, only about half of pregnant women received four or more antenatal care visits between 2015 and 2021 (5 6 per cent). Stronger and faster progress is needed across all higher burden regions to drastically improve maternal and newborn outcomes.
Disparities in antenatal care coverage
Despite progress being made, large regional and global disparities in women receiving at least four antenatal care visits are observed by residence and wealth. Women living in urban areas are more likely to receive at least four antenatal care visits than those living in rural areas, with an urban-rural gap of 20 percentage points (79 per cent and 59 per cent, respectively). In addition, antenatal care coverage increases with wealth, with those in the richest quintile being almost twice as likely to receive at least four antenatal care visits than those in the poorest quintile, with a wealth gap of 29 percentage points (78 per cent and 49 per cent, respectively).
UNICEF, 2019, Health y Mothers, Healthy Babies: Taking stock of maternal health , New York 2019.
World Health Organization, 2016, WHO recommendations on antenatal care for a p ositive pregnancy ex p erience 2016.
UNICEF, The State of the World’s Children 2023 , UNICEF, New York, 2023.
WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division, Trends in Maternal Mortality: 2000 to 2020 , WHO, Geneva, 2023.
Antenatal care coverage
Maternal and newborn health coverage, build and download your own customisable dataset, women’s, children’s and adolescents’ health country profiles and dashboards.
Renewing progress on women’s, children’s and adolescents’ health in the era of COVID-19

Ending preventable newborn deaths and stillbirths by 2030

Measurement and accountability for maternal, newborn and child health: Fit for 2030?
Measurement of reproductive, maternal, newborn and child health and nutrition

Maternal and Newborn Health Disparities country profiles
Every Newborn Action Plan: Country implementation tracking tool guidance note
Pregnancy, Childbirth, Postpartum and Newborn Care: A guide for essential practice
Trends in Maternal Mortality: 1990 to 2015
Definition of indicators
Antenatal care coverage (at least one visit) is the percentage of women aged 15 to 49 with a live birth in a given time period that received antenatal care provided by skilled health personnel (doctor, nurse or midwife) at least once during pregnancy.
Skilled health personnel refers to workers/attendants that are accredited health professionals – such as a midwife, doctor or nurse – who have been educated and trained to proficiency in the skills needed to manage normal (uncomplicated) pregnancies, childbirth and the immediate postnatal period, and in the identification, management and referral of complications in women and newborns. Both trained and untrained traditional birth attendants are excluded.
Antenatal care coverage (at least four visits) is the percentage of women aged 15 to 49 with a live birth in a given time period that received antenatal care four or more times. Available survey data on this indicator usually do not specify the type of the provider; therefore, in general, receipt of care by any provider is measured.
Antenatal visits present opportunities for reaching pregnant women with interventions that may be vital to their health and well-being and that of their infants. WHO recommends a minimum of four antenatal visits based on a review of the effectiveness of different models of antenatal care. WHO guidelines are specific on the content of antenatal care visits, which should include:
- blood pressure measurement
- urine testing for bacteriuria and proteinuria
- blood testing to detect syphilis and severe anaemia
- weight/height measurement (optional).
Measurement limitations. Receiving antenatal care during pregnancy does not guarantee the receipt of interventions that are effective in improving maternal health. Receiving antenatal care at least four times, which is recommended by WHO, increases the likelihood of receiving effective maternal health interventions during antenatal visits. Importantly, although the indicator for ‘at least one visit’ refers to visits with skilled health providers (doctor, nurse or midwife), ‘four or more visits’ refers to visits with any provider, since standardized global national-level household survey programmes do not collect provider data for each visit. In addition, standardization of the definition of skilled health personnel is sometimes difficult because of differences in training of health personnel in different countries.
Related Topics
- Delivery care
- Maternal mortality
- Newborn care
Join our community
Receive the latest updates from the UNICEF Data team
- Don’t miss out on our latest data
- Get insights based on your interests
The dataset you are about to download is licensed under a Creative Commons Attribution 3.0 IGO license.
Antenatal Care
Percent distribution of antenatal care by type of provider, and percentage of antenatal care from a skilled provider.
1) Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by highest type of provider of antenatal care for most recent birth.
2) Percentage of women with a live birth or a stillbirth in the last 2 years receiving antenatal care from a skilled provider for the most recent birth.
Population base:
a) Women who have had a live birth in the 2 years preceding the survey (NR file)
b) Women who have had a stillbirth in the 2 years preceding the survey (NR file)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (NR file)
Time period: Two years preceding the survey
Numerators:
Number of women within the base population who:
1) were attended for antenatal care (ANC) for their last most recent live birth (m80 = 1) or stillbirth (m80 = 3), distributed according to the type of provider with the highest level of qualification (m2a – m2n = 1). (Note that types of providers and variables below are based on the standard DHS-8 questionnaire. Actual provider types and variables are survey specific but will be from the m2a–m2n series.) The types of providers are country specific but typically include:
a) Doctor (m2a = 1)
b) Nurse/midwife (m2b = 1)
c) Auxiliary midwife (m2c = 1)
d) Community health worker/fieldworker (m2i = 1)
e) Traditional birth attendant (m2g = 1)
f) Other (m2h = 1 or m2j = 1 or m2k = 1 or m2l = 1 or m2m = 1)
g) No ANC (m2n = 1)
2) Number of women receiving antenatal care from a skilled provider for the most recent most recent live birth (m80 = 1) or stillbirth (m80 = 3). The classification of skilled provider is also country specific, but typically includes providers such as Doctor, Nurse/midwife, and Auxiliary midwife (often m2a = 1 or m2b = 1 or m2c = 1, but depends on the survey)
Denominator: Number of women in each of the population bases:
a) Women who have had a live birth in the 2 years preceding the survey (m80 = 1 & p19 < 24)
b) Women who have had a stillbirth in the 2 years preceding the survey (m80 = 3 & p19 < 24)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (m80 = 1 or 3 & p19 < 24 )
Variables: NR file.
Calculation
During data collection respondents may mention more than one provider. The percent distribution by type of provider takes the highest type of provider from the list above and does not include other providers mentioned by the respondent.
For each type of provider, the numerator divided by the overall denominator, multiplied by 100.
Handling of Missing Values
"Don't know" or missing values on type of provider are excluded from numerators but included in denominators.
Notes and Considerations
Percent distribution adds up to 100 percent.
The category “Trained nurse/midwife” includes only medically trained and licensed personnel. Traditional birth attendants (also sometimes called midwives) are not considered skilled providers, whether trained or untrained.
The category “Traditional birth attendant/other” includes auxiliary health personnel and cases where the respondent did not know the level of qualification.
The category skilled provider typically includes doctor/nurse, midwife, and auxiliary midwife. The category ‘auxiliary midwife’ may or may not be considered skilled in providing ANC and should be adapted to reflect the country’s healthcare system as in most countries, not all cadres of health care professionals are considered “skilled” in providing ANC.
Footman, K., L. Benova, C. Goodman, D. Macleod, C. A. Lynch, L. Penn‐Kekana, and O. M. R. Campbell. 2015. "Using multi‐country household surveys to understand who provides reproductive and maternal health services in low‐and middle‐income countries: a critical appraisal of the Demographic and Health Surveys." Tropical Medicine & International Health , 20(5): 589-606.
Lawn, J. E., Blencowe, H., Waiswa, P. et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016. 387(10018), 587-603.
Wang, W., S. Alva, S. Wang, and A. Fort. 2011. Levels and trends in the use of maternal health services in developing countries. DHS Comparative Reports No. 26 . Calverton, Maryland, USA: ICF Macro. https://dhsprogram.com/publications/publication-cr26-comparative-reports.cfm
DHS-8 Tabulation plan: Table 9.1
API Indicator IDs:
RH_ANCP_W_DOC, RH_ANCP_W_NRS, RH_ANCP_W_AUX, RH_ANCP_W_CHW, RH_ANCP_W_OHW, RH_ANCP_W_TBA, RH_ANCP_W_OTH, RH_ANCP_W_MIS, RH_ANCP_W_NON, RH_ANCP_W_SKP
( API link , STATcompiler link )
MICS6 Indicator TM.5a: Antenatal care coverage: at least once by skilled health personnel.
Changes over Time
This indicator changed significantly in DHS-8. The reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Also, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey. Finally, the categories of providers changed slightly. “Auxiliary nurse/midwife” was changed to “Auxiliary midwife” and “Community health worker” was changed to “Community health worker/fieldworker”.
Percent distribution of number of antenatal care visits, and of timing of first antenatal visit
1) Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by number of antenatal care visits for most recent birth.
2) Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by number of months pregnant at time of first antenatal care visit for most recent birth.
1) Received antenatal care for their last most recent live birth (m80 = 1) and/or stillbirth (m80 = 3), according to grouped number of visits (m14)
2) Received antenatal care for their last most recent live birth (m80 = 1) and/or stillbirth (m80 = 3), according to grouped number of months they were pregnant at time of first visit (m13)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (m80 = 1 or 3 & p19 < 24)
Number of antenatal visits is grouped into categories of no antenatal visits, 1 visit, 2 visits, 3 visits, 4-7 visits, 8+ visits, and “don’t know” before calculating percentages. Timing of first antenatal visit is grouped into categories of no antenatal visit, <4 months, 4-6 months, 7+ months, and “don’t know” before calculating percentages. The percentages are the numerators divided by the denominator, multiplied by 100.
"Don't know" or missing values on number of antenatal care visits and timing of first ANC are excluded from numerators but included in denominators.
Percent distributions add up to 100 percent.
In DHS-8, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. The population base for this indicator was also expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey.
Also, in DHS-8, the groupings were changed to include 8+ ANC visits based on WHO recommendations.
Benova, L., Ö. Tunçalp, A.C. Moran and O.M.R. Campbell, 2018. “Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries.” BMJ Global Health , 3 (2), p.e000779. https://gh.bmj.com/content/3/2/e000779
MacQuarrie, K.L.D., L. Mallick, and C. Allen. 2017. Sexual and reproductive health in early and later adolescence: DHS data on youth Age 10-19 . DHS Comparative Reports No. 45. Rockville, Maryland, USA: ICF. https://dhsprogram.com/publications/publication-cr45-comparative-reports.cfm
Owolabi, O.O., K.L.M. Wong, M.L. Dennis, E. Radovich, F.L. Cavallaro, C.A. Lynch, A. Fatusi, I. Sombie, and L. Benova. 2017. "Comparing the Use and Content of Antenatal Care in Adolescent and Older First-Time Mothers in 13 Countries of West Africa: A Cross-Sectional Analysis of Demographic and Health Surveys." The Lancet Child & Adolescent Health 1(3):203-212. https://www.sciencedirect.com/science/article/pii/S2352464217300251
Wang, W., S. Alva, S. Wang, and A. Fort. 2011. Levels and trends in the use of maternal health services in developing countries . DHS Comparative Reports No. 26. Calverton, Maryland, USA: ICF Macro. https://dhsprogram.com/publications/publication-cr26-comparative-reports.cfm
World Health Organization. 2016. WHO recommendations on antenatal care for a positive pregnancy experience . Geneva: World Health Organization. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/
World Health Organization. 2018. Global reference list of 100 core health indicators . Geneva: World Health Organization. https://apps.who.int/iris/handle/10665/259951
DHS-8 Tabulation plan: Table 9.2
RH_ANCN_W_NON, RH_ANCN_W_N01, RH_ANCN_W_N23, RH_ANCN_W_N4P, RH_ANCN_W_DKM,
RH_ANCT_W_NON, RH_ANCT_W_TL4, RH_ANCT_W_T45, RH_ANCT_W_T67, RH_ANCT_W_T8P, RH_ANCT_W_DKM
WHO 100 Core Health Indicators: Antenatal care coverage
MICS6 Indicator TM.5b: Antenatal care coverage: at least four times by any provider.
MICS6 Indicator TM.5c: Antenatal care coverage: at least eight times by any provider
Median number of months pregnant at time of first antenatal care visit
Median number of months pregnant at the time of first antenatal care visit for the most recent birth (live birth or stillbirth) in the 2 years preceding the survey.
a) Women who have had alive birth in the 2 years preceding the survey (NR file)
Time period: Two years preceding the survey.
Number of women within each base population who received antenatal care for their most recent live birth (m80 = 1) or stillbirth (m80 = 3) according to the single number of months they were pregnant at time of first visit (m13)
a) Women who have had a live birth in the 2 years preceding the survey who received antenatal care for the live birth (m80 = 1 & m13 < 96 & p19 < 24)
b) Women who have had a stillbirth in the 2 years preceding the survey who received antenatal care for the stillbirth (m80 = 3 & m13 < 96 & p19 < 24)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who received antenatal care for their last birth (m80 = 1 or 3 & m13 < 96 & p19 < 24)
For the median, first calculate percentages of single months pregnant at first visit by dividing the numerators by the denominator. Cumulate the percentages by single months starting with the lowest value.
Linearly interpolate between the number of months immediately before and after where the cumulated distribution exceeds 50 percent to determine the median. See Median Calculations in Chapter 1 .
“Don’t know” and missing values excluded from numerators and denominator of percentages for median calculation.
In DHS-8, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Also, in DHS-8, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey.
DHS-8 Tabulation plan: Table 9.2
RH_ANCT_W_MED
Percentage of women receiving components of antenatal care
1) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had their blood pressure measured.
2) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had a urine sample taken.
3) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had a blood sample taken.
4) Among women with a live birth or a stillbirth in the last 2 years, the percentage that had the baby’s heartbeat listened for.
5) Among women with a live birth or a stillbirth in the last 2 years the percentage that were counseled about maternal diet.
6) Among women with a live birth or a stillbirth in the last 2 years the percentage that were counseled about breastfeeding.
7) Among women with a live birth or a stillbirth in the last 2 years, the percentage that were asked about vaginal bleeding.
b) Women who received antenatal care for their most recent live birth in the 2 years preceding the survey (NR file)
c) Women who have had a stillbirth in the 2 years preceding the survey (NR file)
d) Women who received antenatal care for their most recent stillbirth in the 2 years preceding the survey (NR file)
e) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (NR file)
f) Women who received antenatal care for their most recent birth (live birth or stillbirth) in the 2 years preceding the survey (NR file)
Number of women within each base population who:
1) had their blood pressure measured (m42c = 1)
2) had a urine sample taken (m42d = 1)
3) had a blood sample taken (m42e = 1)
4) had baby’s heartbeat listened for (m42f = 1)
5) were counseled about maternal diet (m42g = 1)
6) were counseled about breastfeeding (m42h = 1)
7) were asked about vaginal bleeding (m42i = 1)
Denominators: Number of women in each of the population bases:
b) Women who have had a live birth in the 2 years preceding the survey who received antenatal care for their last birth (m80 = 1 & m2n = 0 & p19 < 24)
c) Women who have had a stillbirth in the 2 years preceding the survey (m80 = 3 & p19 < 24)
d) Women who have had a stillbirth in the 2 years preceding the survey who received antenatal care for their stillbirth (m80 = 3 & m2n = 0 & p19 < 24)
e) Women who have had a live birth or a stillbirth in the 2 years preceding the survey (m80 = 1 or 3 & p19 < 24)
f) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who received antenatal care for their last birth (m80 = 1 or 3 & m2n = 0 & p19 < 24)
For percentages, the numerator divided by the denominator, multiplied by 100.
“Don’t know” and missing values on key components of antenatal care (e.g., urine sample taken) are excluded from numerators but included in denominators, assuming that they did not receive the antenatal care component.
In DHS-8, a number of changes were made to indicators on content of ANC. First, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Second, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey. Additionally, maternal report of receipt of these specific items of ANC are now reported among both number of women with a livebirth and/or stillbirth in the last 2 years AND number of women who attended ANC for their livebirth and/or stillbirth in the last 2 years.
Several additional key items for content of ANC were added as a proxy for quality of care. These included listening to the baby’s heartbeat and counseling on maternal diet and breastfeeding.
Indicators on iron-supplementation and deworming used to be included in the same table as these components but are now presented in a separate table.
DHS-8 Tabulation plan: Tables 9.3.1 and 9.3.2
RH_ANCC_W_IRN, RH_ANCC_W_PAR, RH_ANCS_W_BLP, RH_ANCS_W_URN, RH_ANCS_W_BLS
MICS6 Indicator TM.6: Content of antenatal care
Percentage of women receiving food/cash assistance, deworming, and iron-containing supplementation during pregnancy
1) Percentage of women with a live birth or a stillbirth in the last 2 years who received food or cash assistance during their most recent pregnancy.
2) Percentage of women with a live birth or a stillbirth in the last 2 years who took intestinal parasite drugs during their most recent pregnancy.
3) Percentage of women with a live birth or a stillbirth in the last 2 years who took iron tablets or syrup during their most recent pregnancy.
1) received food or cash assistance during the pregnancy of the most recent live birth or stillbirth (m82 = 1)
2) took iron tablets or syrup during the pregnancy for the most recent live birth or stillbirth (m45 = 1)
3) took intestinal parasite drugs during the pregnancy for the most recent live birth or stillbirth (m60 = 1)
“Don’t know” and missing values on indicators of food/cash assistance, deworming, and iron-containing supplementation are excluded from numerators but included in denominators, assuming that they did not receive the intervention.
In DHS-8, the reference time period for this indicator changed from 5 years to 2 years, reflecting a shorter time period asked about in the women’s questionnaire. Also in DHS-8, the population base for this indicator was expanded from only women who had at least one live birth in the 2 years preceding the survey to include women who had a stillbirth in the 2 years preceding the survey, as well as women who had one or more births (either live birth or stillbirth) in the 2 years preceding the survey.
The indicator on food/cash assistance was added in DHS-8. The indicators on iron-supplementation and deworming used to be included in the same table as the other ANC components but are now presented in a separate table.
Bhutta ZA, Das JK, Bahl R, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014;384(9940):347–70
DHS-8 Tabulation plan: Table 9.4
Percent distribution of number of days taking iron-containing supplements during pregnancy
Percentage of women with a live birth or a stillbirth in the last 2 years, distributed by number of days taking iron-containing supplements during their most recent pregnancy.
Number of women within each base population who by number of days she took iron-containing supplements during the most recent pregnancy (m46)
Number of days during which women took iron-containing supplements is grouped into categories of none, <60, 60-89, 90-179, 180+, and “don’t know” before calculating percentages. Percentages are the numerators divided by the denominator, multiplied by 100.
“Don’t know” values included in percent distributions. Missing values are excluded from numerators but included in denominators.
(API link TBD, STATcompiler link TBD)
Percentage of women who obtained iron-containing supplements, by source of supplements
Percentage of women with a live birth or a stillbirth in the last 2 years who obtained iron-containing supplements during their most recent pregnancy, by source of supplements.
a) Women who have had a live birth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent live birth (NR file)
b) Women who have had a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent stillbirth (NR file)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the most recent pregnancy (NR file)
Number of women within each base population who were given or bought iron-containing supplements during pregnancy, by declared source of iron-containing supplements (m45 = 1 & m81a – x)
a) Women who have had a live birth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent live birth (m80 = 1 & m45 =1 & p19 < 24)
b) Women who have had a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the pregnancy of the most recent stillbirth (m80 = 3 & m45 =1 & p19 < 24)
c) Women who have had a live birth or a stillbirth in the 2 years preceding the survey who were given or bought iron-containing supplements during the most recent pregnancy (m80 = 1 or 3 & m45 =1 & p19 < 24)
Numerators divided by the same denominator and multiplied by 100.
Supplements may have been obtained from more than one source.
DHS-8 Tabulation plan: Table 9.5
- Open access
- Published: 17 November 2021
Timing of first antenatal care visits and number of items of antenatal care contents received and associated factors in Ethiopia: multilevel mixed effects analysis
Zeitpunkt der ersten Besuche bei der Schwangerenvorsorge und Anzahl der erhaltenen Inhalte der Schwangerenvorsorge und damit verbundene Faktoren in Äthiopien: Mehrebenenanalyse mit gemischten Effekten
- Berhanu Teshome Woldeamanuel ORCID: orcid.org/0000-0002-1930-5432 1 &
- Tadesse Ayele Belachew 1
Reproductive Health volume 18 , Article number: 233 ( 2021 ) Cite this article
3162 Accesses
12 Citations
2 Altmetric
Metrics details
Receiving quality antenatal care (ANC) from skilled providers is essential to ensure the critical health circumstances of a pregnant woman and her child . Thus, this study attempted to assess which risk factors are significantly associated with the timing of antenatal care and the number of items of antenatal care content received from skilled providers in recent pregnancies among mothers in Ethiopia.
