- About Founder
- News & Press
- See Our Reviews
- HONcode Certification
- HIPAA Compliance & Security
- Editorial Guidelines
- Sponsor Program
- Privacy Policy
- Terms & Conditions
- Adam's Book
- Hats & Fun Stuff
- About Community
- Patient News Feed
- Success Stories
- Adam's Blog

LEARNING CENTER
- Heart Valve News Feed
- Atrial Fibrillation
- Free Educational eBooks
- Medtronic Low-Risk TAVR
SURGEON FINDER
- Featured Surgeon
- Recommend Surgeon
HEART HOSPITALS
Adam's blog.
- About Adam Pick
Traveling Timeline After Heart Surgery
By Adam Pick on November 25, 2013
Travel during the holiday season is expected to increase this year, up from the 93.3 million travelers who ventured at least 50 miles away from home this time last year, according to AAA. Although many medical professionals recommend avoiding traveling during recovery, it seems practically unavoidable during this family-centered season. However, just because you might be going against this advice, it doesn’t mean you should throw all caution to the wind. These tips break down some important considerations for traveling after heart surgery.
The National Health Service recommends checking with your airline BEFORE flying, since companies have varying regulations on post-surgery travelers. However, the Civilian Aviation Authority says that 10 to 14 days is sufficient after chest surgery or a coronary artery bypass graft. After any heart operation, patients should remain moderately active to keep the heart pumping. Avoid tight clothing to prevent circulation inhibition as well.
During your early recovery, you’ll want to maintain only moderate activity at your destination. If your destination is the Midwest, consider staying at Wisconsin Dells resorts to take advantage of spas and other relaxation-enhancing amenities. In warmer weather conditions, swimming can also be a fun, light activity to stay active and cool.
Three months
At this point, you may be close to a full recovery but not quite there yet. (Hopefully, you will have taken my advice and attended a great cardiac rehab program.) Mostly, you’ll want to make sure to avoid overworking your heart. Get a full examination — BEFORE your trip — so your doctor can alert you of specific things to look out for. Taking medication like Dramamine isn’t recommended for flying, since you may sleep in a circulation-cutting position for an extended period of time. If you get nervous on airplanes or other forms of transportation, consider anti-anxiety medication instead, so you can keep your heart rate low without compromising your circulation.
Since being active can be difficult in an airplane, request to sit either in the very front or very back of the plane, so you can stretch your legs as often as possible. In the meantime, drink plenty of water, since the low humidity on planes increases the risk of dehydration.
Traveling itself may only come with minor considerations at this stage, such as staying hydrated and active. However, you’ll want to keep a close eye on your diet once you reach your destination. Especially during the holiday season, many people indulge in sugar-filled, high-fat foods. The American Heart Association recommends having less than 7 percent of saturated fat out of your total daily calories. Trans fats should comprise less than 1 percent of your daily intake, while cholesterol should never exceed 300 mg. The best way to reduce your saturated and trans fats intake is to reduce the amount of butter or margarine added to your food when cooking. Trim fat off of your meat or choose lean meats with under 10 percent fat to further cut back.
Right about this time… I traveled to Hawaii with Robyn, my wife, to celebrate my recovery. It was an amazing trip (see picture below).

At 10 months post-op, I went on a two-week business trip through five cities in Europe. During the trip, I had some chest pain — from the lifting and the moving of luggage in awkward positions — so I carried a bottle of Ibuprofen with me at all times to help ease the discomfort.
At the one year mark, many patients have reached full recovery status. Still, it’s always important to continue taking precautions when traveling. Make sure your travel insurance is up to date, since recent surgeries can often raise rates or lead to a higher copay. Access to medical care is highly important when you’re away from home, so feel free to check in with a doctor if anything feels abnormal.
I hope this timeline helps you plan your travel after heart surgery.
Keep on tickin! Adam
- Leave a Comment
- See 12 Comments
Written by Adam Pick - Patient & Website Founder

Adam Pick is a heart valve patient and author of The Patient's Guide To Heart Valve Surgery. In 2006, Adam founded HeartValveSurgery.com to educate and empower patients. This award-winning website has helped over 10 million people fight heart valve disease. Adam has been featured by the American Heart Association and Medical News Today.
12 Comments ... Click here to add one .
Name (required)
E-Mail Address (will not be published) (required)
Submit Comment
Adam's Newest Blogs
Adam's newest posts.

Join 400 Patients on Thursday’s Patient Webinar!

“Is Corkscrew Espophagus A Complication During Heart Valve Surgery?” asks Lori
New Community Posts

Susan says, "Saw this trending, today. https://..."

Suzette says, "Today // while working I get call from..."
Blog Categories
Adam's blog categories.
- Adam's Updates
- Aortic Stenosis
- Aortic Valve Repair
- Aortic Valve Replacement
- Before Surgery
- Bicuspid Aortic Valve
- Heart Valve Replacement
- Medical Technology
- Mitral Regurgitation
- Mitral Valve Repair
- Patient Stories
- Ross Procedure
- Surgeons & Hospitals
- Tricuspid Valve
Surgeon Finder

Find and research over 1,500 patient-recommended heart valve surgeons.
Surgeon Spotlight
Dr. Vinay Badhwar is a heart valve expert having performed thousands of heart valve repair and replacement operations during his career.
See Patient Reviews
New Posts From Our Community
Newest community post.
Susan Lynn from Wilkes Barre says
Saw this trending, today. https://www.pbs.org/newshour/amp/show/
Susan says, "Saw this trending, today. https://" Susan's Journal

Suzette Schear from Holbrook, Long Island says
Today // while working I get call from doctor with instructions
Meet Suzette
Suzette says, "Today // while working I get call from" Suzette's Journal

Richard Munson from Massachusetts says
Wear a tracking device before surgery
Meet Richard
Richard says, "Wear a tracking device before surgery" Richard's Journal

Find Heart Valve Surgeons
Search 1,500 patient-recommended surgeons
The Patient's Guide
This book has helped over 47,000 patients and caregivers from diagnosis to recovery.
Heart Valve Hospitals

Search Heart Hospitals Search Hospitals
Can You Fly After Open Heart Surgery?

Open heart surgery can be minimally invasive or require a long period of recovery. In any case, you or your loved one will likely be in a more delicate state. This means your normal routine, including work, exercise, activities and travel, may not be feasible for several weeks or more. If you have a trip planned in the near future or had your surgery done in another state, traveling by plane can potentially create health complications.
Flying on a commercial airplane is not always recommended for recovering patients, especially those with conditions like diabetes. If you want to know whether it is safe to travel after heart surgery, consider the potential risks of traveling and alternative modes of long-distance patient transportation that are available.
What Is Open Heart Surgery?
Open heart surgery is an umbrella term people use to describe surgical procedures that treat heart problems. This type of surgery typically involves the heart muscle, arteries, valves, aorta and coronary arteries. Open heart surgery gets its name from the nature of the procedure itself, which often requires surgeons to cut through an individual’s breastbone and spread their ribs to perform surgery on their heart. Typically, individuals with heart problems who do not see improvements with medications, lifestyle changes or other procedures may require open heart surgery.
With open heart surgery, surgeons can access the heart to treat the following conditions :
- Coronary artery disease
- Heart valve disease
- Heart failure
- Thoracic aortic aneurysm
- Congenital heart defects, such as hypoplastic left heart syndrome or arterial septal defect
- Arrhythmias
- Atrial fibrillation
- Coronary artery bypass graft (CABG)
In some cases, an individual’s heart will be stopped during open heart surgery. If so, they are connected to a bypass pump, or heart-lung bypass machine, during the procedure. This machine acts as the heart and lungs during the surgery, moving blood through the body and providing oxygen to the blood.
However, patients who require less invasive surgery with smaller incisions may have the procedure performed while their heart is still beating. This form of surgery requires smaller cuts between the ribs. Some patients may undergo open heart surgery to repair issues from a heart attack, for a heart transplant or for valve replacement. The type of surgery a heart patient has depends on their unique condition or combination of problems.
Complications and Restrictions After Open Heart Surgery
Having a major medical procedure like open heart surgery comes with the potential for complications. It’s important to know that you may be limited or restricted in what you can do as you recover.
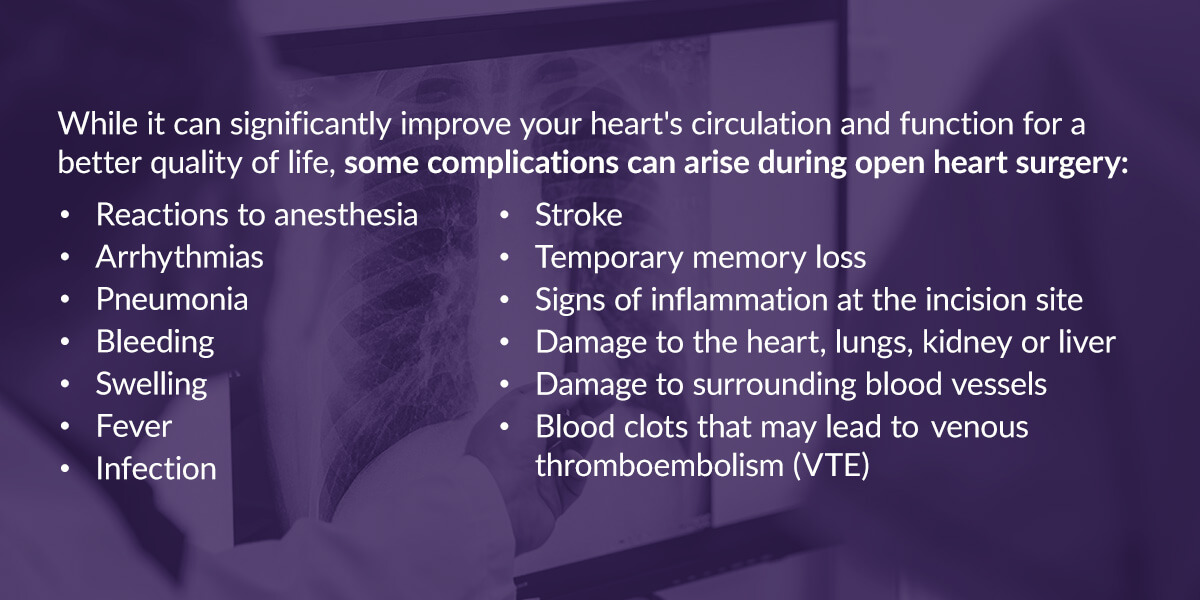
- Reactions to anesthesia
- Temporary memory loss
- Signs of inflammation at the incision site
- Damage to the heart, lungs, kidney or liver
- Damage to surrounding blood vessels
- Blood clots that may lead to venous thromboembolism (VTE)
The severity of these risks also depends on the type of heart condition you have and your overall health.
Second, your lifestyle may change during recovery. Depending on the type of surgery you had, you may need to take medication, attend physical therapy, and get plenty of rest as your chest muscles and breastbone heal. This means your typical activities may need to be postponed until you are well enough.
Third, your travel abilities may be limited for several weeks or more. The complications of heart surgery noted above may become a greater risk if you engage in activities that are too strenuous during recovery, such as intense exercise or flying. If you plan on traveling, some airlines may require you to receive a medical clearance certificate from your doctor. This certificate shows that your health care providers “clear” you to participate in certain activities, including flying across long distances.
Your physician or surgeon will assess you via a thorough examination to determine if your condition could worsen by sitting on a plane for several hours. If you have plans to travel after your surgery, it’s important to talk to your doctors about whether you will require medical clearance.
Risks of Flying Too Soon After Open Heart Surgery
Can you fly after heart surgery? Depending on your condition and recovery time, yes. However, being on an airplane for long periods after an invasive surgery can present issues that may have a negative impact on your cardiovascular health, even if you feel OK after surgery. Commercial air travel can be risky for these reasons:

- High altitude: Flying in an airplane may have the same effect on your heart as visiting high-altitude locations. Patients who have certain heart conditions or high blood pressure may be more at risk for complications . Drastic changes in altitude can potentially worsen symptoms of existing heart conditions or lead to other heart events. Being at higher altitudes can put more strain on the heart.
- Low oxygen concentration: Airplanes, which travel at higher altitudes, also have reduced oxygen pressure. Sitting in the airplane cabin for hours means your body may not receive the optimal amount of oxygen, which can pose a risk for those with existing heart conditions like heart disease, CAD and pulmonary hypertension. Because there is less oxygen getting to your lungs on an airplane, your heart has to work even harder to pump blood to the rest of your body.
- Stress or anxiety: It’s common for people to feel general anxiety or stress about flying due to fear of heights or turbulence. Stress or anxiety can make your heart conditions worse or lead to a high heart rate, which may also prolong your recovery process.
- Changes in pressure: Passengers will feel pressure changes as the aircraft cabin altitude increases or decreases. This can cause gas to increase or expand in the body, resulting in pulmonary barotrauma . You may experience chest pain, a bloody nose or shortness or breath, which can lead to serious lung and heart damage if you’re recovering from open heart surgery.
- Dehydration: On long-haul flights, significant changes in fluid balance can occur due to controlled, dry air. Very low humidity can generally lead to faster dehydration, affecting your blood pressure. This can be problematic for those with heart disease, CAD, arrhythmia or heart failure.
- DVT risk: Sitting in a cramped plane cabin requires long periods of immobility and poor circulation. Combined with potential dehydration, you may be at a higher risk of developing a blood clot , which often forms in veins in the legs. This is also known as deep vein thrombosis (DVT). If you have an implanted heart device, artificial heart valve, arrhythmia, CAD or a coronary stent, your risk may be even greater. Blood clots can lead to a stroke or heart attack.
When flying after cardiac surgery, you may experience several of these risks at once, which could worsen the negative effects on your overall health.
Patients Who Are at Higher Risk
Your risk of complications, such as DVT, when flying after heart surgery may be greater if you have certain preexisting conditions like the following:
- Chronic obstructive pulmonary disease (COPD)
- Kidney disease
- Blocked arteries in the legs
- Heart or lung disease
- History of blood clots
- History of DVT
- Being on extended bed rest
- Having a catheter in a large vein
- Recent or current cancer treatment
- Having limited mobility
- Varicose veins
- Use of hormones, such as oral contraceptives or hormone replacement therapy
While some blood clots can dissolve on their own, and travel-related DVT is generally low , some clots can travel to your lungs. This may result in a blockage of blood flow and potentially lead to a pulmonary embolism, which can be fatal.
Your chances of these complications can also depend on your age. For example, older individuals may have a higher risk of developing blood clots than younger patients. People who smoke may also be more likely to experience post-surgical issues. The risks of experiencing complications during open heart surgery may be higher if the procedure is performed during an emergency.
You may receive medication to control your blood pressure or prevent bleeding and infection when flying after open heart surgery. This can reduce your risk of complications.
How Long Do You Have to Wait to Fly After Open Heart Surgery?
How soon after open heart surgery you can fly depends on your doctor’s recommendation about your overall condition and other factors. For example, if you’ve had a minimally invasive cardiac surgery with no complications, you may be able to fly within two to four weeks. For more moderate or intense open heart surgery, such as heart bypass surgery, you may need to wait four to six weeks .
If you had open heart surgery for a serious complication or other conditions that could potentially make certain activities during recovery more risky, you may have to wait six to eight weeks or longer. Every individual is different, but you should expect a minimum of two weeks before you can safely travel long distances. How long you have to wait to fly after open heart surgery also depends on how much you have healed and whether you have conditions that could put more strain on your heart and lungs while flying.
Tips for Traveling on an Air Flight After Cardiac Surgery
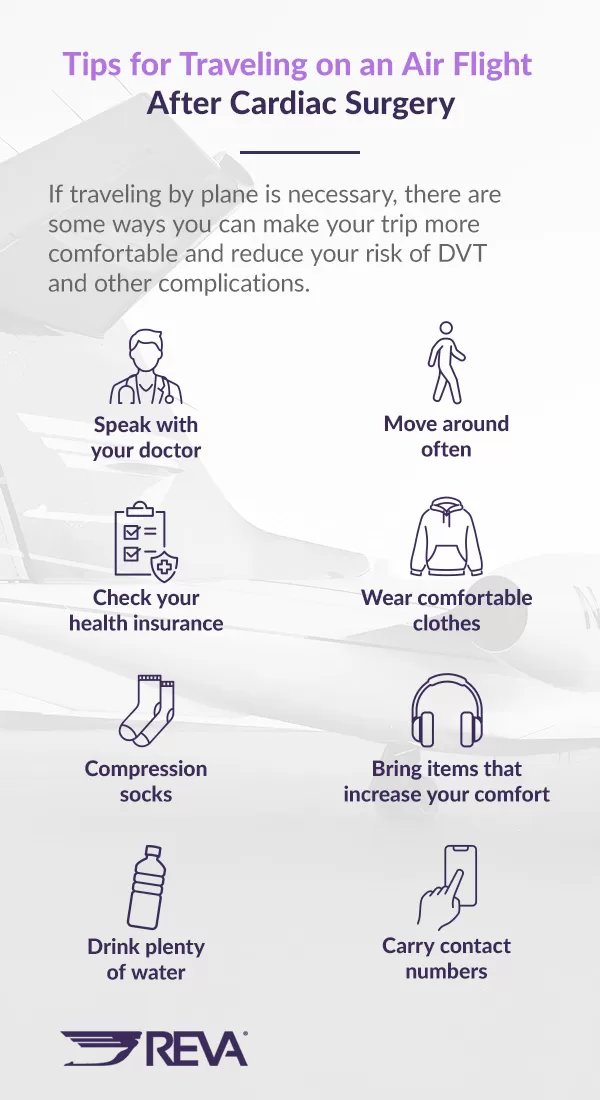
If traveling by plane is necessary, there are some ways you can make your trip more comfortable and reduce your risk of DVT and other complications.
- Speak with your doctor: Check that your prescriptions are up to date and that you have enough for your travels. Ask your doctor whether they can provide a letter describing your condition and any medications you currently take, including dosages. Your doctor will likely provide other essential information you need for your flight.
- Check your health insurance: Determine whether you are covered for travel. Some travel insurance policies may cover preexisting conditions like heart disease, but you may have to pay a higher premium. Contact your insurance broker to ensure you have health insurance coverage.
- Bring compression socks: Compression stockings, or high socks that reach just under the knee, can help you avoid blood clots in the legs during prolonged periods of sitting. Compression socks help improve blood circulation and lymphatic drainage in your legs, decrease swelling, and prevent low blood pressure when you stand up after several hours of sitting down.
- Drink plenty of water: Staying hydrated is essential no matter where you are, but it’s especially important during recovery and on a long flight. Because you’re likely to be more dehydrated on an airplane with dry air, be sure to drink plenty of water. Try to avoid coffee, soda, tea and alcohol, as these can dehydrate you more and may interact negatively with your medication.
- Move around often: Though you may not have tons of legroom, try to at least move your legs and feet for a couple of minutes each hour if you’re seated. If possible, walk up and down the aisles or go to the restroom to stretch your legs. Gentle stretching before your flight can also help with improving blood flow.
- Wear comfortable clothes: Wearing breathable, stretchy clothing can make for a better travel experience in general. Women can wear comfortable bras that are not underwired, especially while their breastbone is healing. Wearing tight clothing, like jeans, may restrict your movements on the plane.
- Bring items that increase your comfort: When traveling after heart surgery, you want to have everything you need for a worry-free flight. If you have anxiety about flying, bring headphones, a book or anything that will help make the time go by faster. You may consider getting a breathing pillow for strengthening the diaphragm and supporting optimal diaphragmatic breathing throughout the flight.
- Carry contact numbers: Whether you’re flying with someone else or alone, be sure to have the contact information of a local doctor, surgeon or specialist who knows about your condition and can assist airline employees and medical staff in the event of a complication.
What Are My Options for Flying Before or After Open Heart Surgery?
If you have a severe heart condition and need to travel for surgery or treatment immediately, flying may be your only option. While this is the quickest method, you will need to consider how to safely arrive at your destination before and after your surgery.
If you’re flying on a public commercial flight, you might consider flying with a medical escort . These trained and qualified professionals — who are also called flight nurses or patient escorts — will travel with you to ensure air travel safety. They will also provide any necessary medical care throughout your trip.

Having a medical escort with you can help you feel reassured that you’re doing what you can to mitigate any risks related to your heart condition. Whether you’re traveling short or long distances, a medical escort providing constant medical supervision can bring you peace of mind during emergency or non-emergency situations .
Another alternative is using a mode of private medical transport, like an air ambulance. If your condition is more severe, the risk of you experiencing worsening symptoms or a life-threatening emergency may be greater when flying on a commercial air flight alone. Because commercial flights are not equipped with knowledgeable medical personnel or life-saving equipment, flying in an air ambulance can be a safer way to travel. Private medical transport services can take you safely from bedside to bedside.
Whether you’re traveling to your surgeon or going home post-op, an experienced medical crew will be on board to mitigate health risks and provide medical attention if needed. In an air ambulance, the medical crew can even adjust the cabin pressure to avoid complications. Air ambulances are self-contained critical care units that can keep you comfortable and meet your needs.
Domestic Air Ambulance
International air ambulance, how air ambulances can help.
Air ambulances have the technology and medical devices to safely transport you from point A to point B. If you have a heart condition that requires care along the way, an air ambulance can make your experience more comfortable than a private aircraft.
While traveling with a medical escort on a commercial flight can be a suitable option, those who have more severe conditions or prefer to travel with more reassurance and security may find an air ambulance more ideal. You might also need an air ambulance if you:
- Need transportation to a specialized medical facility that is far away.
- Do not have access to public transportation where you reside.
- Are unable to drive yourself or fly unaccompanied due to your heart condition.
- Are flying with a commercial airline that has restrictions on the type of medication or oxygen container you have.