The data was extracted from the Ethiopian Demographic and Health Survey 2016. A total of 6645 mothers were included in the analysis. Multilevel mixed-effects logistic regression analysis and multilevel mixed Negative binomial models were fitted to find the factors associated with the timing and items of the content of ANC services. The 95% Confidence Interval of Odds Ratio/Incidence Rate Ratio, excluding one, was reported as significant.
About 20% of the mothers initiated ANC within the first trimester, and only 53% received at least four items of antenatal care content. Being rural residents (IRR = 0.82; 95%CI: 0.75–0.90), wanting no more children (IRR = 0.87; 95%CI: 0.79–0.96), and the husband being the sole decision maker of health care (IRR = 0.88; 95%CI: 0.81–0.96), were associated with reduced items of ANC content received. Further, birth order of six or more (IRR = 0.74; 95%CI: 0.56–0.96), rural residence (IRR = 0.0.41; 95%CI: 0.34–0.51), and wanting no more children (IRR = 0.61; 95%CI: 0.48–0.77) were associated with delayed antenatal care utilization.
Conclusions
Rural residences, the poorest household wealth status, no education level of mothers or partners, unexposed to mass media, unwanted pregnancy, mothers without decision-making power, and considerable distance to the nearest health facility have a significant impact on delaying the timing of ANC visits and reducing the number of items of ANC received in Ethiopia. Mothers should start an antenatal care visit early to ensure that a mother receives all of the necessary components of ANC treatment during her pregnancy.
Zusammenfassung
Hintergrund.
Eine qualitativ hochwertige Schwangerenvorsorge (ANC) durch qualifizierte Anbieter ist für die Sicherung der kritischen Gesundheitslage einer schwangeren Frau und ihres Kindes unerlässlich. In dieser Studie wurde daher untersucht, welche Risikofaktoren bei Müttern in Äthiopien in signifikantem Zusammenhang mit dem Zeitpunkt der Schwangerenvorsorge und der Anzahl der Inhalte der Schwangerenvorsorge stehen, die in den letzten Schwangerschaften von qualifizierten Anbietern durchgeführt wurden.
Die Daten wurden aus dem Ethiopian Demographic and Health Survey 2016 extrahiert. Insgesamt wurden 6645 Mütter in die Analyse einbezogen. Es wurden mehrstufige logistische Regressionsanalysen mit gemischten Effekten und mehrstufige gemischte negative Binomialmodelle verwendet, um die Faktoren zu ermitteln, die mit dem Zeitpunkt und den Inhalten der ANC-Leistungen in Verbindung stehen. Das 95%ige Konfidenzintervall der Odds Ratio/Inzidenzrate, mit Ausnahme von einem, wurde als signifikant angegeben.
Etwa 20% der Mütter begannen die ANC innerhalb des ersten Trimesters, und nur 53% erhielten mindestens vier Elemente der Schwangerenvorsorge. Die Tatsache, dass die Mütter auf dem Land wohnten (IRR = 0,82; 95%CI: 0,75–0,90), keine weiteren Kinder wollten (IRR = 0,87; 95%CI: 0,79–0,96) und der Ehemann der alleinige Entscheidungsträger für die Gesundheitsfürsorge war (IRR = 0,88; 95%CI: 0,81–0,96), war mit einer geringeren Anzahl an erhaltenen ANC-Inhalten verbunden. Außerdem waren die Reihenfolge der Geburten von sechs oder mehr (IRR = 0,74; 95%CI: 0,56–0,96), der Wohnsitz auf dem Land (IRR = 0,0,41; 95%CI: 0,34–0,51) und der Wunsch, keine weiteren Kinder zu bekommen (IRR = 0,61; 95%CI: 0,48–0,77) mit einer verzögerten Inanspruchnahme der Schwangerenvorsorge verbunden.
Schlussfolgerungen
Ländliche Wohnorte, der geringste Wohlstand des Haushalts, kein Bildungsniveau der Mütter oder Partner, keine Exposition gegenüber Massenmedien, ungewollte Schwangerschaft, Mütter ohne Entscheidungsbefugnis und eine große Entfernung zur nächsten Gesundheitseinrichtung haben in Äthiopien einen signifikanten Einfluss auf die Verzögerung von ANC-Besuchen und die Verringerung der Anzahl der erhaltenen ANC-Posten. Die Mütter sollten frühzeitig mit der Schwangerenvorsorge beginnen, um sicherzustellen, dass sie während ihrer Schwangerschaft alle notwendigen Bestandteile der ANC-Behandlung erhalten.
Plain language summary
The third Sustainable Development Goals prioritizes maternal mortality reduction, intending to lower the worldwide maternal mortality rate to 70 per 100,000 live births by 2030. Regular antenatal care from a skilled provider reduces maternal mortality by 20%. The overall quality of ANC service is determined collectively by the timing of ANC, and the contents of ANC received. Though there is an increase in ANC visits and the quality of services received, only 74% of women who gave birth in 2019 received antenatal care from a skilled provider, ranging from 85% in the urban to 70% in the rural. Thus, the quality and content of care might remain poor while the coverage of ANC visits is high. Therefore, it is necessary to analyze the levels and risk factors that affect the timing of ANC visits and contents to assess the quality of ANC services. This is the focus of the current study's research. In this study, nationally representative data from the 2016 Ethiopian Demographic and Health Survey was employed. Our study shows that rural residences, the poorest wealth quintile, no education level, unexposed to mass media, unwanted pregnancy, without decision-making power, and being far from the nearest health facility were found to be factors that hinder early initiation of ANC visits and reduce the number of items of ANC received. In conclusion, we ought to initiate an ANC visit early for a frequent antenatal care visit so that a mother will receive the necessary ANC components.
Peer Review reports
Introduction
Maternal mortality reduction and enhancements in women’s health care are priorities of the third Sustainable Development Goal (SDGs) aimed to reduce the global maternal mortality ratio (MMR) to 70 per 100,000 live births by 2030 [ 1 ]. Between 2000 and 2017, the global maternal mortality rate (MMR) was reduced by 38% [ 2 ]. In Ethiopia, despite a 71.8% decline in MMR between 1990 and 2015, 1 in 64 women are at risk of dying from maternal-related causes, which is a big gap compared with MMR of 199 per 100, 000 live births plan 2020 [ 3 ]. It shows that more effort is needed to achieve the SGDs after ten years. Regular antenatal care from a skilled provider reduces maternal mortality by 20% [ 4 , 5 ]. According to the 2019 Ethiopian mini Demographic and Health Survey, 74% of women who gave birth in the five years before the survey received antenatal care (ANC) from a skilled provider, ranging from 85% in urban areas to 70% in rural areas [ 6 ]. Further, Ethiopia’s DHS 2016 revealed 75% of pregnant women had their blood pressure measured, 73% had a blood sample taken, 66% had a urine sample taken, and 66% received nutritional counseling during their ANC visits [ 7 ].
The use of health facilities is significantly associated with ANC visits, and sufficient ANC involves both the use of services and the sufficiency of the content within the services [ 8 , 9 ]. The 2016 Ethiopia DHS reports that only 20% of women had their first ANC visits in the first trimester, which calls for more ANC attendance [ 7 ]. Furthermore, concerning the type of skilled provider, doctors (5.7%), nurses/midwives (42%), health officers (1.4%), and health extension workers (13.2%) received ANC service.
Previous studies regarding antenatal care in Ethiopia and elsewhere recognized that women’s autonomy [ 10 , 11 , 12 ], birth order and the number of children born [ 13 , 14 , 15 ], husband’s attitude and support [ 10 , 16 ], lack of money [ 17 ] were the main reasons for lower health care utilization. Some studies reported that the education level of mother or husband/partner [ 10 , 11 , 12 , 13 , 15 , 17 , 18 , 19 , 20 ], age [ 10 , 11 , 14 , 19 ], woman’s occupation [ 10 , 17 ], place of residence [ 11 , 12 , 13 , 14 , 15 , 17 , 20 ], place of receiving [ 15 , 19 ], access to mass media [ 10 , 11 , 12 , 13 , 15 , 17 , 18 ], wealth quintile [ 10 , 11 , 12 , 13 , 14 , 15 , 17 , 18 , 19 ], and ANC provider [ 15 ] were the most important factors that affected the utilization of antenatal care services. According to the literature, wanted pregnancy [ 12 , 15 , 17 , 19 , 20 ], a lack of health care services such as a long distance to the health facility [ 10 , 17 , 19 ], health insurance [ 10 ], and permission to visit a health facility [ 17 ] were significant factors associated with antenatal care utilization and service quality.
The World Health Organization (WHO) recommends the first visit received before 12 weeks of pregnancy and the necessary contents of ANC visits to improve women’s care experience and reduce perinatal mortality [ 21 ]. Even though there is an increase in ANC visits and the quality of services received, many women are still not timely initiating the first ANC visit in Ethiopia. As a result, they have not received the critical contents of ANC. Though several studies in the past year in Ethiopia have explicitly examined associated factors of antenatal care utilization and completion of four or more visits during pregnancy [ 11 , 14 , 16 , 17 , 18 , 19 ], these studies did not investigate the actual number of components of ANC service a woman has received. Besides, these studies revealed that the contents of ANC visit highly influence the effectiveness of the ANC service. Thus, the quality and content of care might remain poor while the coverage of ANC visits is high. The overall quality of ANC service is determined collectively by the timing of ANC, and the contents of ANC received. Therefore, it is necessary to analyze the levels and risk factors that affect the timing of ANC visits and contents to assess the quality of ANC services. This is the focus of the current study's research.
Study setting, data and population
We used population based, nationally representative data from 2016 Ethiopian Demographic and Health Survey (DHS) [ 7 ]. The survey was conducted by the Central Statistical Agency (CSA) in collaboration with the Federal Ministry of Health (FMOH) and the Ethiopian Public Health Institute with technical assistance from ICF International and financial support from USAID, the government of the Netherlands, the World Bank, Irish Aid, and UNFPA from January 18, 2016, to June 27, 2016. The 2007 Ethiopia Population and Housing Census sampling frame with 84,915 enumeration areas (EAs), each EAs covering 181 households, was used. The respondents were selected using a stratified two-stage cluster design, each region stratified into urban and rural areas.
First was selecting 645 clusters (202 urban areas and 443 rural areas) with probability proportional to enumeration area size and independent selection within each stratum. In all the selected EAs, the household listing was done from September to December 2015. At the second stage, 28 households were selected per cluster with an equal probability systematic selection involving eligible women aged 15–49 years. Thus, a sample of 16,650 households and 15,683 women aged 15–49 years was identified with a response rate of 94.6%. Furthermore, details of the survey design and methodology have been reported in the 2016 EDHS [ 7 ].
Our analysis was based on the records of 6645 (54.3%) women who have complete information on the number of ANC visits, the timing of their first ANC visits, the contents of their ANC visits, and who gave birth in the five years preceding the survey. The latest deliveries were referred to all women.
This study has two response variables: Timing of first ANC visits; binary outcome categorized into 1 if a mother starts her first ANC visits within the first trimester (early initiation, or 12 weeks after the onset of pregnancy) and 0 elsewhere. Second, the contents of ANC received during pregnancy (a discrete outcome measured as the number of items WHO recommended and recognized as the contents of ANC) in Ethiopia received by a mother during pregnancy.
Standard guidelines for ANC in Ethiopia recognize that every pregnant woman should receive ANC from a skilled provider that consists of iron supplements, intestinal parasite drugs, at least two doses of Tetanus Toxoid injections, malaria intermittent preventive treatment in pregnancy, and health education on danger signs and complications during pregnancy; blood pressure measurement; urine tests; blood tests; health education on prevention of mother-to-child transmission of HIV/AIDS and HIV/AIDS counseling, testing, and collection of results. The composite index comprises a simple count of items received from skilled providers during the ANC visits. The variable had a minimum value of zero, indicating that the mother had not taken any items or received ANC. A maximum value of ten indicates that she has received all the nationally recommended and recognized content of the ANC. The important explanatory variables explored from previously available literature [ 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 ] are presented in Table 1 .
The wealth index was coded as: 1 = poorest, 2 = poorer, 3 = middle, 4 = richer, and 5 = richest. The wealth quintile of women’s households in EDHS is a composite indicator that scores were derived using principal component analysis based on housing characteristics and ownership of household durable goods [ 7 ]. National wealth quintiles are compiled by assigning the household score to each usual (de jure) household member, ranking each person in the household population by their score, and dividing the distribution into five equal categories, each comprising 20% of the population.
In EDHS 2016, birth order is a discrete variable ranging from 1 to 20. The proportion of birth orders two versus three and four versus five is nearly equal, so birth orders two and three and four and five were merged for this analysis. Further, the proportion of children with higher birth orders is relatively small, and birth orders of six and higher have been merged since the percentage distribution. The same categories were also used in the earlier study by Muchie [ 14 ]. Similarly, the percentage of women working in professional, technical, managerial, clerical, or unskilled manuals after screening for missing variables is too small, and the authors merge these two categories for this analysis. These too-few frequencies may, in turn, affect the parameter estimation.
Statistical methods of data analysis
Data analysis was done using the “R programming” version 4.0.3. Descriptive statistics of the subjects were summarized using frequency tables. A Chi-square test was performed to observe any association between the timing of the first ANC visit and the independent variables. An F-test based on analysis of variance (ANOVA) was used to examine the mean difference in the numbers of components of ANC received. Furthermore, the multilevel mixed-effects logistic regression was fitted to identify variables associated with the timing of first ANC visits. Meanwhile, multilevel mixed-effects count models were performed to identify factors associated with the number of ANC components received from a skilled provider during pregnancy.
First, a Poisson regression model with a log link was performed [ 22 ]. Then fitted Poisson regression checked for the problem of overdispersion (variance can be larger than the mean) or under dispersion (variance can be smaller than the mean) using the likelihood test. It was found that this test was significant. Therefore, the negative binomial (NB) regression model was considered the immediate solution for data analysis [ 23 ]. Moreover, the data experiencing excess zeros and overdispersion might be due to these excess zeros. Thus, we performed both the zero-inflated models (Zero Inflated Poisson and Zero Inflated Negative Binomial (ZINB)) and the Hurdle models (Hurdle Poisson (HP) and Hurdle Negative Binomial (HNB)) to check if overdispersion is accounted for due to excess zeros [ 24 ].
To account for the correlation between measurements (intra-cluster correlation (ICC)), we used the multilevel mixed-effects models (cluster/region-specific random effects). The use of a multilevel modeling approach accounts for the hierarchical nature of the EDHS data, where households were selected within EA clusters. There could be unobserved characteristics of cluster influencing women’s decision to timely initiate ANC and the number of ANC visits, such as the availability and accessibility of health services, cultural norms, and prevailing health beliefs. The outcomes of households within the same cluster are likely to correlate. Ignoring this correlation can underestimate variability (producing biased standard errors) and present falsely narrow confidence intervals [ 25 , 26 , 27 ].
Further, disregarding the hierarchical structure of the data and analyzing it as single-level data leads to incorrect inferences (i.e., high type I errors or loss of power) [ 28 ]. Finally, based on the Vuong statistic [ 29 ], likelihood ratio test, the Deviance, AIC, and BIC for model comparison, the multilevel mixed-effects negative binomial model best-fit factors associated with the number of items of ANC received from a skilled provider (see Additional file 1 ). Variables with a 95% confidence interval for the incidence risk ratio (IRR) excluding one were considered statistically significant determinants.
Socioeconomic and demographic characteristics of respondents
This study included 6645 women who had given birth within the five years preceding the survey. The background characteristics of women with respect to the timing of ANC visits are given in Table 2 . Most women (70.3%) were from rural areas, while only 29.7% were from urban areas. Concerning regions, a slightly higher percentage were from Tigray (14.6%), SNNPR (13.3%), Oromia (11.2%), and Amhara (10.7%), while the smallest percent of women were from Afar (6.1%), Gambela (6.8%), and Harari (6.8%). The median age was 27 years. Around 32% were from the richest, and 23% were from the poorest wealth quintile. The majority (49.5%) of women had no education, 32.8% had primary education, and only 6.6% had a higher education level. Regarding media access, only 2.8%, 16.3%, and 21.2% have read a newspaper or magazine, listened to the radio, and watched television at least once a week during their recent pregnancy.
On the other hand, concerning decision-making power over women’s health care, about two-thirds (65%) reported that both women and husbands/partners usually decide on respondents’ health care. Further, about 26% said they had a big problem getting permission to seek medical care, 50.1% had a big problem getting money for treatment in seeking medical care, and 44.2% had a far distance to a health facility in seeking medical care. In comparison, 33.7% reported a big problem in not wanting to go alone to seek medical care. In addition, the majority (80%) of women reported that their last child was wanted at the time of pregnancy. In comparison, 14.7% said the pregnancy was wanted later, and 5.3% reported they wanted no more.
Timing of first ANC visit by some characteristics of women
Only 20.1% of women started their ANC visit within the first trimester, with a median of four months for the first ANC visit. The proportion starting first ANC within the first trimester was lower in the SNNPR (22.2%), Benishangul-gumuz (23.1%), and Somali regions (32.1%), whereas it was higher in Dire Dawa (68.6%) and Addis Ababa (62.5%) cities. More than half (56.2%) of women from urban areas started their first ANC visit within the first trimester compared to 31.1% of rural women. Women who had higher levels of education (63.6%) and primary education (40%) started first ANC within the first trimester compared to uneducated women (31%). Further, women whose husbands/partners had higher education had the highest proportion (57%) of their first ANC visit within the first trimester.
The time to early initiate the first ANC visit was almost uniform among women’s age and occupation. The majority of women who read newspapers or magazines at least once a week (52%), who listen to the radio at least once a week (46%), and who watch television at least once a week (58%) started their ANC visits for their recent pregnancy within the first trimester. On the other hand, the proportion of women who began their first ANC visit within the first trimester increases with women’s autonomy concerning decisions about health care. Most women whose pregnancy was wanted (40%) started their first ANC visit within the first trimester and wanted no more children (25%). Moreover, 43% of women who had no problem getting money, 42.3% of women with a short distance to the nearest health facility, and 41% who had no difficulty going alone in seeking medical care had started their first ANC visit within the first trimester.
The number of items of ANC content received by some characteristics of mothers
Of all women who received ANC at least once, 79.9% had their blood pressure measured, 73.8% had a urine sample taken, and 79.5% had a blood sample taken. Further, 46.3% had been told about pregnancy complications, 45.4% received iron supplementation for at least 180 days, and 5.8% of women received treatment for an intestinal parasite. Additionally, 69.1% received counseling after testing AIDS, 53.7% were informed about birth preparedness, 67% received nutritional counseling, and 42.5% received two or more doses of tetanus toxoid vaccine from a skilled provider during their ANC visits (Fig. 1 ). The mean number of ANC contents received by a woman was 3.5 items and a standard deviation of 2.2, indicating that the distribution is overdispersed. Figure 2 presents a further detailed examination of the relationship between the frequency of ANC visits and the number of items of ANC contents received. It revealed that the likelihood of receiving the highest number of items of ANC content increases with the frequency of ANC visits. The proportion of women who received six items has monotonically increased from 4.2 to 37.3%, increasing ANC visits from one visit to at least five ANC visits (Fig. 2 ).
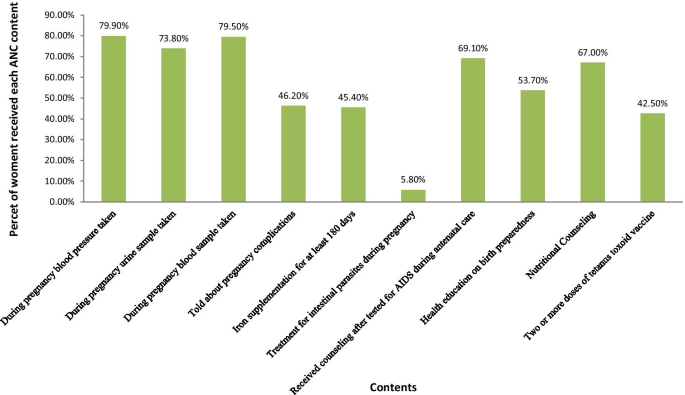
Types of items of ANC Contents received during pregnancy in Ethiopia, EDHS 2016, n = 6645
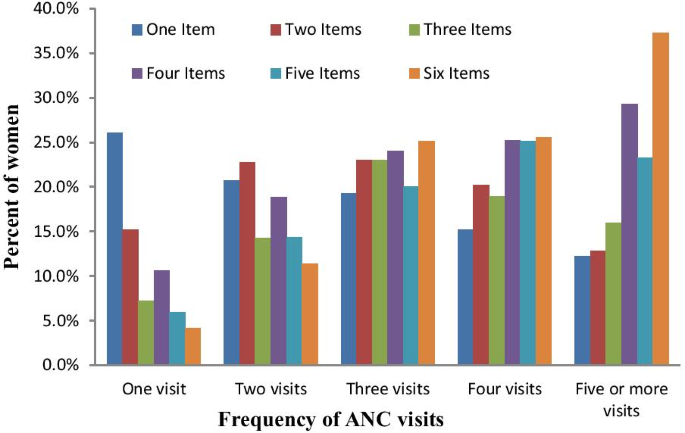
Percentage distribution of number of items of ANC contents received by frequency of ANC visits in Ethiopia, EDHS 2016
Conversely, the pattern showed a declining trend of the likelihood of receiving only one item or two items, or three items, with an increase in the number of ANC visits. In addition, the timing of the first ANC visit showed a positive association with the mean number of items of ANC contents received. For instance, a woman who started her first ANC visit within the first trimester received, on average, 6.2 items. In comparison, women who had received only one ANC visit had received an average of 3.8 items, compared to virtually six items on average among women with four or more ANC visits (Table 3 ).
Factors associated with the timing of the first ANC visits: multilevel mixed-effects logistic regression analysis
The multivariable multilevel logistic regression analysis of factors associated with the timing of the first ANC visit is given in Table 4 . The likelihood of timely initiating the first ANC visit was lower among six or more birth orders (AOR = 0.74; 95%CI: 0.56–0.96) than the first birth order. Moreover, rural women were 59% less likely to start their first ANC visit within the first trimester (AOR = 0.41; 95%CI: 0.31–0.54) than urban counterparts.
The log odds of timely initiating the first ANC visit were higher among the richest wealth quintile (AOR = 2.17; 95%CI: 1.61–2.92), the 4 th (AOR = 2.29; 95%CI: 1.87–2.81), and the 3 rd (AOR = 2.02; 95%CI: 1.68–2.42) wealth quintile, respectively, as compared to the poorest wealth quintile. The odds of starting the first ANC visit within the first trimester was 5.2 times (AOR = 5.20; 95%CI: 2.25–12.03), 2.14 times (AOR = 2.14; 95%CI: 1.50–3.06) and 1.73 times (AOR = 1.73; 95%CI: 148–2.02), higher among women with a higher, secondary and primary level of education, respectively, as compared to uneducated women after controlling for other variables in the model. Similarly, women whose husbands had higher education levels were 45% (AOR = 1.45; 95%CI: 1.08–1.95) more likely to start their ANC within the first trimester than those whose husbands had not been educated. Women aged 40–44 years old were 34% (AOR = 0.66; 95%CI: 0.44–0.99) less likely to start their first ANC visit on time than women aged 15–19 years old.
Furthermore, women who listened to the radio less than once a week (AOR = 1.56; 95%CI: 1.25–1.93), at least once a week (AOR = 1.49; 95%CI: 1.20–1.85) and watched television at least once a week (AOR = 1.58; 95%CI: 1.11–2.23), respectively, were more likely than those who did not listen to the radio or watch television to start their first ANC in the first trimester. Pregnant women who want no more children were 39% (AOR = 0.61; 95%CI: 0.48–0.77) less likely to start their first ANC visit within the first trimester than those whose pregnancies were wanted. Furthermore, a woman who reported a short distance to a health facility seeking medical care was 55% (AOR = 1.55; 95%CI: 1.35–1.78) more likely to start her first ANC visit within the first trimester (Table 4 ).
Factors associated with the number of ANC content items received by a woman: Multilevel mixed-effects Negative binomial analysis
The estimated incidence rate ratio (IRR) indicates that women from rural areas (IRR = 0.82; 95%CI: 0.75–0.90) and female heads (IRR = 0.91; 95%CI: 0.85–0.97) were significantly associated with lower numbers of items of ANC content received. Further, women who wanted no more children (IRR = 0.87; 95%CI: 0.79–0.96), whose husbands/partners decided alone, were significantly associated with lower numbers of items of ANC content received. In contrast, women from the richest wealth quintile (IRR = 1.51; 95%CI: 1.36–1.67), 4 th wealth quintile (IRR = 1.62; 95%CI: 1.49–1.75) and 3 rd wealth quintile (IRR = 1.47; 95%CI: 1.37–1.59), women who had primary education (IRR = 1.24; 95%CI: 1.17–1.32), secondary education (IRR: 1.22, CI: 1.10–1.34) and higher education (IRR = 1.21; 95%CI: 1.05–1.39) as well as women whose partners had primary education (IRR = 1.17; 95%CI: 1.01–1.24), secondary education (IRR = 1.21; 95%CI: 1.11–1.34) and higher education (IRR = 1.16; 95%CI: 1.04–1.30) were more likely to receive a higher number of items of ANC contents. Additionally, women who have no problem of getting permission (IRR = 1.10; 95%CI: 1.03–1.17), who reported short distance to health facilities (IRR = 1.19; 95%CI: 1.12–1.26), who listen to the radio less than once a week (IRR = 1.12; 95%CI: 1.04–1.19) and at least once a week (IRR = 1.15; 95%CI: 1.07–1.23), who watch television less than once a week (IRR = 1.09; 95%CI: 1.01–1.19), who had received 1–3 ANC (IRR = 5.12; 95%CI: 4.68–5.59) and at least four ANC (IRR = 6.08; 95%CI: 5.56–6.65) from a skilled provider were significantly more likely to have a higher number of items of ANC contents during their pregnancy.
The study found that 53% of women received at least four ANC items, while 20% started their first ANC visit within the first trimester. The multilevel negative binomial regression analysis revealed that the covariates of rural residents and an unwanted child at the time of pregnancy were significantly associated with the lower incidence rate ratio of the number of ANC contents received. Further, the frequency of ANC visits during pregnancy was significantly associated with a higher incidence rate ratio of ANC contents received. In contrast, female heads were significantly associated with a lower incidence rate ratio of ANC contents received. The multilevel logistic regression analysis revealed that having six or more birth orders, living in a rural area, being between the ages of 40 and 44, and wanting no more children were all significantly associated with a lower likelihood of initiating ANC visits on time. Higher wealth quintile, higher education level of women and partners, access to mass media, and a short distance to the health facility in seeking medical care, on the other hand, were significantly associated with increased odds of initiating an ANC visit for a recent pregnancy within the last five years before the survey.
This study showed that higher birth order was inversely associated with the timing of the ANC visit, i.e., women were less likely to start their ANC visit within the first trimester of their sixth or higher birth order. A similar study in Uganda [ 30 ] found mothers with third birth orders, compared to those with the first, are about 6–7% less likely to attain the four antenatal visits, and mothers with at least the third birth order are 4–5% less likely to initiate the first visit in the first trimester. Muchie [ 14 ], using Ethiopian Mini DHS 2014, also found 38 and 36% lower odds of completing four or more visits of ANC utilization for birth orders of children four or five, and six or more, respectively. One possible reason for this might be mainly in the first pregnancy when women wanted lots of contact with their care provider. Some women would have liked more communication between appointments and were worried about having to deal with pregnancy complications and pain.
Rural mothers are less likely to receive higher ANC content from skilled providers and start ANC visits within the first trimester than urban mothers. This finding is congruent with that of Beeckman et al. [ 10 ], who reported higher odds of delaying first ANC visits and ANC visits of less than four among rural mothers. Further, a study done in Bangladesh, [ 12 ] found rural mothers are 17% less likely to attend a higher number of ANC visits than urban mothers. Another similar finding from Bangladesh [ 8 ] reported that urban mothers were 1.35 times more likely to receive more items of ANC services from a skilled provider than their rural counterparts. In Ethiopia’s rural areas, there is a lack of skilled health care providers, lack of information on antenatal care services, lack of infrastructure, and long distances from health facilities.
Moreover, most mothers in rural Ethiopia were uneducated. Contrary to our findings, Gebremeskel et al. [ 31 ] and Weldearegawi et al. [ 32 ] reported residence was not associated with the timing of the first ANC visit. This inconsistency might be due to the statistical methodology used and the smaller sample size used by Gebremeskel et al. [ 31 ] (n = 409) and Weldearegawi et al. [ 32 ] ( n = 402), whereas the EDHS 2016 used (n = 6645).
Furthermore, we found that women with at least primary education levels are more likely to start the first ANC visit within the first trimester and receive the highest number of items of ANC content from skilled providers. Similarly, women whose partners had at least a primary education were more likely to receive higher ANC content from skilled providers than the uneducated category. Additionally, women whose partners had higher education were more likely to start ANC visits within the first trimester than those without. Further analysis of the 2011 Ethiopian DHS showed that women who had primary education (79%), secondary education (62%), and higher education were 45% times less likely to delay their first ANC visit [ 10 ]. Consistent with our finding, Islam [ 8 ] also found that there is a 1.12, 1.26, and 1.39 incidence rate ratio of receiving higher numbers of ANC content among women having primary, secondary, and higher education in Bangladesh. But, partners’ primary education level has not significantly increased the incidence of receiving the items of ANC content. In contrast, partners having a secondary or higher education significantly increased the incidence of receiving the items of ANC content [ 8 ].
In contrast, in Ghana, Manyeh et al. [ 33 ] found no significant effect of husband/partner education level on the timing of ANC visits. Additionally, a systematic review analysis in sub-Saharan Arica found that husband education was significantly associated with uptake, frequency, and timing of first ANC visits [ 10 ]. Most likely, this could be because educated women have more access to information and make their own decisions on their health care, which empowered them to exercise, and changed traditional attitudes about using the ANC service. This study suggests that there is an urgent need to focus on mothers’ education. Advocating primary education for girls and encouraging them to pursue secondary or higher education is essential to achieve a tangible change to achieve the sustainable development goals of maternal and infant mortality reduction through effective implementation of maternal health care services [ 14 , 34 ].
The result also suggests women who listened to the radio and watched television at least once a week were more likely to start their first ANC early and received more items of ANC content from skilled providers. This result agrees with the findings of Yaya et al. [ 11 ], where women who watch television at least once a week were 40% less likely to delay their first ANC visit than those who do not watch television at all. But they did not find an association between listening to the radio and the timing of the first antenatal care visit. This variation might be due to a difference in the methodology used. In Bangladesh [ 8 , 12 ], mass media access was associated with increased ANC content received.
Women whose pregnancies were unwanted or wanted later were more likely to delay their first ANC visit and less likely to receive the highest number of ANC content items than wanted pregnancies. A similar study of the Bangladeshi DHS found that wanted pregnancy was associated with a higher incidence of receiving higher items of ANC contents [ 8 ]. Another study from Bangladesh [ 12 ], Southern Ethiopia [ 31 ], Bahir Dar [ 35 ], and Eastern Tigray [ 32 ] found unwanted pregnancy significantly associated with delayed initiation of ANC service utilization. This might be that mothers with unwanted pregnancies have anxiety and poor psychological well-being [ 36 ] and less attention to pregnancy-related complications, and do not use supplements such as folic acid, vaccinations, health information, and nutritional counseling [ 37 ]. Thus, women ought to be encouraged to use modern contraceptives to prevent unwanted pregnancies.
Furthermore, women’s health decision-making power is significantly associated with the content of ANC services received. Women without decision-making power or whose husband/partner alone decides on their health care are strongly associated with lower ANC contents received. This result was congruent with those of northwest Ethiopia [ 38 ], Bangladesh [ 12 ], the systematic review of sub-Saharan Africa [ 10 ], and Tanzania [ 39 ]. However, unlike our findings, Gebresilassie et al. [ 40 ] found that decision-making on self-care seeking was not significantly associated with the timing of the first ANC visit.
Mothers with a shorter distance to the nearest health facility had better odds of initiating their first ANC visit and receiving items of ANC content from skilled providers. Similar findings are reported in a study in Bahir Dar, Ethiopia [ 35 ]. In the Eastern Tigray zone in Northern Ethiopia, distance to the nearest health facility was not a significant predictor of late antenatal care follow-up [ 32 ] . In Rwanda, distance to the health facility was not a significant predictor of poor quality of antenatal utilization [ 41 ]. Likewise, mothers who had permission to seek medical care were more likely to receive more ANC content.
Lastly, the results indicated that the frequency of ANC visits and timing of the first ANC visit during pregnancy was positively associated with the number of items of ANC contents a woman received from a skilled provider. Women who started antenatal care within the first trimester were more likely to receive more ANC contents items than those who delayed their visit. Likewise, the number of items of ANC content monotonically increases with frequent ANC visits. The findings are consistent with those of [ 42 , 43 ].
Findings of this study suggest that rural residences, the poorest wealth quintile, no education level of mothers or partners, unexposed to mass media, unwanted pregnancy, mothers without decision-making power, and a long distance to the nearest health facility have significant impacts on delaying the timing of ANC visits and reducing the number of items of ANC received in Ethiopia. Further, timely initiation of the ANC and the number of ANC visits were significantly associated with the increase in the number of items ANC received during pregnancy. Therefore, this study recommends that women initiate ANC visits timely and frequent antenatal care visits during pregnancy for the quality of ANC received from a skilled provider. Another implication of this study is that educating and empowering girls, particularly in the rural areas, are vital ingredients in all policies aiming to reduce maternal and neonatal deaths through improved quality of antenatal care utilization, particularly in the rural areas. Furthermore, encouraging women to use modern contraceptives, expanding health education in the media, and expanding health facilities are vital inputs that should be included in policies to improve the quality of antennal care utilization, particularly in rural areas. Moreover, women at low economic levels should be given special emphasis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Antenatal care
Confidence interval
Central Statistics Agency
Demographic and Health Survey
Ethiopia Demographic and Health Survey
Enumeration areas
Federal Ministry of Health
Hurdle Poisson
Hurdle negative binomial
Incidence rate ratio
Likelihood ratio test
Maternal Mortality Ratio
Negative Binomial
Sustainable Development Goals
United Nations Population Fund
United States Agency for International Development
World Health Organization
Zero Inflated Poisson
Zero Inflated Negative Binomial
United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. New York: United Nations; 2015. https://sustainabledevelopment.un.org/.pdf
WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division. Trends in maternal mortality: 2000 to 2017. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division; World Health Organization. Geneva: WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division; 2019. https://www.unfpa.org/featured-publication/trends-maternal-mortality-2000-2017 .
Ministry of Health (MOH), Health Sector Transformation plan, 2015/16–2019/20. Addis Ababa, Ethiopia: MOH; 2015 https://www.worldcat.org/title/hstp-health-sector-transformation-plan-201516-201920-2008-2012-efy .
Testa J, OueÂdraogo C, Prual A, et al. Determinants of risk factors associated with severe maternal morbidity: application during antenatal consultations. J GyneÂcol Obste t Biol Reprod (Paris). 2002;31:44–50.
CAS Google Scholar
Prual A, et al. The quality of risk factor screening during antenatal consultations in Niger. Health Policy Planning. 2000;15(1):11–6.
Article CAS Google Scholar
Central Statistical Agency. Ethiopia Mini Demographic and Health survey 2019. Addis Ababa, Ethiopia: Central Statistics Agency; 2019. https://www.unicef.org/ethiopia/Mini/Demographic/and/Health/Survey.pdf
Central Statistics Agency (CSA) [Ethiopia] and ICF International. Ethiopia demographic and health survey 2016. Addis Ababa and Rockville: Central Statistical Agency (CSA) and ICF International; 2016. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf .
Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: assessing the extent of compliance with the WHO recommendations. PLoS ONE. 2018;13(9):e0204752.
Article Google Scholar
Beeckman K, et al. The development and application of a new tool to assess the adequacy of the content and timing of antenatal care. BMC Health Serv Res. 2011;11(1):213.
Okedo-Alex IN, Akamike IC, Ezeanosike OB, et al. Determinants of antenatal care utilization in sub-Saharan Africa: a systematic review. BMJ Open. 2019;9(10):e031890.
Yaya S, et al. Timing and adequate attendance of antenatal care visits among women in Ethiopia. PLoS ONE. 2017;12(9):e0184934.
Bhowmik KR, Das S, Islam MA. Modelling the number of antenatal care visits in Bangladesh to determine the risk factors for reduced antenatal care attendance. PLoS ONE. 2020;15(1):e0228215.
Adhikari M, et al. Sociodemographic correlates of antenatal care visits in Nepal: results from Nepal Demographic and Health Survey 2016. BMC Pregn Childbirth. 2020;20:513.
Kindie Fentahun Muchie. Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: a finding based on a demographic and health survey. BMC Pregn Childbirth. 2017;17:300.
Birmeta K, Dibaba Y, Woldeyohannes D. Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC Health Serv Res. 2013;13:256.
Mekonnen T, et al. Trends and determinants of antenatal care service use in Ethiopia between 2000 and 2016. Int J Environ Res Public Health. 2019;16:748.
Tsegaye B, Ayalew M. Prevalence and factors associated with antenatal care utilization in Ethiopia: an evidence from demographic health survey 2016. BMC Pregn Childbirth. 2020;20:528.
Tegegne TK, et al. Antenatal care use in Ethiopia: a spatial and multilevel analysis. Pregn Childbirth. 2019;19:399.
Tiruaynet K, Muchie KF. Determinants of utilization of antenatal care services in Benishangul Gumuz Region, Western Ethiopia: a study based on demographic and health survey. BMC Pregn Childbirth. 2019;19:115.
Ochako R, Gichuhi W. Pregnancy wantedness, frequency and timing of antenatal care visit among women of childbearing age in Kenya. Reprod Health. 2016;13:51.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: WHO; 2016. http://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf .
McCullagh P, Nelder JA. Generalized Linear Models. 2nd ed. London: Chapman and Hall; 1986.
Google Scholar
Cameron AC, Trivedi PK. Essentials of count data regression. A companion to theoretical econometrics. 2001; 331.
Cameron AC, Trivedi PK. Regression analysis of count data. 2nd edition, Econometric Society Monograph. No. 53. Cambridge: Cambridge University Press; 2013.
Book Google Scholar
Goldstein H. Multilevel statistical models. London: Edward Arnold; 1995.
Domnner A, Klar N. Design and analysis of cluster randomization trials in health research. London: Arnold; 2000.
Klar N. A practical guide to cluster randomized trials in health services research. J Biopharm Stat. 2013;23:711–3.
Austin PC, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. 2017;36(20):3257–77.
Voung QH. Likelihood ratio test for model selection and non-nested hypothesis. Econometrica. 1989;57(2):307–33.
Bbaale E. Factors influencing timing and frequency of antenatal care in Uganda. Australian Medical Journal. 2011;4(8):431–8.
Gebrehiwot GW, et al. Determinants of late antenatal care follow up among pregnant women in Easter zone Tigray, Northern Ethiopia, 2018: unmatched case–control study. BMC Res Notes. 2019;12:752.
Gebremeskel F, Dibaba Y, Admassu B. Timing of first antenatal care attendance and associated factors among pregnant women in Arba Minch Town and Arba Minch District, Gamo Gofa Zone, South Ethiopia. J Environ Public Health. 2015;2015:971506.
Manyeh AK, et al. Factors associated with the timing of antenatal clinic attendance among firsttime mothers in rural Southern Ghana. BMC Pregn Childbirth. 2020;20:47.
Warri D, George A. Perceptions of pregnant women of reasons for late initiation of antenatal care: a qualitative interview study. BMC Pregn Childbirth. 2020;20:70.
Alemu Y, Aragaw A. Early initiations of first antenatal care visit and associated factor among mothers who gave birth in the last six months preceding birth in Bahir Dar Zuria Woreda North West Ethiopia. Reprod Health. 2018;15:203.
Gupta S, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS ONE. 2014;9(7):e101893.
Stern J, et al. Is pregnancy planning associated with background characteristics and pregnancy planning behavior? Acta Obstet Gynecol Scand. 2016;95(2):182–9.
Gudayu TW, Woldeyohannes SM, Abdo AA. Timing and factors associated with first antenatal care booking among pregnant mothers in Gondar Town; North West Ethiopia. BMC Pregn Childbirth. 2014;14:287.
Abdon GR, et al. Trends and factors associated with the utilisation of antenatal care services during the Millennium Development Goals era in Tanzania. Trop Med Health. 2020;48:38.
Gebresilassie B, et al. Timing of first antenatal care attendance and associated factors among pregnant women in public health institutions of Axum town, Tigray, Ethiopia, 2017: a mixed design study. BMC Pregn Childbirth. 2019;19:340.
Rurangirwa AA, et al. Determinants of poor utilization of antenatal care services among recently delivered women in Rwanda; a population based study. BMC Pregn Childbirth. 2017;17:142.