There are a few types of air ambulances that offer different benefits. A helicopter ambulance is suitable for landing near health care facilities or in remote locations and addressing immediate response situations. Fixed-wing ambulances are larger, faster and more suitable for long-distance travel.
Both types of air ambulances come equipped with specialized medical equipment and supplies, much like you would find in an intensive care unit (ICU). Some of this equipment includes:
- Monitoring devices.
- Life support systems.
- A wide range of medications.
You will also find paramedics, doctors and nurses on board your air ambulance who are prepared to handle critical care situations. If it seems like you or a loved one could benefit from safe, tranquil travel on a private air ambulance, know that providing potentially life-saving care is not the only advantage. Here are some other key benefits of using an air ambulance:

- Time-sensitive transportation: In a life-threatening situation, patients need a rapid response. Air ambulances can get medical teams to the individual for quick transport to a specialized facility that they may not receive in a local hospital. A fast response time with a fully equipped aircraft can improve patient outcomes and the chances of survival and recovery.
- Compassionate care: Medical personnel on air ambulances are highly trained and skilled, but they are also dedicated to helping patients before, during and after transport. Loved ones can also be notified of the patient’s health with updates from multi-lingual specialists for clear and consistent communication.
- Quality aircraft: Air ambulances maintain high safety standards, as they are specifically designed to provide medical care for a wide range of injuries and illnesses. Patients will have access to a comfortable and safe environment with high-quality equipment.
- Efficient accessibility: Whether a patient needs to be moved from a mountain to a medical facility or brought back home safely from a foreign country, air ambulances have the capability to quickly transport patients over long distances and access locations that may be too difficult for ground transportation.
Contact REVA for Smooth, Comfortable Medical Transportation
If you need to travel by plane before or after open heart surgery, know that you have options. REVA offers air ambulance and medical escort services that transport you to your destination to mitigate risk. Our experienced, compassionate professionals can get you where you need to be while enhancing your safety and comfort. From critical in-flight medical care to private ground transportation, it’s our goal to help you or your loved one prevent worsening conditions after major surgery.
Traveling with REVA means you can benefit from all the benefits of a private jet along with the latest medical equipment to give you the care you need while flying. At REVA, we offer both domestic and international air ambulance flights , where our friendly medical crew is ready to help you travel to and from treatment. Contact us today to request a free quote for our air ambulance or medical escort services.


Heart Sisters
For women living with heart disease
How soon are heart patients safely fit to fly?