Mihret MS, Limenih MA, Gudayu TW. The role of timely initiation of antenatal care on protective dose tetanus toxoid immunization: the case of northern Ethiopia post natal mothers. BMC Pregn Childbirth. 2018;18:235.
Agha S, Tappis H. The timing of antenatal care initiation and the content of care in Sindh Pakistan. BMC Pregn Childbirth. 2016;16:190.
Download references
Acknowledgements
We are grateful to ICF macro (Calverton, USA) for providing the 2016 DHS data of Ethiopia.
Declaration
The authors declare that the research is our original work, and all sources of materials used have been duly acknowledged.
The author has no support or funding to report.
Author information
Authors and affiliations.
Salale University, Fitche, Oromiya, Ethiopia
Berhanu Teshome Woldeamanuel & Tadesse Ayele Belachew
You can also search for this author in PubMed Google Scholar
Contributions
TAB involved from the inception to design, acquisition of data, analysis and interpretation, drafting the manuscript, BT involved from the inception to design, acquisition of data, analysis and interpretation and drafting the manuscript and editing the manuscript for the final submission. Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Berhanu Teshome Woldeamanuel .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for this study was not required since the data is secondary and is available in the public domain. Anyone can download datasets after registering as a DHS data user at https://dhsprogram.com/data/new-user-registration.cfm .
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table s1..
AIC, BIC, Log-likelihood and Deviance based Model comparison for mixed effects models. Table S2. Vuong Tests for the non-nested models Poisson, negative-binomial (NB), zero-inflated Poisson (ZIP), hurdle Poisson (HP), zeroinflated NB (ZINB), and hurdle NB (HNB) models. Table S3. Akaike’s information criteria (AIC), log-likelihood, and likelihood-ratio for Poisson, negative-binomial regression (NB), mixed Poison (MP) and Mixed NBR (MNBR) models.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Woldeamanuel, B.T., Belachew, T.A. Timing of first antenatal care visits and number of items of antenatal care contents received and associated factors in Ethiopia: multilevel mixed effects analysis. Reprod Health 18 , 233 (2021). https://doi.org/10.1186/s12978-021-01275-9
Download citation
Received : 02 July 2021
Accepted : 25 October 2021
Published : 17 November 2021
DOI : https://doi.org/10.1186/s12978-021-01275-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Contents of antenatal care
- Timing of antenatal care
Schlüsselwörter
- Schwangerenvorsorge
- Inhalte der Schwangerenvorsorge
- Zeitplan der Schwangerenvorsorge
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
Loading metrics
Open Access
Peer-reviewed
Research Article
Number of antenatal care visits and associated factors among reproductive age women in Sub-Saharan Africa using recent demographic and health survey data from 2008–2019: A multilevel negative binomial regression model
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Epidemiology, Gambella Regional Health Bureau, Gambella, Ethiopia
Affiliation Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Affiliation Department of Human Nutrition, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
* E-mail: [email protected]
Affiliation Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- Fetene Getnet Gebeyehu,
- Bisrat Misganaw Geremew,
- Aysheshim Kassahun Belew,
- Melkamu Aderajew Zemene

- Published: December 27, 2022
- https://doi.org/10.1371/journal.pgph.0001180
- Peer Review
- Reader Comments
Antenatal care is one of the best strategies for maternal and neonatal mortality reduction. There is a paucity of evidence on the mean number of ANC visits and associated factors in Sub-Saharan Africa (SSA). This study aimed to investigate the mean number of ANC visits and associated factors among reproductive-age women in Sub-Saharan Africa using the Demographic and Health Survey conducted from 2008 to 2019.
A total of 256,425 weighted numbers of women who gave birth five years before the survey were included. We used STATA version 14 for data management and analysis. A multilevel negative binomial regression model was fitted. Finally, the Adjusted Incident Rate Ratio (AIRR) with its 95% CI confidence interval was reported. Statistical significance was declared at P-value < 0.05.
The mean number of ANC visits among women who gave birth five years before the survey in SSA was 3.83 (95% CI = 3.82, 3.84) Individual-level factors such as being aged 36–49 years (AIRR = 1.20, 95% CI = 1.18,1.21), having secondary education &above (AIRR = 1.44, 95% CI = 1.42, 1.45), having rich wealth status (AIRR = 1.08, 95% CI = 1.07, 1.09), media exposure (AIRR = 1.10, 95% CI = 1.09,1.11), and grand multiparity (AIRR = 0.90, 95% CI = 0.89, 0.91) were significantly associated with the number of ANC visits. Furthermore, rural residence (AIRR = 0.90, 95% CI = 0.89, 0.91), Western SSA region (AIRR = 1.19, 95% CI = 1.18, 1.20) and being from a middle-income country (AIRR = 1.09, 95% CI = 1.08, 1.10) were community-level factors that had a significant association with the number of ANC visits.
The mean number of ANC visits in SSA approximates the minimum recommended number of ANC visits by the World Health Organization. Women’s educational status, women’s age, media exposure, parity, planned pregnancy, wealth status, residence, country’s income, and region of SSA had a significant association with the frequency of ANC visits. This study suggests that addressing geographical disparities and socio-economic inequalities will help to alleviate the reduced utilization of ANC services.
Citation: Gebeyehu FG, Geremew BM, Belew AK, Zemene MA (2022) Number of antenatal care visits and associated factors among reproductive age women in Sub-Saharan Africa using recent demographic and health survey data from 2008–2019: A multilevel negative binomial regression model. PLOS Glob Public Health 2(12): e0001180. https://doi.org/10.1371/journal.pgph.0001180
Editor: Jitendra Kumar Singh, Janaki Medical College, Tribhuvan University, NEPAL
Received: May 27, 2022; Accepted: November 27, 2022; Published: December 27, 2022
Copyright: © 2022 Gebeyehu et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The dataset is available from the DHS program official database www.measuredhs.com .
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Antenatal care (ANC) is care provided by skilled healthcare professionals to pregnant women to ensure the best health conditions for both the mother and fetus during pregnancy [ 1 ]. ANC decreases maternal and perinatal morbidity and mortality [ 2 ]. The ANC service includes birth preparedness, advice on danger signs of pregnancy, counseling on optimal nutrition, prevention, identification and treatment of obstetric complications, and advice on options for family planning [ 3 ].
Maternal death is defined as the death of a woman while pregnant or within 42 days of the pregnancy’s termination from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes [ 4 ]. Child and maternal mortality continued to be major public health concerns in developing countries. Yearly, 527,000 women in low-income countries die from pregnancy-related complications, and nearly 4 million neonates die in their first of which 98% are from developing countries [ 5 ].
According to the World Health Organization (WHO) sustainable development goal (SDG) 3, countries should reduce child mortality to less than 25 deaths per 1,000 live births and maternal mortality to less than 70 per 100,000 live births by the year 2030 [ 6 ]. Although 121 countries had met the target on under-5 mortality, progress will need to accelerate in 53 countries, two-thirds of which are in sub-Saharan Africa [ 7 ]. Studies showed that utilization of at least one antenatal care visit by a skilled provider during pregnancy decreases the risk of neonatal mortality by 39% in sub-Saharan African countries. Thus, to accelerate progress toward the reduction of neonatal mortality, all pregnant women should receive antenatal care [ 8 ].
Globally, 87% of pregnant women received antenatal care visits at least once, and only 60% received the minimum required number of antenatal care visits [ 3 ]. In Sub-Saharan Africa, 49–53% of women received the minimum recommended number of ANC visits 35% accessed at least one visit and 13% of women had no antenatal care visits [ 9 ].
Due to the high burden of maternal and child mortality, WHO adopted the focused antenatal care model by the year 2002, which recommends a minimum of four antenatal care visits by a pregnant woman [ 10 ]. By the year 2016, at the start of the Sustainable Development Goal era, maternal and child mortality was unacceptably high and the world health organization changed the focused ANC model to an essential core package of routine ANC and the number of visits increased to eight [ 1 ].
Previous studies affirmed that Place of residence [ 11 , 12 ], wealth status [ 13 , 14 ], educational status [ 15 , 16 ], distance from a health facility [ 17 , 18 ], quality of health service [ 19 , 20 ], and cost of service [ 21 ] were factors associated with the number of antenatal care visit. Barriers to quality maternal health care must be recognized and addressed at all levels of the health system to enhance maternal health [ 22 ].
Though there are studies on the prevalence of ANC and associated factors in different African countries, we found limited evidence on the mean number of ANC visits and associated factors in SSA using the count model. Since most of the studies were conducted using binary logistic regression, information was lost while categorizing women’s different numbers of visits in the same group. Most of the studies focused on factors associated with the timing of the first ANC initiation. There is a paucity of information on the average number of ANC visits and associated factors among women in SSA.
The count model has the added benefit of estimating the mean number of ANC visits and associated factors, and information loss may not be an issue. Therefore, this study aimed to investigate the mean number of antenatal care visits and associated factors among reproductive-age women in SSA based on the 2008 to 2019 Demographic and Health Survey data.
Methods and materials
Study design, area, and period.
Secondary data analysis was conducted based on the recent Demographic and Health Survey (DHS) data of 35 Sub-Saharan African countries from 2008 to 2019. According to the United Nations geo scheme classification, the continent of Africa is commonly divided into five regions [ 23 ]. Sub-Saharan Africa contains four of these regions namely Eastern Africa, Central Africa, Western Africa, and Southern Africa. This study was conducted in these regions using their recent DHS datasets.
Source and study population
The source population was all reproductive-age women who gave birth five years before each respective survey in Sub-Saharan Africa, whereas those in the selected Enumeration Areas (EAs) were the study population. The sample size was determined from the kids to recode file “KR file” from the standard DHS dataset of Sub-Saharan African countries with at least one survey from 2008 to 2019. DHS uses a two-stage stratified cluster sampling technique. In the first stage, a sample of EAs was selected independently from each stratum with proportional allocation stratified by residence (urban & rural). In the second stage, from the selected EAs, households were taken by systematic sampling technique [ 24 ]. The final sample size was 257,924 (weighted sample 256, 425) women.
Variables and data collection procedure
The outcome variable was the number of antenatal care visits. The independent variables for this study were from two sources such as individual and community-level factors. The individual-level factors include; socio-economic and demographic-related factors, pregnancy-related factors, and behavioral-related factors. Community-level factors include; community-level media exposure, community-level women’s education, place of residence, sub-regions within SSA, and year of the survey. The data were accessed and downloaded from the webpage of the international Demographic and Health Survey.
Operational definitions
The number of antenatal care visits..
Non-negative integer for which this study aims to identify a proper count regression model.
Media exposure.
It was obtained by aggregating women’s exposure to television, radio, and newspaper and if women had been exposed at least once a week it was coded as “1” for yes, and if a woman had not been exposed at least once a week it was coded as “0” for no.
Wealth status.
Is a composite measure of a household’s cumulative living standard divided into 5 quantiles using the wealth quantile data derived from principal component analysis. Finally, it was coded as "0" for the poor, "1" for the middle, and "2" for the rich.

Community-level media exposure.
Was obtained by aggregating the individual level media exposure at the cluster level by using the proportion of women who had media exposure and it was coded as “0” for low (communities in which < 50% of women had media exposure), “1” for high community-level media exposure. This community-level media exposure shows the overall media exposure in the community.
Community-women education.
It was obtained by aggregating the individual-level women’s education into clusters by using the proportion of women who had attended at least primary education. It was coded as “0” for low (communities in which < 50% of women had at least primary education), and “1” for high community-Community-level.
Year of the survey.
The period when the survey was conducted.
Data analysis
The data was cleaned, coded, and extracted using MS excel and STATA version 14 software. Variables with missed values greater than 5% / not applicable were dropped. During data cleaning and coding, the same STATA command was applied for each country. After coding and cleaning the dataset for each country independently, all country dataset was appended to one dataset for further analysis. Sample weighting was done for each country before appending it to one dataset.
Poisson regression model
The standard Poisson regression model was the first model considered while working with count data. It is a technique used to describe count data as a function of a set of independent variables and which assumes the observations should be independent over time and the mean and the variance of the dependent variable should be equal [ 25 ].
However, the assumption of the Poisson regression failed (the sample variance exceeds the sample mean), in the case of overdispersion. In such a case the negative binomial regression model that includes an unobserved specific effect (random term or error term) for the parameter was the preferred one to handle the overdispersion. A Likelihood Ratio(LR) test for the parameter α (p-value < 0.001) was used for the over-dispersion parameter, in the negative binomial (NB) specification against the Poisson model specification [ 26 ].
Multilevel model building
Since DHS data has hierarchical nature different measures of variation (intra-class correlation coefficient (ICC), and Median Incident Rate Ratio (MIRR)) were calculated to detect any clustering effect. Finally, four multilevel count models were fitted.
First, a ‘‘ null ” model ( model 1 ), which only includes a random intercept and allows us to detect the existence of a possible contextual dimension for a phenomenon was estimated and provided evidence to assess random effect using the Intraclass Correlation Coefficient (ICC). Then the individual characteristics were included in the model ( model 2 ) to investigate the extent to which the overall difference in the number of ANC visits was explained by the individual variation. Next, community-level variables were added to the model ( model 3 ) to investigate whether this contextual phenomenon was conditioned by community-level characteristics. Finally, both individual and community-level characteristics were added to the model ( model 4 ) at the same time as the number of ANC visits.
Parameter estimation method
The fixed effects (a measure of association) were used to estimate the association between explanatory variables and the number of ANC visits at both individual and community levels. Factors with a p-value ≤ 0.25 were selected as candidates for the final model. The crude Incident Rate Ratio (CIRR) and the Adjusted Incident Rate Ratio (AIRR) were assessed and finally Adjusted Rate Ratio (AIRR) was presented. Associations between dependent and independent variables were assessed and their strength was presented using adjusted rate ratios and 95% confidence intervals with a p-value of <0.05.
The variance inflation factor (VIF) was assessed to check for multi-linearity and the mean VIF for the fitted model was 1.86. Finally, a model comparison was done using the deviance test, and the model with the lowest deviance was selected as the best-fit model.
Ethical consideration
The waiver of written informed consent was approved by the University of Gondar Institutional Review Board (IRB). As well, after online requesting and explaining the objective of this study to DHS Program/ICF International Inc., a letter of permission was waived from the International Review Board of Demographic and Health Surveys (DHS) program data archivists to download the dataset for this study. The data was not shared or passed on to other researchers.
Socio-demographic characteristics of respondents
A total of 257,924 reproductive-age women who gave birth within five years before the survey were included. The median age of women was 28 years with Inter Quartile Range (IQR) of 23–34 years. Nearly three fourth (72.3%) of the study participants were between the age of 20–35 years. More than one-third (38.43%)of the participants had no formal education. Nearly half (45.71%) of the respondents were from poor and poorest households, and about two-thirds (66.85%) were from rural areas. More than three fourth (77%) of the respondents were from the eastern and western regions of sub-Saharan Africa. And approximately one-third (28%) of the pregnancies were unwanted ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0001180.t001
Number of ANC visits during pregnancy
The mean number of ANC visits in SSA was 3.83 (95% CI = 3.82, 3.84) with the minimum average number of visits among Chadian women (2.29, 95% CI = 2.26, 2.34) and maximum average number of visits among Ghanan women (6.44, 95% CI = 6.35, 6.53). There was also a difference in the mean numbers of ANC visit among regions of SSA with 3.55 (95% CI = 3.53, 3.58) for women from the Central region, 3.66 (95% CI = 3.65, 3.67) for women from the Eastern region, 4.02 (95% CI = 4.00, 4.04) for women from Western region and 4.99 (95% CI = 4.93, 5.06) for women from Southern region.
Multilevel negative binomial regression analysis
Random effect and model comparison results.
Although we considered fitting different count models, we preferred the negative binomial regression model to the standard Poisson regression model as the sample variance (6.6) exceeds the sample mean (3.83) and the Likelihood Ratio (LR) test became significant (p-value <0.001). The data were also checked for excess zeros to determine if there was a possibility to choose models that are suitable for data with an inflated number of zeros (ZIP, ZINB, HP, and HNB). Different measures of variations were calculated to determine whether there is a clustering effect or not. First, the intra-class correlation was calculated and it affirmed that the total variability in the number of ANC visits explained by the cluster variation was only 1.1% ( Table 2 ). This indicated that the cluster variation was not large to use a multilevel model instead of the standard negative binomial regression model, but it is not always true [ 28 ].
https://doi.org/10.1371/journal.pgph.0001180.t002
Furthermore, we could use a likelihood ratio test to compare the likely hood of the fitted multilevel model with the standard model [ 29 ]. The p-value associated with the chi-squared statistics was less than 0.001, hence we would reject the null hypothesis of no between-cluster variation in the rate of occurrence of the outcome (number of ANC visits). In addition, the median incident rate ratio (MIRR) allows us to determine the median relative change in the rate of occurrence of the outcome (number of ANC visits) between an individual in a cluster with a high rate of outcome (ANC visit) and an individual from a cluster with a low rate of outcome (ANC visit) was calculated. The MIRR for the null model became significant (MIRR = 1.20, 95% CI = 1.18,1,21) ( Table 2 ), which tells us doing a multilevel model was preferred over the standard model [ 29 ].
The percent change of variance (PCV) which measures the total variation attributed to individual-level and cluster-level factors was calculated. The deviance test was used to select the best-fitted model and its values are decreasing across model 1 to model 4. Therefore model 4 was the model with the lowest deviance test value and it became the preferred model. The Percent change variation in the final model showed that about 63.6% of the total variability in the number of antenatal care visits was explained by the full model.
Fixed effect results; multilevel negative binomial regression analysis
Maternal age, maternal education, wealth status, media usage, and parity are individual-level factors that had a significant association with the number of ANC visits in the final model. The frequency of ANC visits increased by 8% (AIRR = 1.08, CI = 1.07, 1.10) and 18% (AIRR = 1.18, 95% CI = 1.16, 1.20) for women aged 20–35 and above 35 as compared to women of 15–19 years of age, respectively. Primary education and secondary & above had increased the frequency of ANC visits by 26% (AIRR = 1.26, 95% CI = 1.25, 1.27) and 44% (AIRR = 1.44, 95% CI = 1.42, 1.45) compared with women with no education, respectively. Middle and rich wealth status had increased the frequency of ANC visits by 5% (AIRR = 1.05, 95% CI = 1.04, 1.06) and 8% (AIRR = 1.08, 95% CI = 1.07, 1.09) respectively as compared to women of poor wealth status. Women’s media exposure had increased the frequency of ANC visits by 10% (AIRR = 1.10, 95% CI = 1.09, 1.11) when compared to women with no media exposure. Whereas multiparity and grand multiparity decreased the frequency of ANC visits by 2% (AIRR = 0.98, 95% CI = 0.97, 0.99) and 10% (AIRR = 0.90, 95% CI = 0.89, 0.91) respectively when compared with primiparity. Women with planned pregnancies had 3 percentage points (AIRR = 0.97, 95% CI = 0.96, 0.98) reduced frequency of ANC visits when compared with their counterparts.
Furthermore, community-level factors were significantly associated with the frequency of ANC visits. Women from the rural residence had 10% (AIRR = 0.90, 95% CI = 0.89–0.91) lower ANC visits than their counterparts. Women from Eastern, Southern, and Western SSA regions had 3% (AIRR = 1.03, 95% CI = 1.02, 1.04), 11% (AIRR = 1.11, 95% CI = 1.09, 1.13), and 17% (AIRR = 1.17, 95% CI = 1.16, 1.18) number of ANC visit respectively when compared to women from central SSA region. Women from the community with a high level of media exposure and high level of women’s education had 3% (AIRR = 1.03, 95% CI = 1.02, 1.04) and 2% (AIRR = 1.02, 95% CI = 1.01–1.03) increment with a frequency of ANC visit respectively compared with those from a lower level. Women from middle-income countries had 10% (AIRR = 1.10, 95% CI = 1.09, 1.11) of a greater number of ANC visits compared to their counterparts. In addition, women surveyed from 2012–2015 and 2016–2019 had 5% (AIRR = 1.05, 0.95% CI = 1.04, 1.06) and 7% (AIRR = 1.07, CI = 1.06, 1.08) a greater number of ANC visits when compared with women surveyed from 2008–2011 ( Table 3 ).
https://doi.org/10.1371/journal.pgph.0001180.t003
Antenatal care is an indicator to measure the efficiency of maternal care utilization. It helps in preventing adverse pregnancy outcomes when provided early in the pregnancy and continued through delivery. Identification of problems in pregnancy results in early referrals for women with complications. So this study focused on the mean number of ANC visits and determinants of the number of Antenatal care visits in SSA using the multilevel negative binomial analysis to estimate individual and community-level factors.
This study revealed that although the mean number of ANC visits in SSA approximates the minimum recommended number of ANC visits by the World Health Organization (WHO) [ 1 ], there were still disparities from region to region regarding the number of visits. This might have resulted from inequalities in the accessibility of maternal health services, poor/absence of transportation, inequality in the number of health care providers, and disparities in access to education [ 30 , 31 ]. In addition, this disparity might be due to the difference in the country’s policy and program implementation regarding maternal health service delivery, women’s education, and the role of women in household wealth status [ 32 ]. The other possible reason might be the difference in the implementation of different maternal and child health programs among regions of SSA.
In this study individual and community-level factors are responsible for approximately 64% of differences in the number of ANC visits during pregnancy in Sub-Saharan Africa. In the current study women aged 36–49 and 20–35 years were eighteen and eight percentage points more likely to visit health institutions for ANC service when compared to women aged 15–19 years. The finding supports other studies done previously in different countries [ 33 , 34 ] that showed a positive association between ANC visits and increased age of women. This might be due to birth-related complications and poor health conditions as age advances which trigger the women to demand more visits. In addition, it indicates that young women (15–19 years) probably lack experience in pregnancy care compared to older women [ 9 ].
Our finding also showed that women who had attained primary and secondary and above education were 26 and 44 percentage points more likely to have frequent ANC visits when compared with women with no education respectively. This finding is similar to other studies [ 16 , 35 – 38 ] conducted before in SSA as well as in other countries. This might be a result of the improvement in health literacy as the educational level increase [ 39 ].
Another factor that had a significant relationship with the frequency of ANC visits was whether the pregnancy was planned or not. The study indicated that unwanted pregnancy was 3 percentage points more likely to have a reduced frequency of ANC visits. The finding was consistent with the findings of other studies done before [ 38 , 40 – 42 ]. It is obvious that if the pregnancy was wanted women’s willingness to get health services would increase and there might be early detection of pregnancy, which in turn leads to early booking for ANC, as a result, the frequency of ANC visits would increase.
Furthermore, this study showed that the wealth status of the woman had a positive and significant effect on the frequency of ANC visits. Women from the middle and rich wealth quintiles were more likely to have a frequent number of ANC visits than women from the poor wealth quintile. This finding was consistent with the findings in other studies conducted in different countries [ 13 , 14 , 17 , 43 ]. This indicates that wealth status is an important variable that can influence the frequency of ANC visits. This could be because poor women can not afford transportation fees to a health facility for ANC service utilization. Besides, it can also affect the utilization of ANC services indirectly due to a lack of media exposure and access to education when compared to women with a high wealth status [ 44 , 45 ].
In this study, women’s exposure to mass media has a significant effect on the number of ANC visits. The result showed that women who had media exposure were more likely to have frequent ANC visits than their counterparts. This finding is consistent with previous research [ 9 , 11 , 17 ]. The possible explanation for this finding is that providing women with adequate information about maternal health services increases their utilization of such services. Parity is another factor that had a significant relationship with the frequency of ANC visits. According to our findings, primipara women were more likely to have frequent ANC visits than those with multiparity. In other words, the greater the women’s parity, the less likely they were to have frequent visits. This finding is supported by other previous studies [ 46 – 48 ]. This might be a result of increased confidence from previous birth experiences [ 37 , 49 – 51 ].
Women from rural residences were less likely to have frequent ANC visits. The result was consistent with the findings of studies conducted in different countries [ 44 , 45 , 52 ]. The possible explanation for this is the lack of health facilities in rural areas as compared to urban settings. Furthermore, rural women have no access to health-related information.
Moreover, the geographical region of SSA was found to be a significant factor that could affect the frequency of ANC visits. This study was in line with previously conducted studies [ 11 , 16 , 17 ]. This could be due to disparities in access to health facilities, transportation, and socioeconomic differences.
Our study revealed that women in middle-income countries were more likely to have frequent ANC visits than women in low-income countries. Although no similar study has been conducted, the possible explanations will be improved access to health services, and transportation as the income is higher. Regarding the DHS survey year, women surveyed from 2012–2015 and 2016–2019 were 5 and 7 percentage points more likely to have a greater number of visits than women surveyed from 2008–2011. This might be due to the advancement in the accessibility of health service infrastructures, and the increment in the number of health professionals from time to time.
The current study found that women from high-education communities were more likely to visit healthcare facilities during pregnancy than women from low-education communities. This finding is supported by another study [ 34 ]. This can be explained by herd health literacy where health-related information will be easily accessible in the community.
Women with a high level of media exposure are more likely to have ANC visits than women with a low level of media exposure. The explanation could be that access to the media is an enabling factor for ANC service utilization.
Strength and limitations
This study used large population-based data with a large sample size, which is representative of 35 sub–Saharan African countries. Furthermore, a count data analysis (multilevel Negative Binomial regression analysis) was applied which enabled us to model the effects of each determinant on the frequency of ANC visit efficiently. The novelty of this paper lies in the fact that we have modeled the determinants of the number of antenatal care services in SSA using the most recent DHS data for each country. One significant point of departure of this study is that some countries had no recent DHS data and data from some other countries are not publicly available. Despite the cross-sectional nature of the DHS data, reports of this finding are explained by the incidence rate ratio.
The mean number of ANC visits in SSA approximates the minimum recommended number of ANC visits by the WHO. Maternal education, maternal age above 20 years, media exposure, rich wealth status, high level of community education, high level of media exposure, country GDP, and being from the western and southern regions of SSA increased the frequency of ANC visits. On the other hand, rural residence, multiparity, and unplanned pregnancy negatively affected the frequency of ANC visits. Therefore, this study suggests that addressing geographical disparities and socio-economic inequalities will help alleviate the reduced utilization of ANC services.
Acknowledgments
The authors would like to thank the MEASURE DHS program for the on-request open access to its dataset.
- 1. WHO recommendation on antenatal care for positive pregnancy 27/02/21. Available from: https://apps.who.int/iris/bitstream/10665/250796/1/9789241549912-eng.pdf .
- View Article
- PubMed/NCBI
- Google Scholar
- 3. Unicef for every child, Antenatal care 2021. Available from: https://data.unicef.org/topic/maternal-health/antenatal-care/ .
- 4. WHO, Causes of maternal and child deaths 24/02/21. Available from: https://www.who.int/pmnch/topics/child/countdownreportpages11-21.pdf .
- 5. World bank. Maternal and Child Mortality Development Goals 24/02/21. Available from: https://openknowledge.worldbank.org/handle/10986/17413 .
- 6. WHO. SUSTAINABLE DEVELOPMENT GOAL 3, Ensure healthy lives and promote well-being for all at all ages 2015. Available from: https://sdg-tracker.org/good-health .
- 7. Nation U. The Sustainable Development Goals Report. 2020.
- 10. Antenatal Care Module 03/03/21. Available from: https://www.open.edu/openlearncreate/mod/oucontent/view.php?id=44&print .
- 22. WHO, maternal health 24/02/21. Available from: https://www.afro.who.int/health-topics/maternal-health .
- 24. USAID. Guide to DHS Statistics, DHS-7 (version 2), The Demographic and Health Surveys Program. May 2020.
- 25. Parodi S, Bottarelli E. Poisson regression model in the epidemiology-an introduction [animal diseases]. Annali della Facoltà di Medicina Veterinaria-Università di Parma (Italy). 2006.
- Open access
- Published: 05 April 2024
Availability and readiness of healthcare facilities and their effects on antenatal care services uptake in Bangladesh
- Md. Nuruzzaman Khan 1 , 2 ,
- Md. Badsha Alam 1 ,
- Atika Rahman Chowdhury 1 ,
- Md. Awal Kabir 3 &
- Md. Mostaured Ali Khan 4
BMC Health Services Research volume 24 , Article number: 431 ( 2024 ) Cite this article
Metrics details
Sustainable Development Goal (SDG) 3.7 aims to ensure universal access to sexual and reproductive healthcare services, where antenatal care (ANC) is a core component. This study aimed to examine the influence of health facility availability and readiness on the uptake of four or more ANC visits in Bangladesh.
The 2017/18 Bangladesh Demographic and Health Survey data were linked with the 2017 Health Facility Survey and analyzed in this study. The associations of health facility-level factors with the recommended number of ANC uptakes were determined. A multilevel mixed-effect logistic regression model was used to determine the association, adjusting for potential confounders.
Nearly 44% of mothers reported four or more ANC uptakes, with significant variations across several areas in Bangladesh. The average distance of mothers' homes from the nearest health facilities was 6.36 km, higher in Sylhet division (8.25 km) and lower in Dhaka division (4.45 km). The overall uptake of the recommended number of ANC visits was positively associated with higher scores for the management (adjusted odds ratio (aOR) 1.85; 95% CI, 1.16–2.82) and infrastructure (aOR, 1.59; 95% CI, 1.09–2.19) of health facilities closest to mothers' homes. The odds of using the recommended number of ANC in mothers increased by 3.02 (95% CI, 2.01–4.19) and 2.36 (95% CI, 2.09–3.16) folds for each unit increase in the availability and readiness scores to provide ANC services at the closest health facilities, respectively. Every kilometer increase in the average regional-level distance between mothers' homes and the nearest health facilities reduced the likelihood of receiving the recommended number of ANC visits by nearly 42% (aOR, 0.58, 95% CI, 0.42–0.74).
The availability of healthcare facilities close to residence, as well as their improved management, infrastructure, and readiness to provide ANC, plays a crucial role in increasing ANC services uptake. Policies and programs should prioritize increasing the availability, accessibility, and readiness of health facilities to provide ANC services.
Peer Review reports
Introduction
Maternal mortality is an ongoing public health concern globally, with an estimated 810 deaths every day, mostly from pregnancy-related complications [ 1 ]. Over 99% of these deaths occur in Low- and Middle-Income Countries (LMICs), particularly in Southern Asia (66%) and Sub-Saharan Africa (20%), accounting for approximately 86% of the total global occurrence [ 2 ]. Almost all of these deaths are preventable if basic and cost-effective maternity care is ensured during pregnancy, delivery, and the postpartum period [ 3 ]. As such, ensuring universal access to sexual and reproductive healthcare services, including maternal healthcare services, is an important target to achieve Sustainable Development Goals (SDGs) 3: ensuring health and well-being for all, by 2030.
Antenatal care (ANC) encompasses services provided to pregnant mothers before childbirth and is a crucial maternal healthcare service recommended for all pregnancies. It includes education, screening, counseling, treatment of minor ailments, and immunization services to identify and treat complications through screening and diagnosis. It is also found to be an important determinant of all other types of maternal healthcare services, including delivery and postnatal care [ 4 , 5 ]. ANC alone is estimated to reduce the maternal mortality rate by up to 20% globally; this contribution is around four times higher (80%) in Low- and Middle-Income Countries (LMICs) [ 3 , 6 ].
However, despite its importance in ensuring ANC uptake, around 39% of total pregnant women worldwide do not use the recommended number of ANC services [ 6 ]. The percentage of non-users is even 1.5 times higher in LMICs (50%), mostly in Asian and African countries [ 3 , 6 ]. This lower prevalence of ANC in LMICs is also accompanied by poor-quality ANC services [ 7 , 8 ]. Consequently, dropout from accessing ANC services is very high, and such inadequate care cannot contribute significantly to the reduction of adverse maternal health and birth outcomes, including maternal and under-five mortality [ 8 ].
The government of Bangladesh has made universal access to ANC services as a top priority to achieve the health-related SDGs. For this, the government is now provide ANC services in every maternal and child healthcare providing health facilities with either free of costs or with minimal costs [ 9 ]. Consequently, ANC services use at least once increased over the years, from 34% in 2000 to 82% in 2017/18, although four or more ANC services uptake is still low at 34% [ 10 ]. This lower uptake of four or more ANC services could be due to the poor service quality and need-based use of ANC services only when any complications are faced despite having it’s higher importance to ensure safe pregnancy [ 11 ]. The additional challenges are lack of healthcare equipment and personnel, as well as a lower quality of available services [ 10 , 12 ]. Such challenges have been reported, despite significant progress being achieved during the MDGs, owing primarily to the fixed allocated fund for healthcare services, which causes a mismatch between service availability and demand [ 13 ]. Policies and programs are in place to address these challenges in the field level with comprehensive focus of achieving universal healthcare coverage – as outlined in the SDGs goal [ 14 ]. Although, such a focus, in general, is making significant progress in healthcare services, however, to what extent such improvement of the healthcare facility affects maternal healthcare services is largely unknown in Bangladesh. A similar limitation has been reported in other LMICs. The underlying reason of such lack is the unavailability of linked healthcare facility and households survey data.
Available research on ANC mainly analysed household level data, collected either by national survey or primary survey, and determined individual-, households-, and community characteristics associated with ANC uptake. These include maternal age and education, partner’s education, number of children ever born, wealth index, access to mass media, place of residence and place of region [ 15 , 16 , 17 , 18 ]. Healthcare facility-level factors associated with ANC uptake remain largely understudied in Bangladesh, as well as in LMICs. Importantly, such type of analysis of household level data without considering the healthcare facility level factors underestimate or overestimate the true effects of individual-, household- and community level factors on ANC uptake [ 19 , 20 ]. The underlaying reason is individual-, household-, community-, and healthcare facility level characteristics are interconnected whereas healthcare facility level characteristics work above other factors [ 20 , 21 ]. To address this limitation, we conducted this study to examine the effects of healthcare facility level factors on ANC uptake in Bangladesh, adjusting for individual-, household-, and community-level factors.
Study setting
In this cross-sectional survey data analysis, we analyzed the 2017/18 Bangladesh Demographic and Health Survey (BDHS) and the 2017 Bangladesh Health Facility Survey (BHFS). Both are nationally representative surveys conducted as part of the Demographic and Health Survey (DHS) program by the United States of America (USA) [ 22 , 23 ]. The administrative boundary linkage method was used to link the data from these surveys. Through this method, individual respondents were matched and linked with the nearest healthcare facilities situated within the same administrative unit where the respondents resided. In cases where the respondents' homes had the nearest healthcare facilities located in an administrative division other than their own, such selections were excluded. A more comprehensive description of this method has been published elsewhere [ 22 , 23 ].
The 2017/18 BDHS is the seventh round of DHS in Bangladesh. It was conducted to provide up-to-date information on maternal and child health, including fertility, mortality, and maternal healthcare services use. Nationally representative households were chosen for this survey using stratified random sampling methods in two stages. At the first stage, a total of 675 clusters were selected randomly from a list of 293,579 clusters generated by the Bangladesh Bureau of Statistics as part of the 2011 Bangladesh national population census. Finally, a total of 672 clusters were chosen for the survey, excluding the remaining three clusters due to extreme flooding. The second stage of sampling consisted of selecting a fixed number of 30 households from each of the selected clusters using a simple random sampling method. A list of 20,250 households was generated, of which the survey was conducted in 20,160 households. There were 20,376 eligible women in these selected households with the following conditions: (i) she is a permanent resident of the selected households and passed the most recent night there and (ii) ever married and aged between 15–49 years of age. If a woman spent most of the night at the chosen household but is not a permanent resident of that household, she was also included. With a response rate of 98.8%, a total of 20,127 of the selected women were finally included in the survey.
The 2017 BHFS encompassed 1,524 health facilities, all of which were analyzed in this study. This figure was drawn from a list of 1,600 healthcare facilities generated from the 19,811 registered healthcare facilities in Bangladesh. Each of the 672 PSUs included in the 2017 BDHS and 1,524 healthcare facilities included in the 2017 BHFS has access to GPS point coordinates. Interested readers can see the respective survey reports to know more about these surveys [ 24 , 25 ].
Eligible sample
Total of 4,948 mothers who met the inclusion criteria of this study were analysed. The inclusion criteria were: (i) having at least one livebirth within three years prior to the survey and (ii) providing responses to the access of ANC services along with providers of ANC services. All 1,524 healthcare facilities were also included in the analysis.
Outcome variable
The outcome variable was four or more ANC services use (yes, no). The survey recorded this information by asking women “ Did you receive antenatal healthcare services during your most recent pregnancy? ”. Women who responses positively to this item were then asked, “ How many times did you accessed antenatal healthcare services? ” and “ Where did they receive antenatal healthcare during pregnancy? ”. Women were asked to show the healthcare access card that was used during pregnancy. Number of ANC services received and providers of ANC services, times of accessing ANC services were available in the healthcare access card. If a woman was unable to show the healthcare access card, she was asked several follow-up questions to determine the number, timing, and providers of ANC services. Response recorded were then classified as four or more ANC services access from skilled providers (yes, no).
It is important to mention that we made this classification based on the Bangladesh government’s recommendation of four or more ANC services to receive during pregnancy, rather than the global recommendation of six or more ANC services [ 26 ].
Exposure variables
Health facility-level factors served as a significant exposure variable, with a focus on four key factors: general health service readiness (health facility management systems and infrastructure), degree of availability of antenatal healthcare services at the nearest healthcare facility to mothers' homes, readiness of the nearest healthcare facility to provide antenatal healthcare services, and the average distance between mothers' homes and the nearest healthcare facility (Supplementary Table 1 ). Continuous scores for each factor were generated based on WHO service availability and readiness indicators [ 27 , 28 ], and the procedure for creating these scores is detailed elsewhere [ 29 ]. The calculation of the distance between mothers' residence clusters and the nearest healthcare facility occurred in two stages. Initially, the distance of each cluster to the nearest healthcare facilities was calculated separately for each of the eight administrative divisions. Subsequently, using road communication data, the average distance between mothers' residence clusters and the nearest healthcare facilities was determined. A comprehensive description of this calculation procedure has been published elsewhere [ 20 , 30 ].
The covariates considered were selected by reviewing relevant studies on maternal healthcare services access. For this, we first searched several databases, and the variables considered in the identified papers were summarized. The availability of the summarized variables in the survey we analyzed was then checked. Following this, multicollinearity of the available variables was checked. Following these steps, a list of variables was generated where the variables finally chosen were summarized under three headings following the socio-ecological model of health: individual-level factors, household-level factors, and community-level factors [ 4 , 5 , 10 , 20 , 31 , 32 , 33 , 34 ]. Individual-level factors were mother’s age at the birth of the last child, mother’s education status, mother’s employment status, and pregnancy intention at conception. Household-level factors were partner’s education status, partner’s occupation, number of children ever born, intervals between the two most recent live births, and household wealth status. Place of residence and region (administrative division) were considered in community-level factors.
Statistical analysis
Descriptive statistics were employed to characterize the respondents' features. The association between exposure and outcome variables was assessed using a multilevel mixed-effect logistic regression model at three levels (individuals, households, and clusters), adjusting for factors at the individual, household, and community levels. The rationale for employing the multilevel mixed-effect binary logistic regression model was the hierarchical structure of the BDHS data, where individuals are nested within a household, and households are nested within a cluster [ 35 ]. Ignoring this hierarchy in the model could result in less precise estimates. We ran a total of four models. The initial model, referred to as the null model, included only the outcome variable: the utilization of four or more ANC services. In the second model, healthcare facility-level factors were introduced as independent variables, while the utilization of four or more ANC services remained the dependent variable. This association was then expanded upon in the third and fourth models, where individual and household, as well as community-level factors, respectively, were incorporated as additional independent variables. We also conducted a stratified analysis to assess the association of four or more ANC uptakes with healthcare facility-level factors. Stratification was performed based on the place of residence and the average distance between DHS clusters to the nearest ANC services providing healthcare facility in Bangladesh. Results are reported as odds ratios (OR) with 95% confidence intervals (95% CI). All analyses were performed using the statistical package R (version 4.10).
Background characteristics
Background characteristics of the respondents are presented in Table 1 . Nearly 44% of all respondents reported using four or more ANC services. The rate was even higher among mothers aged 20 to 34 (44.9%, 95% CI, 42.5–47.33) and among unemployed mothers (45.69%, 95% CI, 43.04–48.40). Mothers who had a desired pregnancy at conception reported a higher rate of ANC service utilisation (46.53%, 95% CI, 44.23–48.84) followed by mothers who had a mistimed (40.34%, 95% CI, 35.60–36.51) or an unwanted (27.60, 95% CI, 22.90–32.84) pregnancy at conception. The prevalence of ANC services uptake was found to be much higher among mothers whose partner had more than secondary level education (70.61%, 95% CI, 66.71–74.23) and who were service holders (70.8%, 95% CI, 64.50–73.66). We found lower ANC uptake in mothers who have more than 2 ever born children (33.50%, 95% CI, 30.50–36.70) in comparison to those who had fewer children 48.60% (46.20–51.00). Of the mothers of richest wealth quintile, over 71% (95% CI, 67.32–74.41) reported they uptake four more ANC services. Higher prevalence of four or more ANC services uptake was also reported for urban mothers (56.60%, 95% CI, 52.40–60.70) and mothers whose region of residence were either Khulna (55.23, 95% CI, 49.24—61.07) or Rangpur (52.06%, 95% CI, 56.15–57.91) (Table 1 ).