by Carolyn Thomas ♥ @HeartSisters
Five months after my heart attack, I boarded a plane from the West Coast bound for Rochester, Minnesota. Considering that I’d suffered two terrifying cardiac events on another long flight just five months earlier made this trip just a wee bit scary for me.
Only the reality that I was headed to the world-famous Mayo Clinic helped to propel me onboard. I told myself that if anything happened to me and my heart during this flight, the board-certified cardiologists at the Mayo Women’s Heart Clinic would know exactly what to do for me. If I survived the flight, that is . . . . .
Like many freshly-diagnosed heart attack survivors, my fear of having a heart attack on a plane was very strong. (Note: many survivors experience a very strong fear of having another heart attack just walking down the street).
So being strapped into a metal box 35,000 feet up in the sky, hour after endless hour, inhaling stale air, in a pressurized germ-infested environment, with reduced circulating oxygen levels in my blood, risking the onset of hypobaric hypoxia , and with no guarantee at all that my seatmate would be a board-certified cardiologist seemed just plain crazy.
But apparently there is good news about heart patients and flying from the British Cardiovascular Society.
Most people with heart disease who are not critically ill can safely fly on commercial aircraft, according to a U.K. report. (1) Lead author Dr. David Smith (Royal Devon and Exeter NHS Foundation Trust) told H eartwire:
” The overwhelming conclusion is that the cabin environment poses very little threat. It’s not the flying that’s the problem for heart patients, but the stability or instability of someone’s underlying condition that indicates the probability of a spontaneous cardiac event occurring while they are in the air.”
The passengers who might feel some minor physical effects of low blood oxygen (hypoxia) include those already at risk of:
- myocardial infarction (heart attack)
- heart failure
- abnormal heart rhythms
But according to Dr. Smith, the blood oxygen levels induced by flying “ appear to have little or no adverse circulatory effects, certainly not for short- and medium-haul flights.”
However, some heart patients at high risk are advised to “ defer travel ” until their condition is stable, including those:
- having an ejection fraction <40%
- showing signs and symptoms of poorly controlled heart failure
- with unstable angina or uncontrolled arrhythmias
- awaiting further investigation, revascularization, or device therapy
And here’s how soon after a cardiac procedure you are generally safe to fly:
- After uncompl icated elective (non-emergency) cardiac catheterization (angioplasty, wi th or without stent implants), patients can fly after a few days.
- If patients suffer from stable angina with infrequent attacks, they should be able to fly. It is safe to use nitroglycerin spray in a pressurized aircraft cabin.
- Patients with pacemakers implanted can fly after a few days, unless they have suffered a pneumothorax , in which case they should wait until two weeks after it has fully healed.
- Those with ICD s (Implantable Cardioverter Defibrillators) can fly after a few days, with the added recommendation that they should not fly after the ICD has delivered a shock until the condition is considered stable again.
- Those who have experienced a heart attack (myocardial infarction) can fly after 10-14 days. If you are older than 65 or if you’ve had another heart attack in the past, you’re statistically more likely to have one again. The U.K. Civil Aviation Authority recommends that i f you have no symptoms or other heart conditions and no further cardiac treatment is planned, you’re considered to be at low-medium risk to fly. But if further cardiac treatment is planned, you’re considered to be at higher risk of another heart attack – best not to fly at this time.
- Those who have had heart valve repair or replacement surgery or coronary artery bypass grafts ( open heart surgery ) can usually fly after 4-6 weeks (longer if they have had pulmonary complications).
Generally speaking, if you can walk briskly for 100 metres on the flat without being breathless or in pain, you can fly.
But even when your physician has officially given you the green light to fly again, remember that severe fatigue can continue to be a serious issue for heart patients long after the other physical effects of cardiac procedures have healed.
Anticipating this fatigue may influence your decision, for example, to request an airport wheelchair or a ride to connecting gates on the airline golf cart, and to limit the weight and size of your carry-on bag. Please plan ahead and arrive at the airport significantly early for any flight to minimize rushing or stress.
The anxiety surrounding air travel can be debilitating even for non-heart patients. If fear of flying has ever been a serious issue even before your own cardiac event, it may indeed feel worse now. If you really must fly, ask your own doctor about managing this anxiety before your flight.
Long flights can mean crossing time zones, sleep deprivation and jet lag. Probably the most important effect of changes in sleep patterns for passengers with cardiovascular disease is the potential disruption in taking daily medications. It can be difficult to stick to a normal meds routine when that routine is altered, especially if we’re confused about what time it really is. The U.K. report warns that it’s especially important for passengers with stable heart failure, angina or arrhythmia to maintain the regularity of their medications.
If you’re planning an out-of-country flight in the near future, remember that most major insurance companies will not provide travel medical insurance earlier than 90 days after a cardiac event, or even after a change in your medical treatment. In some cases, just a doctor’s appointment in the past 90 days at which your medication dosage is changed (either increased OR decreased) can mean your condition can be considered “unstable” and thus grounds for denial when you file a travel medical insurance claim.
Each airline has its own policy for allowing flying passengers after a cardiac event – and as you’ll see from the Oregon heart patient’s experience with Alaska Airlines (described below), some of these policies appear to defy accepted medical guidelines. So call both your insurance broker and the airline before you book a flight to double-check all details relevant to your own travel and clinical circumstances.
For heart patients who sport implanted medical devices, it may be comforting to know that the amount of metal used in most implanted heart devices like pacemakers, heart valves or ICDs is very small, according to cardiologists at St. Jude Medical. It is usually not enough to set off airport security metal detectors ; if it does, simply show security personnel your patient identification card. Passing through a metal detector should not hurt your device. However, do not linger near the security system arches or poles.
Dr. Clemens Jilek and his team of researchers from the German Heart Center in Munich recently did a study on 388 heart patients, published in the journal Annals of Internal Medicine . They concluded that metal detector security screening appears safe for those with pacemakers or ICDs implanted.
What about those new full body scans at airport security gates and people with implanted pacemakers or ICDs? According to cardiologist Dr. Richard Fogoros , there are few if any controlled clinical studies or even written information about the safety of these full body scanners for heart patients:
“I called the technical support departments of two major pacemaker manufacturers. I was told that they regard the full body scanner as completely safe for those with implanted pacemakers and ICDs, and this is what they tell patients and doctors when they call for advice (which apparently they do frequently, since there is no written advice anywhere). I was told that:
- 1) their engineers have determined it is extraordinarily unlikely that these scanners are capable of negatively affecting implantable medical devices
- 2) many thousands of people with pacemakers and ICDs have used total body scanners over the past several years, and there has been no allegation of any problems.
“So, both engineering theory and a large volume of real-world experience indicates they are safe, according to them.
“There is no reason to believe that a full body scanner will effect a pacemaker or ICD, and medical device companies are willing to say that verbally (but not in writing).
“If you want to wait until some authority is willing to make a definitive written statement about this, you can opt for a pat-down instead when you go through airport security. Since this issue is in the hands of bureaucrats, however, don’t hold your breath waiting for a resolution.”
A serious health problem you may have also heard linked with air travel, particularly long flights, is deep vein thrombosis (DVT) and venous thromboembolism .
Although a long-haul flight doubles the risk of DVT, it is actually similar to that incurred during car, bus, or train travel for a similar period, the U.K. researchers state. And the absolute risk of DVT for a fit and healthy person is one in 6,000 for a flight of more than four hours, they note, pointing out that pilots are at no greater risk than the general population, a statistic that is not particularly comforting.
Now I have to worry not only about myself, but about my pilots. Why not take the advice of my heart sister Jaynie, who always harps at us to wear compression knee-high stockings while flying?
There are some recommended common sense flight precautions for those at risk of DVT:
- consume plenty of fluids
- exclude caffeine and alcohol
- wear compression stockings
- take a dose of low-molecular-weight heparin (a blood thinner)
- wear a MedicAlert bracelet or dogtag necklace at all times
- talk to your doctor to confirm that your cardiac disease is stable
- carry adequate supplies of all prescribed medicine
- carry a copy of your medical history
- carry emergency phone numbers for your doctor(s), family members and destination contacts
Having memorized these precautions, you might want to also consider the alarming case of one Oregon heart patient who describes her “very interesting flight” to Rochester, Minnesota to see cardiologist Dr. Sharonne Hayes at the Mayo Women’s Heart Clinic. Here is the transcript of her complaint against Alaska Airlines filed with the FAA:
“I mentioned to the E/C flight attendant that I carry nitroglycerin for chest pain in my pocket should I request assistance, and that it was only cautionary in nature because I was traveling alone. “The Head Flight Attendant ordered me off the flight because she ‘assumed’ that I was unhealthy. She required me to provide a doctors’ note clearing me to fly. She informed me that the FAA allows flight crew to decide who is fit to fly or not, and they can remove whomever they feel is unfit to fly. “Alaska Airlines customer services representative and flight attendant refused to speak with my cardiologist who was wakened at 6:30 a.m. on a Sunday morning because I did not have the “requested” doctor’s note. “I explained that the flight crew had no data to support their assumption that I was unfit to fly, nor did they request the other passengers to produce doctors’ notes. “Alaska Airlines discriminated against me based on the fact that I carry nitro in my pocket. They created a very stressful environment and threatened to impair my ability to seek medical care at the Mayo Clinic. They humiliated me in front of a plane full of passengers. “An air carrier may not discriminate against an otherwise qualified individual on the following grounds: 1) the individual has a physical or mental impairment that substantially limits one or more major life activities. 2) the individual has a record of such an impairment. 3) the individual is regarded as having such an impairment.”
(1) Smith D, Toff W, Joy M, et al. “ Fitness to fly for passengers with cardiovascular disease. The report of a working group of the British Cardiovascular Society “ . H eart 2010
COVID-19 UPDATE 2020: “ S hould I avoid plane travel just to be safe?”
“ Planes tend to be low humidity, but the air’s actually pretty clean. It gets re-circulated through these HEPA [high-efficiency particulate air] filters that really are very good at clearing stuff out,” said Dr. Vicki Hertzberg , a biostatistician at Emory University, who co-led a study on flights and disease transmission with scientists at Boeing. “Also, they suck in about 50% clean air with every re-circulation. So in some aspects, the air on a plane is cleaner than what’s going on in your new office buildings.”
Remember that Dr. Hertzberg’s advice applies only to passengers while the plane is in the air. As soon as that aircraft lands, passengers exit the plane and are no longer protected by HEPA filters while walking through the airport, or waiting at the baggage carousel, or shopping or dining in the airport, or getting onto airport transportation vehicles.
NOTE FROM CAROLYN: I wrote more about my fateful five-hour flight in Chapter One of my book, A Woman’s Guide to Living with Heart Disease . You can ask for it at your local library or favourite bookshop, or order it online (paperback, hardcover or e-book) at Amazon , or order it directly from my publisher, Johns Hopkins University Press (use the code HTWN to save 30% off the list price).
Like this? Share it with others!
- Click to email a link to a friend (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to print (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Mastodon (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Tumblr (Opens in new window)
Published by Carolyn Thomas
View all posts by Carolyn Thomas
21 thoughts on “ How soon are heart patients safely fit to fly? ”
Very interesting . I have recently travelled from Houston to Perth. I had 2 heart stents inserted 3 weeks prior to my journey home. I have been home for 5 days now. I’m experiencing shortness of breath and nausea if I do too much.
I’m wondering if the jet lag and fatigue is the cause. I can’t do a lot as I become so exhausted.
Hello Kathleen – I’m sorry you’re experiencing these puzzling new symptoms. I’m not a physician so cannot comment specifically on your situation, but I can tell you generally that you’re still in relatively early days, post-stents. And as this post mentions, “severe fatigue can continue to be an issue for heart patients long after the other physical effects of cardiac procedures have healed.” It’s quite possible that the effects of jet lag and the travel itself are adding to that fatigue. If I were in your shoes, I’d contact my doctor just to check this out – especially if symptoms seem to be worsening instead of gradually improving.
Meanwhile, you could start a Symptom Journal ( more details here ) to track which specific activities seem to aggravate those symptoms. It’s important that recently diagnosed heart patients remain as physically active as possible – so you don’t want to stop moving or start dreading “doing too much” out of a fear of possible after-effects, but you also don’t want to be suffering!
Good luck to you! ♥
Hi Carolyn, I just some how have fallen outside of of the safety zones for flying. I was told from the point of my AMI that my heart was to weak to withstand G-force meaning flying will forever be out of range. Since then I’ve developed Supraventricular tachycardia (SVT-fast or irregular heartbeat) with episodes of SCD that won me an A-ICD (implanted defibrillator). The worse part of all is I don’t feel my SVTs, and my SCD has me going down in slow motion. I’m not allowed to move to far from where I am.
Lastly I have a stent and an A-ICD, I have set off security alarms and it does hurt. They say that we shouldn’t but my stent has set of the alarm. We were given color coded cards to carry with us when the devices were implanted. My stent is at the top of the list. In the 12 years since my AMI I’ve two long road trips. Both were 12 hour bus trips to New York. The first with the cardiac therapist and staff at the heart hospital, super safe trip. The second was with family for a weekend trip, they had to stop every three hours to slow swelling of feet and legs. Robin
This was so interesting to learn about my condìtion. And I will use the knowledge to teach others.
I am with CABG 2 months ago, I have breathing problem, can I traveling by air?
Hello Majid, only your cardiologist can answer you. The U.K. report suggests 6 weeks minimum before CABG patients fly, but longer if you have pulmonary problems. Ask your doctor – and good luck to you.
The NHS choices website also gives information apparently after discussion with the CAA. This suggests that you can safely fly 10 days after chest surgery or CABG. Clearly there is enormous variation in the advice given by different bodies.
With breathing complications like Majid describes, that 10-day suggestion may not be appropriate, which is why the best answer is to consult with her own physician.
Very comprehensive article. Thanks for this useful list of flying-related tips and facts. Now if you could just help us make the airlines run on time to get rid of those long delays . . .
Yeah, I’ll get right on that . . . 😉
Hi, I enjoyed this post. As a person who has congenital heart disease I have often faced “complications” at airports, with one particular gentleman asking what the “HUGE” scar was.. Well how rude.
I am from England and I have had lots of operations, ablations, implants, etc. But travelled a lot as I do not let it get in the way. I just would like to say that I have always brought insurance to cover myself (and family), especially for my heart, and although it costs a lot sometimes, it’s worth every penny.
Do not let it stop you travelling but always listen to your doctor too, if they say no, then go with that; save your money and go another time (she says through grumbled teeth, wanting to see her friends in America).
Great article.
That IS rude! (what’s the huge scar from? Preferred answer: How about “None of your frickety-frackin’ business!” ?!?) Travel insurance is such an important issue for heart patients as some policies will NOT cover pre-existing conditions or even incidents that follow a recent doctor’s appointment or meds change! Always read the fine print. Good luck with getting to America to see your friends!
Rude question answer, “I had my heart removed so insensitive questions like yours won’t hurt it.” But then, I am a brat! 🙂
Elizabeth Youmans RN, BSN
Like Liked by 1 person
My husband had a heart attack and cardiac arrest last week, not sure how much of the large muscle will return but hopeful, and he’s walking and breathing good. We also go abroad. Now feel worried as lots of people who have had heart attacks go, but have not seen any post re cardiac arrest. Whether this makes a difference, also been told as a cardiac arrest person it’s very difficult to get insurance, can you shed any light?
Hi Brian – The good news is that walking and breathing seem fine so far! I just went back and re-read the U.K. report mentioned in my post. You are right – nothing specifically about cardiac arrest; they seem to include that condition within heart attack criteria. Your cardiologist involved will have far more info and be able to advise both of you on the safety of international flights based on unique details of the case. Getting out-of-country travel medical insurance – regardless of cardiac arrest or any other cardiac diagnosis – is fraught with fine print designed to deny medical claims based on how “unstable” the patient’s condition is (but even a doctor’s appointment during the past 90 days at which any treatment decision is adjusted – like decreasing the dosage of a previously prescribed drug because the patient is doing better! – can suggest to the insurance company that the condition is now “unstable”). Talk to a trusted insurance broker for more info. Best of luck to you…
- Pingback: Tea&Biscotti
Hi Carolyn,
This is a very good post and one you should run every year at the start of vacation time. I said that I had been given paper work somewhere regarding travel and not to for this first year. It was clearly written in this post. When I went on my trip, they were running tests on me because of my edema. It dropped my EF (ejection fraction) down to 40% and they still haven’t been able to find out why. I also have congestive heart failure, when I talk about taking a trip I mean going outside of my state.
I went on a 12 hours-one way, and 12 hours-back home trip. I know that they had told me not to take trips without first talking it over with the doctor; this was one of those times in which I looked for someone to agree with me as opposed to following orders.
But it wasn’t an uneventful trip. I began to feel the discomfort shortly after heading back. They wanted to know if I wanted them to get emergency help, and I told them I could make it home. It was a week before I began to feel better.
I won’t make that mistake again, this is a very good posting for all of us, it reminds us of things we try to forget.
Very useful overview for those of us wondering about how soon is “too soon to fly”. Thanks for sharing this.
After I had heart surgery 4 years ago, I worried constantly about having another incident. But my most recently job had me traveling 50 – 75% of the time including many flights or long drives in the car. What my cardiologist was able to reassure me is that my continuing to control my diet, exercise and blood pressure should keep me healthy. Thanks for the article and the common sense flight precautions.
hallo there, thanks for this info on flying.I don’t have heart disease but the last time I flew, at Easter week the woman sitting next to me on the plane suffered a heart attack about 30 min out of Gatwick. The airline staff were very good, and they managed to keep her calm and the plane landed safely within a very short time and she was immed evacuated. I don’t know what happened to her after that but I can see how terrifying it might be if U are a heart patient and U are trapped in a plane. It was certainly terrifying for the rest of us to witness. Thx for your very good work here on this website. Useful and well-done.
Very excellent advice of highest quality on flying following a heart incident. My wife must fly to our daughter’s wedding in two months and already she is worried very much since her own heart incident so I’m showing to her this article. Thank you.
Your opinion matters. What do you think? Cancel reply