Distribution of health facilities in Bangladesh
Table 2 presents the distribution of health facilities across divisions. Out of the 1524 health facilities, 1413 (92.71%) offered ANC services. The average distance between these health facilities and the BDHS clusters was approximately 6.36 km, with the highest in the Sylhet division (8.25 km) and the lowest in the Dhaka division (4.45 km). The health facility management system's mean score was 0.81, with the Dhaka division (0.94) scoring higher than Khulna (0.89), Rangpur (0.85), and Mymensingh (0.85) divisions. Similarly, Dhaka (mean score, 0.87) and Rangpur (mean score, 0.72) reported higher availability of various antenatal healthcare services compared to the overall average score of 0.70. The average score for healthcare facility readiness to provide ANC services was 0.67, with the lowest reported in Sylhet (0.46) and Barishal (0.51) divisions.
Model selection
The results of the multilevel mixed-effect logistic regression model assessing the association of ANC services uptake with health facility, individual, household, and community-level factors are presented in Table 3 . Four separate models were run, and the best model is the one with the smallest AIC, BIC, and ICC values. Based on these markers, the final model, model 4, was the best-fitted model. The null model's ICC value was 0.16213, indicating a 16.21% difference in four or more ANC uptakes across clusters considered in the analysis. This reduced to only 6.87% once health facility, individual, family, and community-level factors were adjusted in the final model. The variance of the random intercept decreased from 2.02 to 1.26 as we progressed from the null model to model 4. This decline further indicates that model 4 provided a better fit to the data compared to the previous models.
Association of four or more antenatal care service uptake with health facility-, individual-, family- and community-level factors
The association between the uptake of four or more ANC services and healthcare facility-, individual-, family-, and community-level factors determined through four models is presented in Table 3 . However, since model 4 demonstrated the best fit, we summarize these results here, noting that the findings in other models were directionally similar. We observed that each unit increase in the management and infrastructure scores of the nearest healthcare facility was associated with 1.85 times (95% CI, 1.16–2.82) and 1.59 times (95% CI, 1.09–2.19) higher odds/likelihood of adequate ANC uptake, respectively. The likelihood of ANC service access increased (aOR, 3.02, 95% CI, 2.01—4.19) with an increase in the availability of ANC services at the healthcare facility nearest to mothers’ homes. Similarly, each unit increase in the score of readiness of mothers’ homes nearest healthcare facility was associated with 2.36 times (95% CI, 2.09–3.16) increase in the likelihood of four or more ANC services uptake. Furthermore, we found that for every one-kilometre increase in distance between mothers' homes and the nearest healthcare facility, there was a 42% decrease in the uptake of four or more ANC services.
Of the different covariates adjusted in the final model, mothers' increased years of education, their partner’s occupation other than agricultural workers, a richer wealth quintile, and residing in Khulna, Mymensingh, Rajshahi, and Rangpur were found to be positively associated with an increased uptake of four or more ANC services. In contrast, lower quality of ANC services and experiencing mistimed and unwanted pregnancies rather than wanted pregnancies were found as negative predictors for the uptake of four or more ANC services.
Health facility environment and uptake of four or more antenatal healthcare services
We generated the health facility environment by considering the number of ANC services providing healthcare facilities within 6.36 km (the average distance between DHS cluster to the nearest ANC services providing healthcare facility in Bangladesh). Following this, we ran three different multilevel mixed-effects logistic regression models for overall, rural, and urban areas to access the relationships between four or more ANC service uptake and the health facility environment. Individual, household, and community-level factors were adjusted in each model (Table 4 ). We found the likelihood of ANC services uptake increased with the increased number of healthcare facilities within 6.36 km, and the relationship reported was strongest for the rural area. Increased healthcare facility scores, in response to the management and infrastructure, were found as significant influential predictors of ANC services uptake for all cases, though effect sizes were strongest for rural areas following urban areas and overall. Similarly, the availability of ANC services and the readiness of mothers’ homes nearest healthcare facility to provide ANC services were reported as significant predictors of ANC services uptake for overall and for rural and urban areas separately. However, as before, the relationship was strongest for rural areas.
This study found that improving healthcare facility management and infrastructure, along with increased availability of ANC services at the healthcare facility nearest to mothers' homes and its readiness to provide ANC services, are significant determinants of the uptake of four or more ANC services. We also found that every kilometre increase in distance between mothers' homes and the nearest healthcare facility where ANC services are available is associated with a 42% lower odds of uptake for four or more ANC services. These relationships were observed for Bangladesh as a whole, as well as for its urban and rural areas separately, with the rural areas exhibiting the strongest association. The findings will assist policymakers in prioritizing improvements in healthcare facilities to achieve the SDGs' goal of universal healthcare coverage and a reduction in maternal and child mortality by 2030.
The study found that 44% of women used ANC four or more times, which is 12% higher than the prevalence reported in 2014 [ 33 ], and consistent with prior evidence, socio-economic variation was observed as well [ 33 , 34 , 36 , 37 , 38 , 39 ]. Although the increasing trend indicates progress in ANC uptake, the growth rate is insufficient to meet the SDGs targets by 2030—merely 6 years from now. Moreover, the rate still remains lower than in neighboring countries such as India (51.7%), Nepal (69.8%), and Pakistan (36%) [ 40 , 41 , 42 ]. Additional context-specific policies and programs are now a priority for Bangladesh to increase ANC services uptake to meet the SDGs target by 2030.
We revealed that improving healthcare facility-level factors, including better management and infrastructure, availability of ANC services at the nearest healthcare facility, and its readiness to provide ANC services, play a significant role in increasing the uptake of ANC services. The findings could not be directly validated due to the lack of relevant literature in Bangladesh and other LMICs. However, previous studies in Bangladesh reported a significant influence of healthcare facility-level factors on modern contraception uptake, reducing cesarean delivery, unintended pregnancy, and improving pregnancy outcomes [ 19 , 20 , 43 , 44 , 45 , 46 ]. The association may arise in both direct and indirect ways. Existing evidence showed that adequate infrastructure and the availability of healthcare providers and equipment are key indicators of quality care [ 12 ], which later increases ANC services uptake [ 47 , 48 , 49 ]. In line with our findings, this pathway is commonly observed in Bangladesh and LMICs [ 50 , 51 ].
In Bangladesh, current governmental initiatives to enhance healthcare facility management and infrastructure, as well as the increasing number of healthcare facilities, are on their way to increasing ANC service uptake, although there are challenges that need to be addressed to get best effectiveness of the healthcare facility. For example, a common challenge in Bangladesh is the lack of skilled and enough healthcare personnel. This low provider-patient ratio frequently increases waiting time in facilities, which becomes a burden for pregnant women during ANC check-ups. These circumstances altogether contribute to women dropping out of ANC services. Another significant barrier to ANC service uptake is healthcare facility readiness to provide ANC, which frequently arises as a result of lower governmental priorities to equip Upazila to community level healthcare facilities with required facilities. According to a recent study in Bangladesh, 54.6% of facilities that provide ANC services have at least one ANC-trained staff, while only 4.3% of facilities are fully prepared to provide ANC services [ 31 ]. Although, in total around 13,000 community clinics are available across rural areas of the country and only 33% of the facilities have considerably high preparedness for ANC services [ 31 ]. By policy, they are the primary provider of ANC services, but their lack of readiness impedes women's access to healthcare. All of these factors have a negative impact on women's ANC uptake behaviours, as reflected in our analysis and consistent with other relevant study findings for other outcomes in Bangladesh [ 19 , 20 , 43 ].
However, we found that the increase in distance of mothers’ homes to the nearest healthcare facility reduces women’s ANC services uptake, especially in the rural areas. Our findings corroborates with the findings from other LMICs settings [ 33 , 34 , 36 , 37 , 38 , 39 , 52 , 53 , 54 , 55 , 56 ]. There are several possible explanations for this influence. For instance, increased travel time and costs may contribute to the uptake of healthcare services, particularly for ANC services, which require multiple visits. Moreover, mothers in Bangladesh, like in LMICs, frequently face mobility restrictions due to community-level misconceptions and societal norms [ 19 , 20 ]. This is particularly more evident in the late stages of pregnancy. In addition, there is a tendency in Bangladesh, like in many other LMICs, to access healthcare services based on need rather than considering merits [ 44 ]. This, together with the increased distance, can then contribute to lower uptake of ANC services until serious complications arise. These challenges are common countrywide, particularly in rural areas and among mothers facing socio-economic disadvantages [ 19 , 20 , 44 ].
This study holds significant policy implications aimed at enhancing the utilization of antenatal healthcare services and improving maternal healthcare outcomes. The notable correlation between healthcare facility-level factors and ANC uptake underscores the importance of prioritizing healthcare services alongside the current focus on individual, household, and community-level factors. This necessitates governmental attention towards healthcare services, including enhancing service availability and readiness of healthcare facilities through proper monitoring and strengthening existing infrastructure. The findings also highlight the potential impact of reducing the distance to healthcare facilities on increasing healthcare service uptake. This underscores the importance of initiating ANC services in community clinics across Bangladesh, which serve as primary healthcare centres catering to approximately 6000 individuals. However, to achieve this, the government must ensure the presence of healthcare personnel at these facilities, coupled with infrastructural development efforts. Collectively, these initiatives are poised to bolster ANC uptake towards universal levels, thereby reducing maternal and child mortality rates and advancing the relevant SDGs.
Strengths and limitations
This study has several strengths and a few limitations. First and foremost, as a strength, the study examined two nationally representative datasets that are relatively large and representative of all areas. Second, we used an advanced statistical model to analyze the data, adjusting for potential confounders, which has made the study findings more precise and reliable. However, the major limitation is that the cross-sectional nature of the BDHS survey restricted the study from establishing a causal relationship between exposures and outcomes. The BDHS displaced cluster locations up to 0–5 km for rural areas and 0–2 km for urban areas to ensure the privacy of the respondents. As a result, the calculated average distance between the nearest health facility and the actual distance may differ slightly. The BDHS, on the other hand, ensured that the new disrupted locations remained within the designated administrative boundaries. As a result, errors due to displacement are likely to be random and small. A previous study found that this variation has no effect [ 57 ]. Recall bias is another issue that might have occurred during reported ANC visits and other confounding factors. However, despite these limitations, this is the first study in the context of Bangladesh and other LMICs that explored the effects of health facility-level factors on ANC services uptake in Bangladesh, adjusted for individual, household, and community-level factors. This will help policymakers in Bangladesh and other LMICs to understand why prioritizing healthcare facilities is important to ensure the recommended number of ANC services uptake.
This study revealed a lower uptake of the recommended four or more ANC services. Factors at the healthcare facility level, such as the availability of ANC services, the readiness of healthcare facilities to provide these services, and the proximity of mothers' homes to the nearest healthcare facility, emerged as crucial determinants of the uptake of four or more ANC services. This suggests that significant investment in the healthcare sector is required to ensure the availability of maternal healthcare services at the root level healthcare facilities, such as community clinics. Adequate skilled healthcare personnel need to be recruited and ensured to be present at the community healthcare facility on a 24/7 basis. Health facilities should be strengthened to provide ANC services, and more health facilities with such capacities are needed. For this, policies and programs should prioritize increasing the availability and accessibility of health facilities that provide ANC services.
Availability of data and materials
The data that support the findings of this study are available from The DHS Program, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of The DHS Program ( https://dhsprogram.com/data/ ). Data are, however, available from the corresponding author (Khan MMA via email: [email protected]) upon reasonable request and with permission of the DHS Program.
Abbreviations
Low- and middle-income countries
Sustainable development goal
Antenatal care service
Bangladesh demographic and health survey
Bangladesh health facility survey
Confidence interval
Akaike information criterion
Bayesian information criterion
Ahinkorah BO, Seidu A-A, Budu E, Mohammed A, Adu C, Agbaglo E, Ameyaw EK, Yaya S. Factors associated with the number and timing of antenatal care visits among married women in Cameroon: evidence from the 2018 Cameroon Demographic and Health Survey. J Biosoc Sci. 2022;54(2):322–32.
Article PubMed Google Scholar
Organization WH. Trends in maternal mortality 2000 to 2017: estimates by WHO. UNFPA, World Bank Group and the United Nations Population Division: UNICEF; 2019.
Google Scholar
World Health Organization. Maternal Mortality. Geneva, Switzarland: World Health Organization; 2022.
Khan MN, Harris ML, Loxton D. Assessing the effect of pregnancy intention at conception on the continuum of care in maternal healthcare services use in Bangladesh: Evidence from a nationally representative cross-sectional survey. PLoS ONE. 2020;15(11): e0242729.
Article CAS PubMed PubMed Central Google Scholar
Khan MN, Harris ML, Loxton D. Low utilisation of postnatal care among women with unwanted pregnancy: A challenge for Bangladesh to achieve Sustainable Development Goal targets to reduce maternal and newborn deaths. Health Soc Care Community. 2022;30(2):e524–36.
Hossain AT, Siddique AB, Jabeen S, Khan S, Haider MM, Ameen S, Tahsina T, Chakraborty N, Nahar Q, Jamil K. Maternal mortality in Bangladesh: Who, when, why, and where? A national survey-based analysis. J Global Health. 2023;13:07002.
Article Google Scholar
Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. 2017;7(11): e017122.
Article PubMed PubMed Central Google Scholar
Merid MW, Chilot D, Yigzaw ZA, Melesse AW, Ferede MG, Aragaw FM, Bitew DA. Women in low-and middle-income countries receive antenatal care at health institutions, yet not delivered there: a multilevel analysis of 2016–2021 DHS data. Trop Med Health. 2024;52(1):1.
Khan MN, Harris M, Loxton D. Modern Contraceptive Use Following an Unplanned Birth in Bangladesh: An Analysis of National Survey Data. Int Perspect Sex Reprod Health. 2020;46:77–87.
Mn KHAN. Effects of Unintended Pregnancy on Maternal Healthcare Services Use in Bangladesh. Faculty of Health and Medicine: School of Medicine and Public Health, The; 2020. p. 1.
Sarker BK, Rahman M, Rahman T, Rahman T, Khalil JJ, Hasan M, Rahman F, Ahmed A, Mitra DK, Mridha MK. Status of the WHO recommended timing and frequency of antenatal care visits in Northern Bangladesh. PLoS ONE. 2020;15(11): e0241185.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, Adeyi O, Barker P, Daelmans B, Doubova SV. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–252.
Beattie R, Brown N, Cass H. Millennium development goals progress report. Arch Dis Child. 2015;100(Suppl 1):S1–S1.
Joarder T, Chaudhury TZ, Mannan I. Universal health coverage in Bangladesh: activities, challenges, and suggestions. Adv Public Health. 2019;1–12.
Rahman A, Nisha MK, Begum T, Ahmed S, Alam N, Anwar I. Trends, determinants and inequities of 4+ ANC utilisation in Bangladesh. J Health, Popul Nutr. 2017;36(1):1–8.
Sarker BK, Rahman T, Rahman T, Rahman M. Factors associated with the timely initiation of antenatal care: findings from a cross-sectional study in Northern Bangladesh. BMJ Open. 2021;11(12): e052886.
Ali N, Sultana M, Sheikh N, Akram R, Mahumud RA, Asaduzzaman M, Sarker AR. Predictors of optimal antenatal care service utilization among adolescents and adult women in Bangladesh. Health Serv Rep and Managerial Epidemiol. 2018;5:2333392818781729.
Pervin J, Venkateswaran M, Nu UT, Rahman M, O’Donnell BF, Friberg IK, Rahman A, Frøen JF. Determinants of utilization of antenatal and delivery care at the community level in rural Bangladesh. PLoS ONE. 2021;16(9): e0257782.
Khan N, Islam Trisha N, Rashid M. Availability and readiness of health care facilities and their effects on under-five mortality in Bangladesh: Analysis of linked data. J Glob Health. 2022;12:04081.
Khan MN, Akter S, Islam MM. Availability and readiness of healthcare facilities and their effects on long-acting modern contraceptive use in Bangladesh: analysis of linked data. BMC Health Serv Res. 2022;22(1):1180.
Kilanowski JF. Breadth of the socio-ecological model. J Agromedicine. 2017;22(4):295–7.
PubMed Google Scholar
Burgert CR, Prosnitz Debra. Linking DHS Household and SPA Facility Surveys: Data Considerations and Geospatial Methods. In: DHS Spatial Analysis Reports No. 10. Rockville, Maryland, USA: ICF International; 2014.
Kanyangarara M, Chou VB, Creanga AA, Walker N. Linking household and health facility surveys to assess obstetric service availability, readiness and coverage: evidence from 17 low-and middle-income countries. J Global Health. 2018;8(1):010603.
National Institute of Population Research and Training (NIPORT) and ICF. Bangladesh Health Facility Survey. Dhaka, Bangladesh: NIPORT, and ICF; 2017.
National Institute of Population Research and Training (NIPORT) and ICF. Bangladesh Demography and Health Survey. Dhaka, Bangladesh: NIPORT, and ICF; 2017.
Directorate General of Health Services (DGHS). Bangladesh national strategy for maternal health 2019–2030. In: Dhaka, Bangladesh Ministry of Health and Family Welfare. 2019.
Organization WH. Service availability and readiness assessment (SARA): an annual monitoring system for service delivery: reference manual. In.: World Health Organization; 2013.
O’Neill K, Takane M, Sheffel A, Abou-Zahr C, Boerma T. Monitoring service delivery for universal health coverage: the Service Availability and Readiness Assessment. Bull World Health Organ. 2013;91:923–31.
Cummins D. Teenage pregnancy and early marriage in Timor-Leste: Research on the decision-making pathways of young women in the Municipalities of Covalima. Timor-Leste UNFPA: Aileu and Dili. Dili; 2017.
Tegegne TK, Chojenta C, Forder PM, Getachew T, Smith R, Loxton D. Spatial variations and associated factors of modern contraceptive use in Ethiopia: a spatial and multilevel analysis. BMJ Open. 2020;10(10): e037532.
Hakim S, Chowdhury MAB, Ahmed Z, Uddin MJ. Are Bangladeshi healthcare facilities prepared to provide antenatal care services? Evidence from two nationally representative surveys. PLOS Glob Public Health. 2022;2(7): e0000164.
Khan MA, Khan N, Rahman O, Mustagir G, Hossain K, Islam R, Khan HT. Trends and projections of under-5 mortality in Bangladesh including the effects of maternal high-risk fertility behaviours and use of healthcare services. PLoS ONE. 2021;16(2): e0246210.
Khan MN, Harris ML, Oldmeadow C, Loxton D. Effect of unintended pregnancy on skilled antenatal care uptake in Bangladesh: analysis of national survey data. Arch Public Health. 2020;78(1):1–13.
Talukder A, Siddiquee T, Noshin N, Afroz M, Ahammed B, Halder HR. Utilization of Antenatal Care Services in Bangladesh: A Cross-sectional Study Exploring the Associated Factors. The Anatolian J FamMed. 2021;4(1):49.
Diez-Roux AV. Multilevel Analysis in Public Health Research. Annu Rev Public Health. 2000;21(1):171–92.
Article CAS PubMed Google Scholar
Chanda SK, Ahammed B, Howlader MH, Ashikuzzaman M. Shovo T-E-A, Hossain MT: Factors associating different antenatal care contacts of women: A cross-sectional analysis of Bangladesh demographic and health survey 2014 data. PLoS ONE. 2020;15(4): e0232257.
Islam MM, Masud MS. Determinants of frequency and contents of antenatal care visits in Bangladesh: Assessing the extent of compliance with the WHO recommendations. PLoS ONE. 2018;13(9): e0204752.
Islam MA, Kabir MR, Talukder A. Triggering factors associated with the utilization of antenatal care visits in Bangladesh: An application of negative binomial regression model. Clin Epidemiol Glob Health. 2020;8(4):1297–301.
Bhowmik KR, Das S, Islam MA. Modelling the number of antenatal care visits in Bangladesh to determine the risk factors for reduced antenatal care attendance. PLoS ONE. 2020;15(1): e0228215.
Ogbo FA, Dhami MV, Ude EM, Senanayake P, Osuagwu UL, Awosemo AO, Ogeleka P, Akombi BJ, Ezeh OK, Agho KE. Enablers and barriers to the utilization of antenatal care services in India. Int J Environ Res Public Health. 2019;16(17):3152.