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
- Patient Care & Health Information
- Tests & Procedures
- Coronary artery bypass surgery
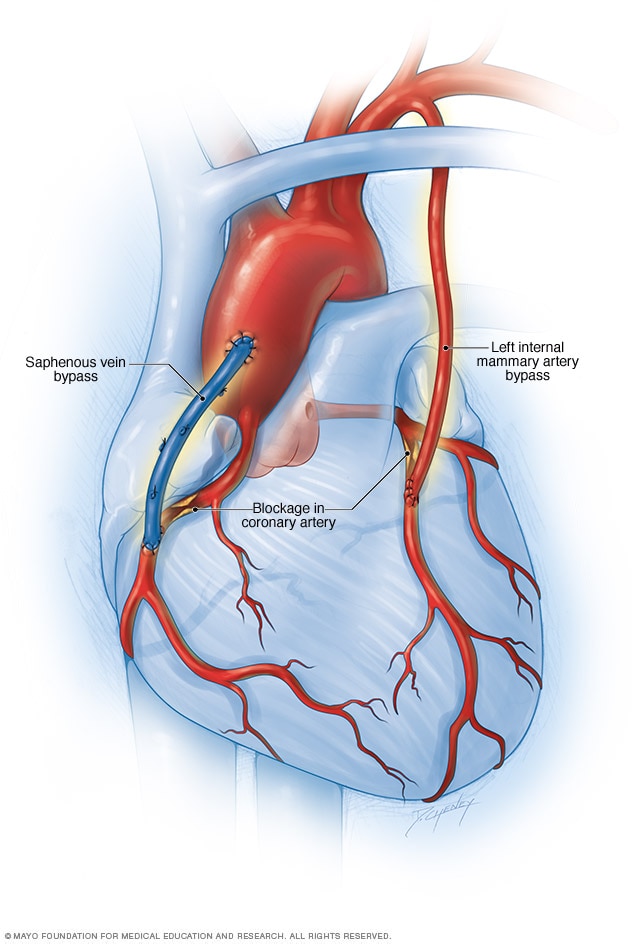
Coronary artery bypass surgery creates a new path for blood to flow to the heart. A healthy blood vessel from another part of the body is used to redirect blood around a blocked area of an artery. Usually the blood vessel is taken from an artery in the chest, called the internal mammary artery. Sometimes it's taken from a leg vein, called the saphenus vein.
Coronary artery bypass surgery creates a new path for blood to flow around a blocked or partially blocked artery in the heart. The surgery involves taking a healthy blood vessel from the chest or leg area. The vessel is connected below the blocked heart artery. The new pathway improves blood flow to the heart muscle.
Other names for this surgery are:
- Coronary artery bypass grafting.
- CABG — pronounced "cabbage."
- Coronary artery bypass graft surgery.
- Heart bypass surgery.
Coronary artery bypass surgery doesn't cure the heart disease that caused a blockage, such as atherosclerosis or coronary artery disease. But it can reduce symptoms such as chest pain and shortness of breath. The surgery, commonly called CABG, may reduce the risk of heart disease-related death.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Coronary artery bypass surgery is done to restore blood flow around a blocked heart artery. The surgery may be done as an emergency treatment for a heart attack, if other immediate treatments aren't working.
Your health care provider might recommend coronary artery bypass surgery if you have:
- A blockage in the left main heart artery. This artery supplies a lot of blood to the heart muscle.
- Severe narrowing of the main heart artery.
- Severe chest pain caused by narrowing of several heart arteries. The narrowing reduces blood flow to the heart even during light exercise or at rest.
- More than one diseased heart artery and your lower left heart chamber doesn't work well.
- A blocked heart artery that can't be treated with coronary angioplasty. This less-invasive treatment uses a balloon on the tip of a thin tube, called a catheter, to widen the artery. A small coil called a stent is typically used to keep the artery open.
- An angioplasty with or without a stent that hasn't worked. For example, an artery narrowed again after stenting.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.

Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Coronary artery bypass surgery is open-heart surgery. All surgeries have some risks. Possible complications of coronary artery bypass surgery include:
- Heart attack due to a blood clot after surgery.
- Infection at the site of the chest wound.
- Long-term need for a breathing machine.
- Irregular heart rhythms, called arrhythmias.
- Kidney problems.
- Memory loss or trouble thinking clearly, which often is temporary.
The risk of complications is higher if the surgery is done as an emergency procedure.
Your specific risk of complications after coronary artery bypass surgery also depends on your overall health before surgery. Having the following medical conditions increases the risk of complications:
- Blocked arteries in the legs.
- Chronic obstructive pulmonary disease (COPD).
- Kidney disease.
Medicines to control bleeding and blood pressure and to prevent infection are typically given before surgery to reduce the risk of complications. If you have diabetes, you may get medicine to control blood sugar during surgery.
How you prepare
Before coronary artery bypass surgery, you may need to make changes to your activities, diet and medicines. Your health care provider gives you specific instructions.
Arrange for someone to drive you home after your hospital stay. Also make plans to have help at home during your recovery.
What you can expect
Before the procedure.
If coronary artery bypass surgery is a scheduled procedure, you are usually admitted to the hospital the morning of the surgery. You have many heart tests and blood tests the days and hours before surgery.
During the procedure
Coronary artery bypass surgery is major surgery that's done in a hospital. Doctors trained in heart surgery, called cardiovascular surgeons, do the surgery. Heart doctors, called cardiologists, and a team of other providers help care for you.
Before you go into the operating room, a health care provider inserts an IV into your forearm or hand and gives you medicine called a sedative to help you relax.
When you are in the operating room, you can expect these things:
- Anesthetics. You receive a combination of medicines through the IV and a face mask. These medicines put you in a pain-free, sleep-like state. This is called general anesthesia.
- Breathing machine. A care provider inserts a breathing tube into your mouth. This tube attaches to a breathing machine called a ventilator. The machine breathes for you during and immediately after the surgery.
- Heart-lung machine. During surgery, a heart-lung machine keeps blood and oxygen flowing through your body. This is called on-pump coronary bypass.
Coronary artery bypass surgery usually takes about 3 to 6 hours. How long surgery takes depends on how many arteries are blocked.
A surgeon typically makes a long cut down the center of the chest along the breastbone. The surgeon spreads open the rib cage to show the heart. After the chest is opened, the heart is temporarily stopped with medicine. The heart-lung machine is turned on.
The surgeon removes a section of healthy blood vessel, often from inside the chest wall or from the lower leg. This piece of healthy tissue is called a graft. The surgeon attaches the ends of the graft below the blocked heart artery. This creates a new pathway for blood to flow around a blockage. More than one graft may be used during coronary artery bypass surgery.
Some variations of coronary artery bypass surgery include:
- Off-pump or beating-heart surgery. Sometimes a heart-lung machine is not used during coronary artery bypass surgery. Instead the surgery is done on the beating heart. Special equipment stabilizes the specific area of the heart being operated on. This type of surgery can be challenging because the rest of the heart is still moving. It's not an option for everyone.
- Minimally invasive surgery. A heart surgeon does the surgery through small cuts in the chest. Minimally invasive heart surgery might be called port-access or keyhole surgery.
After the surgery is done, the health care providers restore your heartbeat in the operating room and stop the heart-lung machine. The surgeon uses wire to close the chest bone. The wire stays in your body after the bone heals.
After the procedure
After coronary artery bypass surgery, a team of health care providers checks on you and makes sure you are as comfortable as possible. You may feel sore and confused when you wake up. You can usually expect the following:
- Breathing tube. The breathing tube stays in your throat until you wake up and can breathe on your own.
- Hospital stay. Expect to spend 1 to 2 days in a hospital intensive care unit. The length of your entire hospital stay depends on how you recover and if you have complications. Some people who have coronary artery bypass surgery go home within a week.
- Heart rhythm and breathing checks. Your health care team watches you closely after surgery to check for complications. Machines record your breathing and heart rhythm. You have frequent temperature checks.
- Medicines. Medicines are given to you by IV to reduce pain and prevent complications such as blood clots. If you don't already take a daily aspirin, your health care provider may recommend you do so. You may need to take the aspirin every day for life. There are specific medical recommendations about who benefits from aspirin therapy. Talk to your health care provider about aspirin use.
- Cardiac rehabilitation. Often called cardiac rehab, this supervised program of education, counseling and exercise helps improve heart health after heart surgery. You'll be encouraged to start moving and walking while you're still in the hospital. When you go home, you continue a cardiac rehab program at a medical center until you can safely follow a home program.
After surgery and when you're at home, you need to watch for symptoms of complications. Call your health care provider if you have:
- Rapid heart rate.
- New or worsened pain around your chest wound.
- A change in skin color around your chest wound.
- Bleeding or other discharge from your chest wound.
It usually takes about 6 to 12 weeks to recover after coronary artery bypass surgery. With your provider's OK, you can usually drive, return to work or the gym, and resume sexual activity after 4 to 6 weeks. But everyone recovers differently. Ask your health care provider for guidance.
After recovering from coronary artery bypass surgery, most people feel better. Some people remain symptom-free for many years. But the graft or other arteries may become clogged in the future. If this happens, you might need another surgery or procedure.
Your results and long-term outcome depend on how well you control blood pressure and cholesterol levels and chronic conditions such as diabetes. It's important to take your medicines as directed.
You can manage and even improve your heart health by making lifestyle changes. Try these recommended steps:
- Don't smoke. Smoking is a major risk factor for heart disease, especially atherosclerosis. Quitting is the best way to reduce the risk of heart disease and its complications. If you need help quitting, talk to your provider.
- Eat healthy foods. Choose plenty of fruits, vegetables and whole grains. Limit sugar, salt and saturated fats.
- Manage weight. Being overweight increases the risk of heart disease. Ask your provider what a healthy weight is for you.
- Exercise. Regular exercise helps control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. With your provider's OK, aim for 30 to 60 minutes of physical activity most days of the week. After coronary artery bypass surgery, your provider will tell you when it's safe to begin exercising again.
- Manage stress. Find ways to help reduce emotional stress. Practicing mindfulness and connecting with others in support groups might be helpful. If you have anxiety or depression, talk to your provider about strategies to help.
- Get good sleep. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Coronary artery bypass surgery care at Mayo Clinic
- What is coronary artery bypass grafting? National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/coronary-artery-bypass-grafting. Accessed Aug. 31, 2022.
- Choi K, et al. Coronary artery bypass grafting in octogenarians — Risks, outcomes, and trends in 1283 consecutive patients. Mayo Clinic Proceedings. 2022; doi:10.1016/j.mayocp.2022.03.033.
- Loscalzo J, et al., eds. Ischemic heart disease. In: Harrison's Principles of Internal Medicine. 21st ed. McGraw Hill; 2022. https://accessmedicine.mhmedical.com. Accessed Aug. 31, 2022.
- Aranki S, et al. Early noncardiac complications of coronary artery bypass graft surgery. https://www.uptodate.com/contents/search. Accessed Aug. 31, 2022.
- AskMayoExpert. Cardiac rehabilitation (adult). Mayo Clinic; 2022.
- Lawton JS, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2022; doi:10.1016/j.jacc.2021.09.006.
- Aranki S, et al. Coronary artery bypass graft surgery: Long-term clinical outcomes. https://www.uptodate.com/contents/search. Accessed Sept. 12, 2022.
- Ami TR. Allscripts EPSi. Mayo Clinic. Aug. 23, 2022.
- Doenst T, et al. PCI and CABG for treating stable coronary artery disease: JACC review topic of the week. Journal of the American College of Cardiology. 2019; doi:10.1016/j.jacc.2018.11.053.
- Bakaeen FG, et al. 2021: The American Association for Thoracic Surgery Expert Consensus Document: Coronary artery bypass grafting in patients with ischemic cardiomyopathy and heart failure. The Journal of Thoracic and Cardiovascular Surgery. 2021; doi:10.1016/j.jtcvs.2021.04.052.
- Lloyd-Jones DM, et al. Life's essential 8: Updating and enhancing the American Heart Association's construct of cardiovascular health: A presidential advisory from the American Heart Association. Circulation. 2022; doi:10.1161/CIR.0000000000001078.
- What is CABG? American Heart Association. https://www.heart.org/en/health-topics/consumer-healthcare/answers-by-heart-fact-sheets/answers-by-heart-fact-sheets-treatments-and-tests. Accessed Sept. 12, 2022.
- Mankad R (expert opinion). Mayo Clinic. Oct. 21, 2022.
- Acute coronary syndrome
- Cardiogenic shock
- Coronary artery disease
- Enlarged heart
- Heart arrhythmia
- Heart attack
- Heart disease
- Heart failure
- Myocardial ischemia
- Spontaneous coronary artery dissection (SCAD)
- Sudden cardiac arrest
- Takayasu's arteritis
- Ventricular fibrillation
News from Mayo Clinic
- Mayo Clinic Healthcare expert shares good news and bad news about angina Nov. 01, 2023, 03:00 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Cardiology & Heart Surgery hospitals in the nation for 2024-2025 by U.S. News & World Report.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.

- See All Locations
- Primary Care
- Urgent Care Facilities
- Emergency Rooms
- Surgery Centers
- Medical Offices
- Imaging Facilities
- Neurology & Neurosurgery
- Obstetrics & Gynecology
- Orthopaedics
- Pediatrics at Guerin Children's
- Urgent Care
- Medical Records Request
- Insurance & Billing
- Pay Your Bill
- Advanced Healthcare Directive
- Initiate a Request
- Help Paying Your Bill
.cls-1{fill:#2e64ab;}.cls-2{fill:#fff;} CS-Blog Cedars-Sinai Blog
Bypass patient on the road to recovery.
May 01, 2019 Cedars-Sinai Staff

Jim Calio was having an ordinary day until he walked up a flight of stairs and nearly passed out. A trip to the Smidt Heart Institute revealed that two of his arteries were 70 percent blocked and that he would need triple bypass surgery .
"I was on track for a massive heart attack if I hadn't taken care of this," Calio says.
Today, thanks to at the institute's Preventive and Rehabilitative Cardiac Center , the 70-year-old journalist is energetic and healthy.
"The crazy thing was that a week before I went in the hospital I was working out every day on machines, lifting weights, and I felt great. "It was when I was walking that I said, 'Something's not right.'"

Jim Calio's dog, Samantha, has been a constant companion through his recovery from triple-bypass surgery. A crucial element of his recovery was the monitored exercise program at the Preventive and Rehabilitative Cardiac Center.
During outings with his dog, Samantha, Calio first felt the shortness of breath that was signaling his heart trouble. But he didn't take the symptom seriously. He knew he had plaque buildup in at least one artery, but he thought he had it under control with cholesterol medications and a healthy diet.
"The crazy thing was that a week before I went in the hospital I was working out every day on machines, lifting weights, and I felt great," he says. "It was when I was walking that I said, 'Something's not right.'"
A crucial element of Calio's recovery was an exercise regimen, which he chose to complete at the Preventive and Rehabilitative Cardiac Center. He could have attended a rehabilitation facility closer to his home, but he wanted to continue working with the Cedars-Sinai staff he trusted.
Read: Shortness of Breath: When to See Your Doctor
"They know me, they have my chart and they are very attentive," Calio says.
"If you let it, a [heart event] can become all-consuming. Early on in the recovery, maybe out of fear, you think, 'Gee, I wonder if it's going to be OK? Will I be able to exercise again?'"
The center is outfitted with equipment designed to assist and strengthen the cardiovascular system. Patients in the exercise program wear heart monitors that display their heart rate and rhythm during exercise. The center's team members closely watch the heart rhythm from monitors and advise patients on how hard to exert themselves on the treadmills, stationary bicycles and other equipment.
Read: Heart Attack, Cardiac Arrest, Heart Failure—What's the Difference?
"My confidence came back right away," Calio says of his experience at the center. "I walked in my neighborhood, too—first without the dog, then with her. I felt great. No huffing and puffing."
Calio has an affectionate nickname for the center: "I call it the Cardio Club."
His dedication to his prescribed exercise and rehabilitation program has been crucial to his full recovery. He is back to his normal exercise routine, including weightlifting, and is planning travel-writing trips such places as London, Hong Kong and Ireland.
"This is a lot of fun, and it's kind of gravy on my career," he says of his travel writing, which he took up after working as a journalist for publications such as People, Newsweek and Life magazines in the 1970s, '80s and '90s. "I'm not going to retire. I'll keep cranking out stories as long as I can."

Jim Calio walking with his dog Samantha after undergoing triple bypass surgery at Cedars-Sinai.

Popular Categories
Blog & magazines, popular topics, make an appointment, call us 7 days a week, 6 am - 9 pm pt, support cedars-sinai.