Neupane B, Rijal S, Gc S, Basnet TB. Andersen’s model on determining the factors associated with antenatal care services in Nepal: an evidence-based analysis of Nepal demographic and health survey 2016. BMC Pregnancy Childbirth. 2020;20(1):1–11.
Sahito A, Fatmi Z. Inequities in antenatal care, and individual and environmental determinants of utilization at national and sub-national level in Pakistan: a multilevel analysis. International J Health Policy Manag. 2018;7(8):699.
Khan M, Harris ML, Huda M, Loxton D. A population-level data linkage study to explore the association between health facility level factors and unintended pregnancy in Bangladesh. Sci Rep. 2022;12(1):1–11.
Khan MN, Islam MM, Akter S. Spatial distribution of caesarean deliveries and their determinants in Bangladesh evidence from linked data of population and health facility survey. Lancet Reg Health Southeast Asia. 2023;14:100153.
Kabir MA, Rahman MM, Khan MN. Maternal anemia and risk of adverse maternal health and birth outcomes in Bangladesh: A nationwide population-based survey. PLoS ONE. 2022;17(12): e0277654.
Khan MN, Kabir MA, Shariff AA, Rahman MM. Too many yet too few caesarean section deliveries in Bangladesh: Evidence from Bangladesh Demographic and Health Surveys data. PLOS Global Public Health. 2022;2(2): e0000091.
Zhongming Z, Linong L, Xiaona Y, Wangqiang Z, Wei L. Low quality healthcare is increasing the burden of illness and health costs globally. 2018.
Tadesse Berehe T, Modibia LM. Assessment of quality of antenatal care services and its determinant factors in public health facilities of Hossana town. Hadiya zone, Southern Ethiopia: A Longitudinal Study. Advances in Public Health; 2020. p. 2020.
Puspitasari DA, Omas Bulan S. The effect of accessibility and availability of health infrastructure on maternal healthcare utilization in Indonesia to achieve Sustainable Development Goals. IOP Conference Series: Earth Environ Sci. 2021;716(1): 012110.
Negash WD, Fetene SM, Shewarega ES, Fentie EA, Asmamaw DB, Teklu RE, Aragaw FM, Belay DG, Alemu TG, Eshetu HB. Multilevel analysis of quality of antenatal care and associated factors among pregnant women in Ethiopia: a community based cross-sectional study. BMJ Open. 2022;12(7): e063426.
Anwar I, Nababan HY, Mostari S, Rahman A, Khan JA. Trends and inequities in use of maternal health care services in Bangladesh, 1991–2011. PLoS ONE. 2015;10(3): e0120309.
Fisseha G, Berhane Y, Worku A, Terefe W. Distance from health facility and mothers’ perception of quality related to skilled delivery service utilization in northern Ethiopia. Int J Women’s Health. 2017;9:749–56.
Dotse-Gborgbortsi W, Dwomoh D, Alegana V, Hill A, Tatem AJ, Wright J. The influence of distance and quality on utilisation of birthing services at health facilities in Eastern Region, Ghana. BMJ Glob Health. 2020;4(Suppl 5): e002020.
Steinbrook E, Min MC, Kajeechiwa L, Wiladphaingern J, Paw MK, Pimanpanarak MPJ, Hiranloetthanyakit W, Min AM, Tun NW, Gilder ME, et al. Distance matters: barriers to antenatal care and safe childbirth in a migrant population on the Thailand-Myanmar border from 2007 to 2015, a pregnancy cohort study. BMC Pregnancy Childbirth. 2021;21(1):802.
Seidu A-A. A multinomial regression analysis of factors associated with antenatal care attendance among women in Papua New Guinea. Public Health Prac. 2021;2: 100161.
Muchie KF. Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: a finding based on a demographic and health survey. BMC Pregnancy Childbirth. 2017;17(1):1–7.
Sato R, Elewonibi B, Mhande M, Msuya S, Shah I. Canning D: Distance to Facility and Healthcare Utilization in Tanzania: Unbiased and Consistent Estimation using Perturbed Location Data. USA Population Association of America: Population Association of America New York; 2019.
Download references
Acknowledgements
The authors thank the MEASURE DHS for granting access to the 2017/18 BDHS data. We are grateful to Department of Population Science of Jatiya Kabi Kazi Nazrul Islam University, where this study was designed and conducted. We also acknowledge the support of maternal and child health division (MCHD) of icddr,b and its core donors the Governments of Bangladesh, Canada, Sweden and the UK for providing unrestricted support for its operations and research.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Population Science, Jatiya Kabi Kazi Nazrul Islam University, Namapara, Mymensingh, 2220, Bangladesh
Md. Nuruzzaman Khan, Md. Badsha Alam & Atika Rahman Chowdhury
School of Medicine and Public Health, College of Health, Medicine and Well-Being, The University of Newcastle, NSW 2308, Callaghan, Australia
Md. Nuruzzaman Khan
Department of Social Work, Pabna University of Science and Technology, Pabna, 6600, Bangladesh
Md. Awal Kabir
Maternal and Child Health Division (MCHD), icddr,b, 68 Shaheed Tajuddin Ahmed Sarani, Mohakhali, Dhaka, 1212, Bangladesh
Md. Mostaured Ali Khan
You can also search for this author in PubMed Google Scholar
Contributions
Khan MN and Khan MA designed the study. Khan MN performed the data analysis. Khan MN, Chowdhury AR, Alam MB, and Kabir MA wrote the first draft of this manuscript. Khan MN and Khan MA critically reviewed and edited the previous versions of this manuscript. All authors approved this final version of the manuscript.
Corresponding author
Correspondence to Md. Mostaured Ali Khan .
Ethics declarations
Ethics approval and consent to participate.
We utilized secondary data extracted from the 2017 Bangladesh Demographic and Health Survey (BDHS). This survey received approval from the Institutional Review Board of ICF and the National Research Ethics Committee of the Bangladesh Medical Research Council. Informed consent was obtained from all participants, and for participants under the age of 16, consent was also obtained from their guardian. All necessary patient/participant consent forms have been acquired, and relevant institutional documentation has been archived. No separate ethical approval was required for this study, as we were granted access to the survey data and authorized to conduct our research. All methods were conducted in compliance with applicable guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Khan, M.N., Alam, M.B., Chowdhury, A.R. et al. Availability and readiness of healthcare facilities and their effects on antenatal care services uptake in Bangladesh. BMC Health Serv Res 24 , 431 (2024). https://doi.org/10.1186/s12913-024-10824-4
Download citation
Received : 02 April 2023
Accepted : 05 March 2024
Published : 05 April 2024
DOI : https://doi.org/10.1186/s12913-024-10824-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Antenatal care
- Healthcare facility level factors
- Linked data
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

Antenatal care – at least eight visits
Antenatal care – at least eight visits.
Definition:
The number of women of reproductive age with a live birth in a specified reference period who received antenatal care (ANC) eight or more times from any provider is expressed as a percentage of women in the same age range with a live birth in the same period.
Data Sources:
There are two common data sources for this indicator:
Routinely collected administrative data
Population-based household surveys
Data from routinely collected and compiled administrative data sources will provide information as recorded in medical charts/ records or registers and are entered into national and/or subnational health information systems:
- Health information management system (HMIS) and/or
- District Health Information Management System (DHIS2)
Routinely collected administrative data and health facility statistics are the preferred data source in settings with a high utilization of health facility services and data are recorded in a manner that ensures good data quality for both the public and private health sectors.
Key source of data: Administrative data sources include health facility and health services data abstracted from obstetric and neonatal medical records. Relevant information is recorded about the number and timing of ANC visits among all women who attended ANC during pregnancy within health facilities on paper forms completed by health personnel and/or through an electronic medical record. Data from paper or electronic sources are entered or abstracted into a database or registry and are compiled and analysed within the national and/ or subnational HMIS. The Ministry of Health (MoH) and/or National Statistical Offices (NSO) are usually responsible for the reporting of this indicator.
Indicator definition and calculation: The indicator is calculated as the percentage of women who received ANC eight times from any provider among all births in a health facility during a specified reference period.
Numerator: Number of antenatal clients with eighth ANC visit.
Denominator: Total number of antenatal clients with a first ANC visit.
Unless specified, the statistic may include any woman regardless of age and includes both live births and stillbirths, as defined by the health facility and/or national or subnational vital statistics offices. The numerator and denominator definition of ANC is based on individual health facility report or is in accordance with the country-specific definition by the MoH and/or NSO.
Frequency of measurement: The indicator can be calculated on an annual basis or may be tracked on a more frequent and ongoing basis (e.g. monthly, quarterly), depending on facility, subnational and national processes for data entry, compilation and analysis. As a guide, the recommended frequency of measurement based on reporting level is outlined below:
- Facility level: Monthly, quarterly, or as needed based on the country and/or facility need
- Subnational (first and second administrative) level: Monthly or quarterly
- National level: Annually (data can be aggregated to provide national-level data).
Disaggregation: By level of facility, location of facility (e.g., urban, rural), type of health personnel, and timing of ANC visit. Missing values: Missing values are usually not known, or not reported.
The main source of data for this indicator has been through population-based household surveys collected through nationally or sub-nationally representative and statistically sound questionnaires, such as:
- Demographic Health Surveys (DHS)
- Multiple Indicator Cluster Surveys (MICS)
- Reproductive Health Surveys (RHS)
- Other household surveys with a similar methodological design.
Population-based household survey data are the preferred data source in settings with a low utilization of health facility services, or where private health sector data are excluded from routinely collected administrative data sources.
Key source of data: Eligible women of reproductive age (15–49 years) are identified in the household survey for inclusion and interviewed using an individual women’s questionnaire. Women are considered eligible for survey interview if they are either usual residents or visitors of the household who stayed there the night before the interview. All eligible and interviewed women between 15 and 49 years of age who had a live birth during a specified reference period, typically 2–5 years prior to the time of interview, are asked “Did you see anyone for antenatal care for this pregnancy?”, in reference to the last live birth the individual woman had during the same reference period. If women saw anyone for ANC, they are then asked to identify “How many times did you receive antenatal care during this pregnancy?” MoH and NSO typically conduct household surveys and compile, analyze and report the results for this indicator in collaboration with the survey program (e.g., DHS, MICS, RHS) and funding agency.
Indicator definition and calculation: Individual women of reproductive age (15–49 years old) are asked about ANC visits for their most recent live birth. Questions about ANC visits are asked, irrespective of the child’s current living status (dead or alive), and are for live births that they have had during a specified reference period, which is typically 2–5 years before the time of the survey completion. The definition is as follows:
The percentage of interviewed women (aged 15 to 49 years) with a live birth in the 2–5 years prior to survey completion who received ANC at least eight times from any provider.
The indicator consists of the following numerator and denominator:
Numerator: Number of interviewed women (aged 15–49 years) with a live birth who received ANC at least eight times from any provider
Denominator: Total number of women (aged 15–49 years) with a live birth. Frequency of measurement: Household surveys are typically conducted every 3–5 years.
Disaggregation at population level: Type of health personnel, place of delivery, mode of delivery, place of residence (e.g., urban, rural), sex of live birth, birth order, socioeconomic status (e.g., education level, wealth quintile), age of woman at the time of delivery, and births attended by skilled health personnel.
Missing values: Included in the distribution as “don’t know” and /or “missing”.
ANC is a critical component for improving maternal and newborn health and provides a platform for important healthcare functions, including: health promotion, screening and diagnosis, injury and disease prevention, as well as birth preparedness and preparation for the postnatal period. By implementing timely and appropriate evidence-based practices, ANC can reduce morbidity and mortality and optimize overall health and well-being. ANC also provides the opportunity to communicate with and support women, families and communities at a critical time in the course of a woman’s life. ANC comprises effective communication about physiological, biomedical, behavioral and sociocultural issues, as well as emotional and psychological support, to pregnant women in a respectful way (WHO, 2013; WHO, 2016; Lattof, et al, 2020).
This indicator helps program management at global, national and subnational levels by monitoring and evaluating perinatal outcomes and using data to make informed decisions about the planning, development and evaluation of health services delivery and initiatives. The antenatal period presents opportunities for reaching pregnant women with interventions that may be vital to both maternal, fetal and newborn health and well-being. WHO previously recommended that pregnant women complete at least four ANC visits. However, new guidelines from the WHO ANC Model (2018) increase the recommended number of contacts a pregnant woman has with health providers throughout her pregnancy from four to eight visits, and future programs should consider measuring based on these guidelines (WHO, 2016). This indicator should be interpreted with caution as it is a measure of contact with the health system and does not take into account the content and quality of care received. Receiving ANC during pregnancy does not guarantee the receipt of evidenced-based interventions that are effective in improving maternal and newborn health and survival. It should not be assumed that women received ANC in accordance with WHO, other international organizations, and/or country-specific recommendations or guidelines. Therefore, this indicator should be complemented with information on the content and quality of interventions received during each ANC contact in order to more effectively monitor and evaluate the effectiveness and impact of maternal and newborn health interventions.
Data collected from administrative and other routine data systems
Administrative data may suffer from poor quality such as irregularities in report generation, data duplication and inconsistencies (Abouzahr and Boerma, 2005). Reporting challenges exist at the facility level given data quality issues, including incomplete, inaccurate and lack of timely data due to insufficient capacity in the health system or inadequate system design.
Many HMIS databases or registries are event-based and only include ANC information for women who delivered a birth at a health facility. In some instances, the denominator may include births delivered by women of an unspecified age range and include both live births and stillbirths. In addition, the definition of a stillbirth varies by country and context, such as differences in inclusion for gestational age (e.g., 20–28 weeks) and birthweight (e.g. ≥ 500 grams). As this often only represents those women who present to health facilities for ANC, it does not capture the number of pregnancies and demand for ANC within the total population. These differences in definitions compromise the ability to compare data between countries.
Administrative data should be interpreted with caution in settings where data quality is poor and the percentage of births at public and private sector health facilities is low, or where data from the private health sector are not compiled within the HMIS reporting.
In settings where routine HMIS data lack information on pregnancies and/or births that occur outside the public sector – for example, in homes or private sector facilities – the total number of births in the HMIS should not serve to estimate the denominator for this indicator. Where data on the total numbers of live births for the entire population for the denominator are unavailable, evaluators can calculate total estimated live births using census data for the total population and crude birth rates in a specified area (total expected live births = estimated population x the total crude birth rate).
Data collected through household surveys
Women may not be able to accurately recall details around childbirth when data are collected through household surveys (Blanc, et al, 2016). There is also a time lag as the recall period is from two to five years before the survey data are collected.
The most commonly used denominator is the number of live births, which acts as a proxy for the number of pregnant women. However, inclusion of only live births underestimates the total number of pregnancies by excluding those that end in stillbirth or spontaneous or induced abortion, as well as ectopic and molar pregnancies. It also causes survivor bias in that only those women who are alive at the time of interview would be included and underestimates the total number of women requiring care during pregnancy.
The indicator usually measures visits with any provider because national-level household surveys do not collect provider data for each visit. In addition, standardization of the definition of health personnel is sometimes difficult because of differences in naming conventions, competencies and training of health personnel between and within countries (WHO, 2018).
For more information on this indicator, please see the MoNITOR indicator reference sheet developed by the World Health Organization: Who-indicators (srhr.org) .
References:
- WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016.
- Every Woman Every Child. Indicator and monitoring framework for the Global Strategy for Women’s, Children’s and Adolescents’ Health (2016–2030). Geneva: World Health Organization; 2016.
- Lattof SR, Moran AC, Kidula N, Moller AB, Chayathilaka CA, Diaz T, Tunçalp Ö. Implementation of the new WHO antenatal care model for a positive pregnancy experience: a monitoring framework. BMJ Glob Health. 2020;5(6):e002605 (https://gh.bmj.com/content/5/6/ e002605.long)
- The DHS Program [website]. Rockville: ICF International; 2020 (http://www.dhsprogram. com/)
- Multiple Indicator Cluster Surveys (MICS) [website]. New York: UNICEF; 2020 (http://mics. unicef.org)
- Abouzahr C, Boerma T. Health information systems: the foundations of public health. Bull World Health Organ. 2005;83(8): 578–83.
- Blanc AK, Diaz C, McCarthy KJ, Berdichevsky K. Measuring progress in maternal and newborn health care in Mexico: validating indicators of health system contact and quality of care. BMC Pregnancy Childbirth. 2016;16(1):255 ( https://doi.org/10.1186/s12884-016-1047- 0 )
- Definition of skilled health personnel providing care during childbirth: the 2018 joint statement by WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA. Geneva: World Health Organization; 2018
Related content:
Health System Strengthening
Newborn Health
Factors Associated with Numbers of Antenatal Care Visits in Rural Ethiopia
Affiliations.
- 1 Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
- 2 Department of Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
- 3 Department of Biomedical Sciences, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia.
- PMID: 34140778
- PMCID: PMC8203265
- DOI: 10.2147/JMDH.S308802
Introduction: Antenatal care (ANC) is a medical care and procedure carried out for pregnant women. Data on ANC visits can help policymakers show gaps in service provision. Therefore, this study assessed the factors associated with the number of ANC visits among women in rural Ethiopia.
Methods: We included a total of 6611 women who gave birth within 5 years preceding the survey from the 2016 Ethiopian Demographic and Health Survey. A multi-level negative binomial regression analysis was employed to consider the hierarchical nature of the data. In the multivariable analysis, variables with a p-value <0.05 were considered to be significantly associated with the number of ANC visits.
Results: Overall, 27.3% (95% CI: 14.63, 15.76) of women had at least four ANC visits during pregnancy in rural Ethiopia. Among individual level factors, age group 25-29 years (adjusted incidence rate ratio (AIRR)=1.13,95% CI:1.02,1.26), household rich wealth status (AIRR=1.17, 95% CI:1.04,1.31), women's educational status (primary, AIRR=1.19,95% CI:1.08,1.32; secondary, AIRR= 1.30,95% CI:1.08,1.55; above secondary, AIRR=1.35, 95% CI:1.07,1.71), partner educational status (primary, AIRR=1.16, 95% CI:1.05,1.28; secondary, AIRR=1.22,95% CI:1.08,1.38), and autonomy to decision to their care (AIRR=1.25,95% CI:1.10,1.42) were positively associated factors whereas having a birth order of five or more (AIRR=0.80,95% CI: 0.69,0.94) was a negative associated with number of ANC visits. Among community-level variables, being in higher community level literacy (AIRR=1.35, 95% CI: 1.14, 1.59) and higher poverty level (AIRR=0.77, 95% CI: 0.64, 0.92) were significant factors with the number of ANC visits.
Conclusions and recommendations: Women's age, wealth status, women's educational status, partner educational status, autonomy to decision making in health care, and birth order were determinants of the number of ANC visits. Furthermore, poverty and literacy are also important factors at the community level. Addressing economic and educational interventions for rural women should be prioritized.
Keywords: antenatal care; multilevel negative binomial count analysis; rural Ethiopia; women.
© 2021 Mamuye Azanaw et al.
Grants and funding
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd edition. Geneva: World Health Organization; 2015.

Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd edition.
C antenatal care.
- Always begin with Rapid assessment and management (RAM) B3-B7 . If the woman has no emergency or priority signs and has come for antenatal care, use this section for further care.
- Next use the Pregnancy status and birth plan chart C2 to ask the woman about her present pregnancy status, history of previous pregancies, and check her for general danger signs. Decide on an appropriate place of birth for the woman using this chart and prepare the birth and emergency plan. The birth plan should be reviewed during every follow-up visit.
- Check all women for pre-eclampsia, anaemia, syphilis and HIV status according to the charts C3 - C6 .
- In cases where an abnormal sign is identified (volunteered or observed), use the charts Respond to observed signs or volunteered problems C7 - C11 to classify the condition and identify appropriate treatment(s).
- Give preventive measures due C12 .
- Develop a birth and emergency plan C14-C15 .
- Advise and counsel on nutrition C13 , family planning C16 , labour signs, danger signs C15 , routine and follow-up visits C17 using Information and Counselling sheets M1 -M19 .
- Record all positive findings, birth plan, treatments given and the next scheduled visit in the home-based maternal card/clinic recording form.
- Assess eligibility of ART for HIV-infected woman C19 .
- If the woman is HIV infected, adolescent or has special needs, see G1 - G11 H1 - H4 .
C2. ASSESS THE PREGNANT WOMAN: PREGNANCY STATUS, BIRTH AND EMERGENCY PLAN
Use this chart to assess the pregnant woman at each of the four antenatal care visits. During first antenatal visit, prepare a birth and emergency plan using this chart and review them during following visits. Modify the birth plan if any complications arise.