Congenital Heart Defect/Disease
11 things no one warns you about after open-heart surgery.
Like any surgery, before you go in for open-heart surgery they mostly warn you about the risks of surgery. They discuss what could happen during the surgery, things that could go wrong, and anything specific to the type of heart surgery you are having. They speak of recovery time in general terms. I was born with a congenital heart defect called transposition of the great arteries. I still have a mustard procedure in place. After three open-heart surgeries, I have to say there are many things that I wish they would’ve warned me about during my surgeries.
1. Recovery from open-heart surgery takes time.
The suggested recovery time is always longer than what they tell you. While you might be able to return to most regular activities, it can take your body a full year to recover from open-heart surgery and it might even take longer for you to feel back to your normal. My most recent, third open-heart surgery was two years ago and I’m still recovering.
2. Open-heart surgery can cause hair loss.
Be prepared to lose a lot of hair after surgery. I have really long thick hair and I lost a lot of it after my most recent open-heart surgery. There are a couple of reasons why you use a lot of hair after open-heart surgery. One of the big factors with hair loss is the stress open-heart surgery has on your body. Another possibility is because of the long amount of time you are under for cardiac surgery and being in one place which can cut blood flow to your hair follicles. Sometimes medications can be the cause of hair loss. Taking supplements such as biotin and zinc can help with hair regrowth, but make sure to check with your doctor first.
3. Your personality and mood may change after open-heart surgery.
After open-heart surgery, many people experience personality and mood changes. The most commonly experienced emotions are depression , fatigue, and anxiety . These can be caused by being on bypass, anesthesia, or medication such as oxycontin. You may experience mood swings like crying or getting angry or easily frustrated.
I mostly experienced this after my second open heart surgery when I was a teenager and my third open-heart surgery. After both of them, I experienced depression, anxiety and PTSD. Before my second open heart surgery, I was more outgoing but afterward, my personality changed and I was quieter and self-reflective. I struggled with suicidal thoughts and mood swings. After my most recent surgery, I finally got the therapy I needed after years of not seeking help. If you are struggling, please find help, be open with your doctor and make sure you have someone to talk to.
4. You may experience collarbone and sternum pain after open-heart surgery.
Sometimes you can have prolonged collarbone and sternum pain. Collarbone pain and sternum pain can be caused by the trauma of the surgery on your body or sternal wires. This pain can be sometimes helped with cardiac rehab or a resternotomy. However, make sure to communicate with your doctor about your pain to make sure it’s normal. After this past open heart surgery, I’ve had a lot of pain and clicking in my shoulders and chest. It’s caused a lot of chronic pain but working with physical therapy has helped me regain strength.
5. A chest pillow is a must.
Having a pillow to stabilize your chest is a must. Most hospitals will send you home with one, but if they don’t, make sure to get one. Chest pillows can help you when you sleep, sneeze, and cough; they have many uses. I had a pillow with me for almost a year after my last surgery and I still use one during long trips in the car.
6. Car rides after heart surgery may be uncomfortable.
The ride home from the hospital after open-heart surgery will be hard. Make sure to have your chest pillow and a seatbelt cover as well. You will feel every bump, turn, and stop. It will take some time before it will not be painful to be in the car.
7. Sleeping can be hard after surgery.
It’s hard to find a comfortable position to sleep in. If you are a side or belly sleeper it can be hard laying on your back. Finding your favorite chest pillow will be your savior. You might also experience nightmares for a bit after surgery, but it will pass. If you continue to experience them, speak to your doctor and seek help if you feel like you are experiencing PTSD.
8. After open-heart surgery, you may have a poor appetite.
Usually, this goes away after a couple of weeks. But I remember nothing tasted good. I remember everyone raving about how the hospital food was so great and it all tasted like cardboard to me. I felt the same when I got home. Nothing tasted good, even my favorite foods. Even if you don’t feel hungry, it’s important to make sure to eat well and stay hydrated.
9. You may experience memory loss and/or brain fog.
There are a couple of things that can cause memory loss and brain fog after open-heart surgery. If you were put on bypass, it can cause these issues. It is also called “pump head.” Post-operative cognitive dysfunction (POCD) can also cause memory loss. Both of these are usually short-term but can have the possibility of long-term effects. For the first six months, I really struggled with memory loss and brain fog. As time went on, it started to get better and I started to regain my memory and wasn’t so foggy-headed.
10. Hormonal changes can occur after heart surgery.
For women, your period can be affected by the surgery. It can be temporary or even in cases has permanently been changed. Your periods can become irregular, heavy, lighter, or more painful. Whenever I’m in the hospital for some reason my body just automatically decides it’s going to have my period even though it’s not that time.
11. Wearing certain types of clothing might be hard during surgery recovery.
Usually in discharge, they tell you to wear button-down clothing for a while, but what they don’t tell you is that your skin is super sensitive and wearing tight clothing even a couple of months after might be hard. For women, wearing bras might be tough. Try to find comfortable sports bras you can unclasp or undershirts. I tend to wear bras now that don’t have underwires and have a t-shirt cotton feel.
If you or someone you know needs help, visit our suicide prevention resources .
If you need support right now, call the National Suicide Prevention Lifeline at 1-800-273-8255, the Trevor Project at 1-866-488-7386 or reach the Crisis Text Line by texting “START” to 741741.
Image via contributor
Amelia Blackwater is a chronic illness and mental health writer and poet. She graduated from CSUSB with a BA in Creative Writing in 2011. She finds therapy in writing about her experiences living with CHD, migraines, multiple mental health problems including C-PTSD, Anxiety Disorder, OCD, and recovered Eating Disorder She recently is on the mend from her third open heart surgery. Follow her journey on Instagram @ameliablackwater
Triple Bypass 2 years on.: I sometimes... - British Heart Fou...
British heart foundation, triple bypass 2 years on..
I sometimes reply to the questions and experiences of others but I don't instigate threads, so this is an exception.
Two years ago today, age 64, I was in surgery for triple CABG following a heart attack and one stent in 2019, and a return of some symptoms such as pressure in upper chest and awful jaw pain (which was the signal for the original heart attack) around March, April 2021. Recovery was slow but steady. They'd warned me that it could be "2 years before you know what you'll finish up with".
Recovery was slow but steady, and I had problems with my left lung which collapsed during surgery, had to be reinflated and afterwards repeatedly filled up with fluid, leading me to A&E on one occasion. Three months after surgery I went back to playing my badminton in a "not pushing it" way. I did cardiac rehab which I can thoroughly recommend, and I keep fit in the gym and with walks that can be up to 10 miles. After a year I felt much better.
So where am I now, what are my concerns, and how does my experience compare with others, I wonder?
Taken all round, I guess I'm ok. I can do much of what I did before. Work out at the gym, play badminton almost back to my former level and even do a Parkrun now and then. Life is good and precious. I'm thankful for the expertise that got me to here.
Concerns/problems:
I do get discomfort in the chest. A lot of it is to do with the surgery, I know. The cutting of the flesh, nerves and bones has certainly left its mark and I experience numbness, tingling and soreness even now. I doubt at this stage that it will ever resolve. It's a fairly low level nuisance in the grand scheme of things though.
More concerning, I can occasionally get what I term as angina pains and I am not sure why this should be after the bypass. A sort of burning in the upper chest that seems to permeate from back to front. The GTN spray has never had any effect on me so I've given up using it. Such pain and discomfort in my case is never exertion related. It's invariably at rest, perhaps after eating a meal or it will wake me in the small hours. If I followed the guidance to the letter I would be at A&E on every episode of this, but I think after a while you get a feel for what is the new normal for you, and somehow, although it is not nice it doesn't FEEL like I'm having another heart attack, if that makes sense. I wonder if it's some other deterioration in the condition of the heart. Perhaps a declining ejection fraction. I just don't know, but after it clears up, I'm as good as before, playing my badminton etc.
I've considered the possibility that the phenomenon is subconsciously mental, perhaps anxiety related, but I'm not an anxious person in any way. Even immediately before the CABG I wasn't particularly concerned. I knew I needed to have it done and just thought what will be will be, and now I never lie awake worrying about another heart attack.
So there it is. Heading for 4 years after HA, 2 years after CABG, I'm still here doing my thing. Plenty of good life quality, but with these few niggles and concerns.
Does this ring true with others who have travelled a similar road? I'd be fascinated to know.
- Glyceryl Trinitrate
- Percutaneous coronary intervention
Hi RailRover
I’m sorry to hear you’re experiencing chest pain even after your CABG.
I can resonate with the chest pain on rest however. I have a congenital heart defect in the form of myocardial bridging which causes vasospastic angina. This is when my arteries become constricted and there is a lack of blood supply to my heart. I experience the chest pain on a daily basis, but have noticed it can be more severe and higher in intensity during rest.
You mentioned that you have not been responding to your GTN spray. Vasospastic angina can also be resistant to nitrates.
Have you checked in with your cardiologist and let them know about your symptoms? If not, I would recommend you do this as further testing may be required to rule out anything new.
Keep us posted on your progress.
All the best.
'Vasospastic angina can also be resistant to nitrates.'
Responding to nitrates during an episode of angina is a diagnostic criteria of vasospastic angina.
For more information please see the Coronary Vasomotor Disorder International Study Group COVADIS, definitions of vasospastic angina and the BHF website information about vasospastic angina.
covadis.online/definitions/
bhf.org.uk/informationsuppo... .
Interesting. I do not always respond to my GTN spray during a spasm. Perhaps I should’ve phrased that as “my vasospastic angina” instead of “vasospastic angina”.
There is growing evidence that nitrates are not effective for people living with microvascular angina.
It's really important to be able to work with a Cardiologist who understands microvascular and vasospastic angina as well as being able to offer the appropriate testing.
Without appropriate testing we are left with assumptions and uncertainty, which isn't helpful.
Have you been able to access a knowledgeable Cardiologist to help you?
I’m currently taking a medication which can help with the symptoms of MVA. It’s still early days, so I am just monitoring its effects on my symptoms for the time being.
Medication changes were made by a cardiologist who treated me abroad. He seems to be more knowledgeable about coronary artery spasms in comparison to the cardiologists I have consulted in the U.K. so far. This includes both the private sector and NHS.
The UK has some of the leading researchers and world leading experts in caring for patients living with microvascular and vasospastic angina. I believe I have already provided you with some suggestions of some Cardiologists who maybe able to help you.
I have a very good team of knowledgeable and empathetic Cardiologists at the hospital in north London I attend.
Microvascular and vasospastic angina are often mistakenly considered to be the same. They are different with different underlying causes with different treatment options.
I hope you can find the support you need here in the UK.
Thanks for your thoughts. Possibly worth exploring other cardiac issues.
You may find these articles helpful. bhf.org.uk/informationsuppo...
acc.org/latest-in-cardiolog... .
Thank you RailRover, you have given me such hope!!! I am also a survivor of double cabg in January of this year, so still in early days of recovery. I dont know about you, but I got very little advice post op? I've had to find things out in my own as I've recovered!! I'm hyper aware of any niggles in chest area now!! The emotional part of the recovery is the hardest !! So much crying!! Have you experienced the same? I'm trying to be as positive as I can and hope that this is it for me now and that the op has worked. My condition is hereditary..I've had 3 heart attacks since 2021 and 2 stents which collapsed so needed the bypass. I'm also a member of the pumping marvellous forum but am considering coming off it for a while as there seems to be an awful.lot of people posting scare mongering replies to people who just ask a simple question!! For new members, or people like me with health anxiety it's not good. It was so nice to read a positive uplifting story for a change so thank.you!!!
I'm glad you got something from it! Not really a crying sort of person. More a "what will be, will be" sort. You are right. The acute care is top notch, but the further from that you get, the support soon drops away. Have you done rehab? If not, I urge you to go. It will put you on your feet again.
hi- I can def relate to the chest discomfort but this year 4 years on it’s hardly there & the tingling has finally gone- so don’t give up on it getting better. I too thought it would never go but it did eventually!!
Thank you for that! There is hope yet then.
I'm coming up to 6 years post HA and stents and 5 years post triple bypass. I get many of the physical issues related to bones, nerves and skin as you do, but absolutely none of the internal pain. What is interesting is that you still are prescribed GTN whereas for me it was noted as being "contra-indicated" and I stopped having a spray when I had the bypass (not as though I ever used it anyway). I wonder whether that is down to our personal situations or local protocol at the hospital we had our ops.
As far as physical abilities are concerned, I've definitely recovered my health to pre-HA levels. Two months after my op, I walked 10 miles non-stop. I've managed 17 miles non-stop and was on for 20 miles last year, but had to stop for a rest as the day was too hot! I now climb Munros up in Scotland, indeed on occasion have done pairs of Munros. I do feel I am starting to slow up a bit, but at 71 carrying a 11kg backpack up these lumps of granite (so I can participate in my other pastime of Amateur Radio from the summits), well it can't be that bad.
I would certainly get any "unexplained" symptoms checked out. Prevention is better than cure. The way I look at it is that the NHS has invested in us by doing the bypass operations and it is our responsibility to protect that investment. Just like a car needs maintenance from time to time, we need to be maintained. Maybe you just need a drop of Castrol R in your tank. Now I am showing my age! 😀
All the best, Gerald
Great stuff! Good to hear you are doing so well.
My stories on here somewhere not sure if it’s possible for you to go and find it?To précis my experience I had my triple by pass aged 31, I am now nearly 77.Never had a heart attack got angina at the limits of exertion and a great doctor not happy with a normal ecg at rest insisted on an exercise test as HAs were becoming more frequent at younger ages.
Thanks to a great late surgeon Mr Parker at St Georges Hyde Park Corner and after cancellation after my first attendance,(my blood a rare B Rhesus Negative was used for a poor lady in a road accident),I had a successful op in August 1977.
These days I cycle and age 77 play a tough game of walking football twice a week.Of course after major surgery like that you pick up on every strange feeling you get as a portend of something sinister, which before in the normal course of life you wouldn’t give a thought to.So there’s certainly HOPE I am hoping to get an entry in the Guinness Book of Records as the longest surviving triple bypass patient.Tempting providence but how far I’ve got astounds me when at 31 I thought I would never reach here.
You're an inspiration, Bigscar and I'm sure we're all looking forward to celebrating your entry into the Guinness Book of Records. (Oh, and you're making me feel like a couch potato and encouraging me to get out there and do some more exercise! 😂😂) Carol
hi bigscar this is inspiring I’m only 5 years post quad bypass and just recently have felt down due to tiredness the docs have said don’t do so much and some people just get tired so no help there coming on here has shown me that all people are different and react differently to the same medication or operation I was beginning to think I was coming to the end of my journey but you have helped me realise it’s part of the journey and I could still have years to go
hi RailRover
An excellent article and in many ways reassuring, that’s me with a few variations 2 years on from my CABG
All the best
Hi RailRover I’m still quite early days 18 months compared to you, mine was a Stemi couldn’t fit Stents so bypass it was it all happened so quickly, I would also Recommend I’m walking with our dogs do at least 3x 5 miles a week and the other 4 between 2& 3 miles along with some utube workouts, I too have a GTN spray only used it twice had to go back to A& E a couple of times
If you feel any different please go see someone even a call to the doctor get some checks done, I think like you say it’s a new normal and we will have little niggles but we also need to act upon these if unduly worried
Wish you all the best 😊
Hello RailRover. You should speak to your GP. Angina symptoms aren't usually an emergency but they do need investigating. You need your GP to refer you to a chest clinic for a proper evaluation. Probably nothing, but better safe than sorry.
Hi Rail Rover,
From your symptoms and the fact that it happens at rest and after eating might point towards acid reflux. I suffer from this and what you’re describing sounds very similar to what I experience.
Have you tried Gaviscon or similar when your symptoms appear? Might be worth a try?
I hope you get to the bottom of it soon.
Thanks. I have tried Gaviscon, but that doesn't seem to shift it.
Hello RailRover. 8 years on from Heart Attack and triple CABG. No symptoms of any angina or breathlessness and pain pre op. No GTN prescribed after op or indeed needed. However, 6 months ago I had an OHSCA (Out of Hospital Sudden Cardiac Arrest ) treatment for this was a defib/pacemaker implanted. Had GTN spray prescribed as now seem to be back to square one with low level breathlessness and tight chest on to much exertion. So feel a bit peeved. But im
Sorry to hear of the setback, but I hope you are fighting back.
hi railrover I was put on lanzoprasole after my bypass which helps with acid stomach which you might have perhaps a chat with the doctor?
Yes. I have that too as a daily med.
I'm four years on from a double bypass, and much of what you say resonates with me. I don't think there's been a day when I wasn't aware that my chest had been operated on. Whilst I've no signs of angina, there have been odd days, maybe once a year, when it's been significantly worse, and I have got so uncertain that I have reported for medical advice. However, I've always been given a full working over followed by a clean bill of health, so I completely agree that there are signs that, otherwise, I might have taken as indicators of heart problems, that appear instead to be just consequences of being pulled around in the operation.
Like you, I don't tend to worry much, but to take things as they come. I've made a full recovery, gone back to club cycling and, last year, did RideLondon (100 miles).
I did have a couple of passings out at Easter, resulting in a trip to hospital, but that seems to have been more to do with naturally-low heart rate exacerbated by my bisoprolol. The consultant has stopped that and it looks like that's going to be it.
Yes. Bisoprolol had my pulse rate down under 40 at times. They were reluctant to take me off it, but falling about all over the place isn't really my bag. Off it and back to my pre HA resting pulse rate of 52 now. I think they can be guilty of a little too much "one size fits all" with the prescribing and they aren't keen to deviate from it.
I actually did the passing out thing again at the beginning of August, while on a Scout expedition to Scotland of all times and places. Off to the nearest hospital, usual checks, nothing untoward found, ordered to report back to the local team when I got home (same ones as took me off Bisoprolol at Easter). I've now had a loop recorder implanted, to try to find out what's going on. But apart from those two incidents I've been fine, as usual (which of course means that there doesn't seem to have been much of interest for the recorder to record...) bhf.org.uk/informationsuppo...
Thanks to each and every one who has taken the trouble to respond. All most interesting and very much appreciated!
RailRover, I am nearly 24 months post double LAD CABG and I am mirroring everything you’ve said post Op regarding aches pains and worries. Ive looked after myself my whole life keeping super fit, watching my weight, drinking in moderation and having a reasonable diet yet I still have coronary heart disease.
I’m still coming to terms with my new normal but getting on with my life without clogging up A&E.
Not what you're looking for?
You may also like..., new recent life update.
It's hard right now
Extending My Guinness World Record
What should i expect one year post nstemi.
Bisoprolol side effects
Related Posts
Moderation team
Popular Posts
Content on HealthUnlocked does not replace the relationship between you and doctors or other healthcare professionals nor the advice you receive from them.
Never delay seeking advice or dialling emergency services because of something that you have read on HealthUnlocked.