View in own window

C3. CHECK FOR PRE-ECLAMPSIA
Screen all pregnant women at every visit.
C4. CHECK FOR ANAEMIA
C5. check for syphilis.
Test all pregnant women at first visit. Check status at every visit.
C6. CHECK FOR HIV STATUS
Test and counsel all pregnant women for HIV at the first antenatal visit. Check status at every visit.
If no problem, go to page C12 .
C7-C11. RESPOND TO OBSERVED SIGNS OR VOLUNTEERED PROBLEMS
C12. give preventive measures.
Advise and counsel all pregnant women at every antenatal care visit.
C13. ADVISE AND COUNSEL ON NUTRITION AND SELF-CARE AND SUBSTANCE ABUSE
Use the information and counselling sheet to support your interaction with the woman, her partner and family.
Counsel on nutrition
- Advise the woman to eat a greater amount and variety of healthy foods, such as meat, fish, oils, nuts, seeds, cereals, beans, vegetables, cheese, milk, to help her feel well and strong (give examples of types of food and how much to eat).
- Spend more time on nutrition counselling with very thin, adolescent and HIV-infected woman.
- Determine if there are important taboos about foods which are nutritionally important for good health. Advise the woman against these taboos.
- Talk to family members such as the partner and mother-in-law, to encourage them to help ensure the woman eats enough and avoids hard physical work.
Advise on self-care during pregnancy
Advise the woman to:
- Take iron tablets F3 .
- Rest and avoid lifting heavy objects.
- Sleep under an insecticide impregnated bednet.
- Counsel on safer sex including use of condoms, if at risk for STI or HIV G2 .
- Avoid alcohol and smoking during pregnancy.
- NOT to take medication unless prescribed at the health centre/hospital.
Counsel on Substance Abuse:
- Avoid tobacco use during pregnancy.
- Avoid exposure to second-hand smoke.
- Do not take any drugs or Nicotine Replacement Therapy for tobacco cessation.
Counsel on alcohol use:
- Avoid alcohol during pregnancy.
Counsel on drug use:
- Avoid use of drugs during pregnancy.
C14-C15. DEVELOP A BIRTH AND EMERGENCY PLAN
Facility delivery.
Explain why birth in a facility is recommended
- Any complication can develop during delivery - they are not always predictable.
- A facility has staff, equipment, supplies and drugs available to provide best care if needed, and a referral system.
- If HIV-infected she will need appropriate ARV treatment for herself and her baby during childbirth.
- Complications are more common in HIV-infected women and their newborns. HIV-infected women should deliver in a facility.
Advise how to prepare
Review the arrangements for delivery:
- How will she get there? Will she have to pay for transport?
- How much will it cost to deliver at the facility? How will she pay?
- Can she start saving straight away?
- Who will go with her for support during labour and delivery?
- Who will help while she is away to care for her home and other children?
Advise when to go
- If the woman lives near the facility, she should go at the first signs of labour.
- If living far from the facility, she should go 2-3 weeks before baby due date and stay either at the maternity waiting home or with family or friends near the facility.
- Advise to ask for help from the community, if needed I2 .
Advise what to bring
- Home-based maternal record.
- Clean cloths for washing, drying and wrapping the baby.
- Additional clean cloths to use as sanitary pads after birth.
- Clothes for mother and baby.
- Food and water for woman and support person.
Home delivery with a skilled attendant
- Review the following with her:
- Who will be the companion during labour and delivery?
- Who will be close by for at least 24 hours after delivery?
- Who will help to care for her home and other children?
- Advise to call the skilled attendant at the first signs of labour.
- Advise to have her home-based maternal record ready.
Explain supplies needed for home delivery
- Warm spot for the birth with a clean surface or a clean cloth.
- Clean cloths of different sizes: for the bed, for drying and wrapping the baby, for cleaning the baby's eyes, for the birth attendant to wash and dry her hands, for use as sanitary pads.
- Buckets of clean water and some way to heat this water.
- Bowls: 2 for washing and 1 for the placenta.
- Plastic for wrapping the placenta.
Advise on labour signs
Advise to go to the facility or contact the skilled birth attendant if any of the following signs:
- a bloody sticky discharge.
- painful contractions every 20 minutes or less.
- waters have broken.
Advise on danger signs
Advise to go to the hospital/health centre immediately, day or night, WITHOUT waiting if any of the following signs:
- vaginal bleeding.
- convulsions.
- severe headaches with blurred vision.
- fever and too weak to get out of bed.
- severe abdominal pain.
- fast or difficult breathing.
- She should go to the health centre as soon as possible if any of the following signs:
- abdominal pain.
- swelling of fingers, face, legs.
Discuss how to prepare for an emergency in pregnancy
where will she go?
how will they get there?
how much it will cost for services and transport?
can she start saving straight away?
who will go with her for support during labour and delivery?
who will care for her home and other children?
- Advise the woman to ask for help from the community, if needed I1 – I3 .
- Advise her to bring her home-based maternal record to the health centre, even for an emergency visit.
C16. ADVISE AND COUNSEL ON FAMILY PLANNING
Counsel on the importance of family planning.
- If appropriate, ask the woman if she would like her partner or another family member to be included in the counselling session.
Ask about plans for having more children. If she (and her partner) want more children, advise that waiting at least 2 years before trying to become pregnant again is good for the mother and for the baby's health.
Information on when to start a method after delivery will vary depending whether a woman is breastfeeding or not.
Make arrangements for the woman to see a family planning counsellor, or counsel her directly (see the Decision-making tool for family planning providers and clients for information on methods and on the counselling process).
- Counsel on safer sex including use of condoms for dual protection from sexually transmitted infections (STI) or HIV and pregnancy. Promote especially if at risk for STI or HIV G4 .
- For HIV-infected women, see G4 for family planning considerations
- Her partner can decide to have a vasectomy (male sterilization) at any time.
Method options for the non-breastfeeding woman
Special considerations for family planning counselling during pregnancy.
Counselling should be given during the third trimester of pregnancy.
can be performed immediately postpartum if no sign of infection (ideally within 7 days, or delay for 6 weeks).
plan for delivery in hospital or health centre where they are trained to carry out the procedure.
ensure counselling and informed consent prior to labour and delivery.
can be inserted immediately postpartum if no sign of infection (up to 48 hours, or delay 4 weeks)
plan for delivery in hospital or health centre where they are trained to insert the IUD.
Method options for the breastfeeding woman
C17. advise on routine and follow-up visits.
Encourage the woman to bring her partner or family member to at least 1 visit.
Routine antenatal care visits
- All pregnant women should have 4 routine antenatal visits.
- First antenatal contact should be as early in pregnancy as possible.
- During the last visit, inform the woman to return if she does not deliver within 2 weeks after the expected date of delivery.
- More frequent visits or different schedules may be required according to national malaria or HIV policies.
- If women is HIV-infected ensure a visit between 26-28 weeks.
Follow-up visits
C18. home delivery without a skilled attendant.
Reinforce the importance of delivery with a skilled birth attendant
Instruct mother and family on clean and safer delivery at home
If the woman has chosen to deliver at home without a skilled attendant, review these simple instructions with the woman and family members.
- Give them a disposable delivery kit and explain how to use it.
Tell her/them:
- To ensure a clean delivery surface for the birth.
- To ensure that the attendant should wash her hands with clean water and soap before/after touching mother/baby. She should also keep her nails clean.
- To, after birth, dry and place the baby on the mother's chest with skin-to-skin contact and wipe the baby's eyes using a clean cloth for each eye.
- To cover the mother and the baby.
- To use the ties and razor blade from the disposable delivery kit to tie and cut the cord.The cord is cut when it stops pulsating.
- To wipe baby clean but not bathe the baby until after 6 hours.
- To wait for the placenta to deliver on its own.
- To start breastfeeding when the baby shows signs of readiness, within the first hour after birth.
- To NOT leave the mother alone for the first 24 hours.
- To keep the mother and baby warm.To dress or wrap the baby, including the baby's head.
- To dispose of the placenta in a correct, safe and culturally appropriate manner (burn or bury).
- Advise her/them on danger signs for the mother and the baby and where to go.
Advise to avoid harmful practices
For example:
not to use local medications to hasten labour.
not to wait for waters to stop before going to health facility.
NOT to insert any substances into the vagina during labour or after delivery.
NOT to push on the abdomen during labour or delivery.
NOT to pull on the cord to deliver the placenta.
NOT to put ashes, cow dung or other substance on umbilical cord/stump.
Encourage helpful traditional practices:
If the mother or baby has any of these signs, she/they must go to the health centre immediately, day or night, WITHOUT waiting
- Waters break and not in labour after 6 hours.
- Labour pains/contractions continue for more than 12 hours.
- Heavy bleeding after delivery (pad/cloth soaked in less than 5 minutes).
- Bleeding increases.
- Placenta not expelled 1 hour after birth of the baby.
- Very small.
- Difficulty in breathing.
- Feels cold.
- Not able to feed.
All rights reserved. Publications of the World Health Organization are available on the WHO website ( www.who.int ) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: tni.ohw@sredrokoob ).
Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website ( www.who.int/about/licensing/copyright_form/en/index.html ).
- Cite this Page Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd edition. Geneva: World Health Organization; 2015. C, ANTENATAL CARE.
- PDF version of this title (2.6M)
In this Page
- ASSESS THE PREGNANT WOMAN: PREGNANCY STATUS, BIRTH AND EMERGENCY PLAN
- RESPOND TO OBSERVED SIGNS OR VOLUNTEERED PROBLEMS
- GIVE PREVENTIVE MEASURES
- ADVISE AND COUNSEL ON NUTRITION AND SELF-CARE AND SUBSTANCE ABUSE
- DEVELOP A BIRTH AND EMERGENCY PLAN
- ADVISE AND COUNSEL ON FAMILY PLANNING
- ADVISE ON ROUTINE AND FOLLOW-UP VISITS
- HOME DELIVERY WITHOUT A SKILLED ATTENDANT
Other titles in this collection
- WHO Guidelines Approved by the Guidelines Review Committee
Recent Activity
- ANTENATAL CARE - Pregnancy, Childbirth, Postpartum and Newborn Care ANTENATAL CARE - Pregnancy, Childbirth, Postpartum and Newborn Care
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
'I kept on saying goodbye': Gaza hospital reports rise in stillbirths and neonatal deaths
TEL AVIV — When Mai Kamal Zaqout learned she was pregnant in December, she and her husband, Ahmad, felt something they hadn’t experienced in many weeks in G aza : happiness — a glimmer of optimism amid the war’s devastation and despair.
Zaqout, 22, said Ahmad placed his hand on her belly and told her: “This is it. She is our last hope.”
But within months, that hope was shattered.
Ahmad, 29, was killed in an airstrike.
Then Zaqout fled south to Rafah, where more than a million people have sought refuge, in hopes of giving birth to her daughter in safety.
But Zaqout fell ill, weak from a lack of food and clean drinking water. Already grieving, she received another devastating blow seven months into her pregnancy: Her baby no longer had a heartbeat.
“I didn’t understand. I started crying and screaming,” she told an NBC News crew on the ground late last month. “All of the hospital gathered,” she said, asking, “‘What’s wrong with her? Why is she crying?’”
“I started saying, ‘Check again. Make sure,’” she said.
Her baby was stillborn in March.
Doctors in Gaza and humanitarian groups told NBC News that Zaqout is one of a growing number of women who have lost pregnancies or had complications, another dire consequence of the war.
“The doctors told me malnutrition had a big role in this,” Zaqout said. “I was not able to eat properly. I didn’t take vitamins. There was nothing available. … The water was polluted. I was feeling it.”

Zaqout said she visited the Emirati Hospital in Rafah during her pregnancy. Dr. Haider Abu Sneima, the hospital’s director, told NBC News last month that various factors were affecting maternal health there.
The little food that is available lacks “proteins, vitamins or vegetables, and if you find them, prices are out of the imaginary,” he said. "A pregnant woman or her family can’t obtain them."
On top of that, Abu Sneima added, the psychological pressures of the war have “a very negative effect on the mother and her baby.”
In recent weeks, he said, there appeared to be a rise in babies being born premature and generally “small in size.”
“We don’t see big children like we used to give birth to in the past. We don’t see these children anymore,” he said.
Dominic Allen, the designated representative for Palestinian territories with the United Nations Population Fund (UNFPA), said that when he visited Gaza last month, doctors at the Emirati Hospital similarly told him that they were no longer seeing “normal-sized” babies.
They reported “more complications around births caused, they’re telling us, by malnutrition and dehydration and from stress,” Allen said. “What they are seeing is an increased number of stillborn babies and neonatal deaths.”
NBC News could not independently verify those reported trends, and no data was available to confirm them. The Israel Defense Forces did not respond to a request for comment.
The World Health Organization has repeatedly said that malnourishment is rising in Gaza.
“Different doctors particularly in the maternity hospitals are reporting that they’re seeing a big rise in children born [with] low birth weight and just not surviving the neonatal period because they are born too small,” WHO spokeswoman Dr. Margaret Harris said Tuesday at a briefing .
The reports come amid mounting concerns about looming famine in Gaza. Already, Palestinian health authorities reported that at least 27 people, including children, have died from severe malnutrition in the enclave. Israel faces growing pressure from the international community to expedite the delivery of aid into Gaza, which it has been accused of restricting.
Israeli authorities have denied hindering the flow of aid into Gaza and have instead blamed humanitarian groups for the issue.
According to the UNFPA, around 155,000 pregnant women and new mothers in Gaza are “struggling to survive.”
“They are suffering from hunger and the diseases that stalk it, amid life-threatening shortages of food, water and medical care,” the agency wrote on its website .
“For the 5,500 women who will give birth in the coming month, accessing adequate health care is an unimaginable challenge. Only three maternity hospitals remain in the Gaza Strip, and they are overwhelmed with patients,” it said, adding: “Doctors and midwives — desperate for medicines and supplies — are struggling to provide adequate care to newborns.”
Dr. Angela Bianco, director of maternal fetal medicine and a professor of obstetrics, gynecology and reproductive science at the Icahn School of Medicine at Mount Sinai in New York, said she wasn’t surprised by the Rafah doctors’ reports, though limited data makes it difficult to draw conclusions.
“When you look at the world’s medical literature and you look at the impact of stress on pregnancy outcomes, there is data that definitely supports that there’s an increased rate of adverse pregnancy outcomes and specifically stillbirth and preterm birth in the face of maternal stress — specifically more so extreme stress.”
Zaqout said that after losing her husband, her baby girl was “my last hope.”
“For real. I was dreaming about her,” she said.
Zaqout’s husband is one of the more than 32,600 people killed in Gaza in the nearly six months since Israel launched its offensive after Hamas’ Oct. 7 attacks. Roughly 1,200 people were killed in Israel that day, and some 260 were taken hostage. At least 252 IDF soldiers have been killed since Israel’s ground offensive began.
Speaking with NBC News in Gaza on March 23, UNICEF’s global spokesperson, James Elder, said a cease-fire is necessary to address the spiraling humanitarian crisis in the enclave.
“People are exhausted, the coping mechanisms have been smashed,” he said. “The health system is teetering on collapse, and now we have imminent famine.”
Zaqout does not know exactly why her baby was stillborn, but she said she believes it was a consequence of Israel’s offensive in Gaza.
After the delivery, she said, “I kept on saying goodbye.”
“I told her, ‘Go to your father, a bird in paradise. I will wait for you and be patient, and we’ll back to what we were,’” she said. “We were a family on Earth. We will be in the afterlife.”
Chantal Da Silva is a breaking news editor for NBC News Digital based in London.

IMAGES
VIDEO
COMMENTS
Definition: The percentage of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times. Due to data limitations, it is not possible to determine the type of provider for each visit. Numerator: The number of women aged 15-49 with a live birth in a given time period that received antenatal care ...
recommended number of visits. Adequate prenatal care is care beginning in the first 4 months of pregnancy with at least 80%- 109% of the recommended number of visits. Adequate plus care is care beginning in the first 4 months of pregnancy with 110% or more of the recommended visits (8, 10). A prenatal care visit is defined as one in which the ...
The American College of Obstetricians and Gynecologists recommends antenatal visits every four weeks until 28 weeks' gestation, every two weeks until 36 weeks' gestation, and weekly thereafter ...
Like the WHO FANC model, the country guideline also suggests at least 4 scheduled ANC visits where the timely ANC visits refer to the 1st ANC visit within 16 weeks of pregnancy, the 2 nd ANC visit between 24-28 weeks, the 3rd ANC visit at 32 nd week, and the 4th ANC Visit at 36 th week of gestation .
Antenatal care (also termed prenatal care) is one of the most common preventive health services in the United States, accessed by about 4 million women annually.1 Antenatal care aims to improve the health and wellbeing of pregnant patients and their babies through (1) medical screening and treatment; (2) anticipatory guidance; and (3) psychosocial support.2, 3 The World Health Organization's ...
The ideal denominator for measuring the coverage of the early antenatal care visit is the number of pregnant women in a given time period, which also applies to other antenatal care indicators such as coverage of at least one antenatal care visit or at least four antenatal care visits. It is very difficult to calculate the number of pregnant ...
Factors Associated with Number of Antenatal Care Visits. About 10.7% of the number of antenatal care visits during pregnancy in clusters was explained in the full model. The Percent change variation in the final model showed that about 74.9% of the total variability in the number of antenatal care visits was explained (Table 3).
Definition: The percentage of women aged 15-49 with a live birth in a given time period that received antenatal care four or more times. Due to data limitations, it is not possible to determine the type of provider for each visit. Numerator: The number of women aged 15-49 with a live birth in a given time period that received antenatal care ...
Antenatal care coverage (at least four visits) is the percentage of women aged 15 to 49 with a live birth in a given time period that received antenatal care four or more times. Available survey data on this indicator usually do not specify the type of the provider; therefore, in general, receipt of care by any provider is measured.
Number of antenatal visits is grouped into categories of no antenatal visits, 1 visit, 2 visits, 3 visits, 4-7 visits, 8+ visits, and "don't know" before calculating percentages. ... "Don't know" or missing values on number of antenatal care visits and timing of first ANC are excluded from numerators but included in denominators. ...
Reduced visit versus traditional visit schedules for routine antenatal care ... In comparisons of fewer to standard number of scheduled antenatal visits, moderate strength evidence did not find differences for gestational age at birth (4 studies), being small for gestational age (3 studies), Apgar score (5 studies), or neonatal intensive care ...
Receiving quality antenatal care (ANC) from skilled providers is essential to ensure the critical health circumstances of a pregnant woman and her child. Thus, this study attempted to assess which risk factors are significantly associated with the timing of antenatal care and the number of items of antenatal care content received from skilled providers in recent pregnancies among mothers in ...
Moderate quality evidence from 2 RCTs (N=1520) showed that there is a clinically important difference favouring standard care versus a reduced number of appointments on the number of women who reported number of antenatal visits as 'not quite enough' or 'too few': RR 6.28 (95% CI 3.66 to 10.80). Very low quality evidence from 2 RCTs (N ...
Background Antenatal care is one of the best strategies for maternal and neonatal mortality reduction. There is a paucity of evidence on the mean number of ANC visits and associated factors in Sub-Saharan Africa (SSA). This study aimed to investigate the mean number of ANC visits and associated factors among reproductive-age women in Sub-Saharan Africa using the Demographic and Health Survey ...
Sustainable Development Goal (SDG) 3.7 aims to ensure universal access to sexual and reproductive healthcare services, where antenatal care (ANC) is a core component. This study aimed to examine the influence of health facility availability and readiness on the uptake of four or more ANC visits in Bangladesh. The 2017/18 Bangladesh Demographic and Health Survey data were linked with the 2017 ...
The antenatal period presents opportunities for reaching pregnant women with interventions that may be vital to both maternal, fetal and newborn health and well-being. WHO previously recommended that pregnant women complete at least four ANC visits. However, new guidelines from the WHO ANC Model (2018) increase the recommended number of ...
Introduction: Antenatal care (ANC) is a medical care and procedure carried out for pregnant women. Data on ANC visits can help policymakers show gaps in service provision. Therefore, this study assessed the factors associated with the number of ANC visits among women in rural Ethiopia.
9 months. 36-38 weeks. All pregnant women should have 4 routine antenatal visits. First antenatal contact should be as early in pregnancy as possible. During the last visit, inform the woman to return if she does not deliver within 2 weeks after the expected date of delivery.
Zaqout's husband is one of the more than 32,600 people killed in Gaza in the nearly six months since Israel launched its offensive after Hamas' Oct. 7 attacks. Roughly 1,200 people were killed ...