- Weill Cornell Medicine

- When You Can Fly
Generally, you should wait to fly until after you have had your first postoperative visit with your surgeon.
- Remember that in the airport terminal, you may not have the stamina to walk as fast or far as you did before the surgery.
- Also remember that you cannot carry anything heavier than 10 pounds for the first six weeks after the surgery, so you'll have to arrange for your heavier bags to be carried by someone else.
Related Links
- Postoperative Incisional Pain
- When You Can Drive
- Diet Following Stomach Fundoplication
Contact Us Digital Health Services
Weill Cornell Medicine Cardiothoracic Surgery 525 East 68th Street Box 110 Suite M 404 New York, NY 10065 Directions Phone: (212) 746-5166 Email: [email protected]
- Your Presurgical Appointment
- The Day of Your Surgery
- Information for Families
- Guide to Heart and Aortic Surgery
- Guide to Lung, Stomach, Mediastinal, or Esophageal Surgery
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
- What to Expect
Triple Bypass Surgery: What to Expect on the Day of Surgery
Before the surgery, during the surgery, after the surgery.
- Next in Triple Bypass Surgery Guide Triple Bypass Surgery: Recovery
Triple bypass surgery is a major surgery that takes between three to six hours. It requires general anesthesia, meaning you'll be unconscious while it's happening. On average, you'll remain in the hospital for up to seven days.
By understanding what happens before, during, and after triple bypass surgery, you can increase your chances of success.
The day of triple bypass surgery can be hectic and overwhelming. If the surgery is planned, you will have more time to prepare both mentally and physically for the procedure. If it is an emergency, preoperative tests are very time sensitive and multiple examinations may be happening at once.
On the day of the procedure, you will meet with the entire healthcare team including the cardiothoracic surgeon , cardiologist, anesthesiologist , perfusionist , operating room nurses, and other surgeons as needed. All operative consent forms will be signed at this time to ensure you are fully prepared and do not have any additional questions or concerns.
The registered nurse will take vital signs including:
- Blood pressure
- Temperature
- Respirations
- Pulse oximetry
Prior to going into the operating room for the procedure, patients will have preoperative tests done. This may include:
- Echocardiogram
- Electrocardiogram (EKG or ECG)
- Chest X-ray
- Carotid ultrasound
- Pregnancy test (if indicated)
You will also be given a surgical soap that must be used on the surgical sites to properly cleanse the area and prevent infection. After cleaning, you will be given a hospital gown and the nurse will shave the surgical area if needed. The surgeon will mark the surgical site after you are fully prepped.
Your medications will be reviewed by the nurse and surgical team. Be prepared to discuss all of your medications, vitamins, and supplements at this time including the dosages, the last time they were taken, and how often they are taken. Bringing a list of the information is helpful so nothing is missed.
Patients are instructed to empty their bladder prior to going into the operating room, and asked to remove all jewelry, glasses, contact lenses, and dentures if applicable.
Finally, the nurse will insert an intravenous catheter (IV) that will be used to provide hydration, medications, and anesthetics during the procedure.
When it’s time for the surgery, you will be taken into the operating room on a stretcher and then placed onto the operating room table. You will then be prepared for general anesthesia , which will last for the duration of the surgery. Before the operation begins, the following will take place:
- You will be given a small dose of medication to help you relax while the surgical team is preparing.
- Vital sign monitors are placed.
- Your skin will be cleaned again with surgical cleaner and draped in sterile drapes, exposing only the surgical area(s).
- Once you are sedated by the anesthesiologist, an endotracheal tube will be placed to help you breathe during the procedure. Anesthesia medications relax your muscles making it difficult to breathe and this procedure will allow the team to help control your breathing while on the ventilator .
Once you are fully prepped for surgery, the surgical team will first harvest the three vessels needed for the bypass. Blood vessels can be taken from your leg ( saphenous vein ), inside your chest (internal mammary artery), or your arm ( radial artery ).
After the surgeons harvest the vessels, a midsternal vertical incision is made in the center of the chest in order to access the heart. The patient may be placed on a bypass machine during the procedure depending on the surgeon. The surgery can be performed "on-pump" or "off-pump".
On-pump surgery refers to the use of a heart-lung machine that circulates blood and breathes for the body throughout the surgery. The machine allows doctors to stop the heart.
The second technique used is off-pump surgery , also called “beating heart surgery.” It is done while the heart is still beating, and does not use the heart-lung machine. This is a more difficult surgery to perform because of its technical precision, but is the preferred approach for some surgeons.
According to the National Institute for Health and Care Excellence (NICE) , the procedure works as well as a coronary artery bypass using a pump. It is a newer technique that has shown some increased benefits, including:
- Quicker than the conventional procedure
- Reduces the chance of bleeding during the surgery
- Decreased risk of certain serious complications after surgery, such as a stroke
- Shortened hospital stay
After the grafts have been placed, the heart is restarted (if needed) via controlled electrical shocks. The surgical incision is closed using mesh webbing, sutures, and/or staples depending on the surgeon's preference.
Immediately following triple bypass surgery, you will be transferred to the intensive care unit (ICU) or cardiac intensive care unit (CICU or CCU) for close monitoring. You will typically have an endotracheal breathing tube for several hours after surgery and still be connected to a ventilator.
You will be given medication to keep you sleepy. If you start to wake up, you will not be able to talk with the breathing tube. It may feel uncomfortable but shouldn't be painful. Once fully awake, the breathing tube will be removed.
You will spend a minimum of one day in the intensive care unit and will be hooked up to a variety of machines including a monitor for vital signs, an IV pump to deliver fluids and medications, and a catheter to drain your bladder.
After the initial ICU recovery, you will be moved to a post-surgical unit to continue your recovery. At this time, you will meet with a physical therapist, occupational therapist, and nutritionist to continue the recovery process.
Following the procedure, everything will be harder to do including eating, dressing, bathing, and other activities of daily living. This is normal and to be expected after undergoing triple bypass surgery. Working with the healthcare team will help you start to feel more normal.
A Word From Verywell
It's important to follow all instructions from the healthcare team before, after, and during triple bypass surgery. This surgery, while the most common open heart procedure, is very serious and there is the possibility of life-threatening complications.
Discuss any concerns and questions with your surgeon prior to the procedure to fully understand not only the surgical procedure but also the recovery process.
Society for Cardiovascular Angiography and Interventions. Your care team during coronary bypass surgery .
National Heart, Lung, and Blood Institute. Coronary artery bypass grafting .
Johns Hopkins Medicine. Coronary artery bypass graft surgery .
University of Michigan Health. Coronary artery bypass surgery: When you arrive at the hospital .
Martínez-González B, Reyes-Hernández CG, Quiroga-Garza A, et al. Conduits used in coronary artery bypass grafting: A review of morphological studies . ATCS . 2017;23(2):55-65. doi:10.5761/atcs.ra.16-00178
Melly L, Torregrossa G, Lee T, Jansens JL, Puskas JD. Fifty years of coronary artery bypass grafting . J Thorac Dis . 2018;10(3):1960-1967. doi:10.21037/jtd.2018.02.43
Johns Hopkins Medicine. Off-pump coronary artery bypass surgery .
National Institute for Health and Care Excellence. Off-pump coronary artery bypass grafting: Interventional procedures guidance . Published January 26, 2011.
By Kathleen Gaines, MSN, RN, CBC Kathleen Gaines, MSN, RN, CBC, is a nurse and health journalist, as well as an adjunct clinical faculty member at hospitals in the Philadelphia area.

IMAGES
COMMENTS
Two weeks. The National Health Service recommends checking with your airline BEFORE flying, since companies have varying regulations on post-surgery travelers. However, the Civilian Aviation Authority says that 10 to 14 days is sufficient after chest surgery or a coronary artery bypass graft. After any heart operation, patients should remain ...
After triple bypass surgery, most people stay in the hospital for five to seven days. Once you've returned home, it can take up to 12 weeks to fully recover. During this time, your healthcare provider will likely refer you to an outpatient cardiac rehabilitation program. Find out how to recover from triple bypass surgery, including recovery ...
How soon after open heart surgery you can fly depends on your doctor's recommendation about your overall condition and other factors. For example, if you've had a minimally invasive cardiac surgery with no complications, you may be able to fly within two to four weeks. For more moderate or intense open heart surgery, such as heart bypass ...
Those who have had heart valve repair or replacement surgery or coronary artery bypass grafts (open heart surgery) can usually fly after 4-6 weeks (longer if they have had pulmonary complications). Generally speaking, if you can walk briskly for 100 metres on the flat without being breathless or in pain, you can fly.
This is called on-pump coronary bypass. Coronary artery bypass surgery usually takes about 3 to 6 hours. How long surgery takes depends on how many arteries are blocked. A surgeon typically makes a long cut down the center of the chest along the breastbone. The surgeon spreads open the rib cage to show the heart.
Life expectancy after a first bypass surgery is estimated to be 18 years. This varies based on many factors, such as age and overall health. Survival rates after a triple bypass have been shown to be about 71% at 10 years, 28% at 20 years, and 9% at 30 years.
When you get home from the hospital, you might experience: frequently and go away within a couple of weeks. If it worsens, contact your surgeon. • Muscle pain or tightness — You might feel discomfort. • Reduced appetite — It takes a few weeks for your appetite to return. Your sense of taste may be weaker and certain smells might make ...
CABG can be lifesaving. The average life expectancy after CABG is about 18 years . CABG is a major operation that can take between 3 to 6 hours to complete. And most people make a good recovery — serious complications after CABG surgery aren't common. Heart surgeons go through years of specialized training.
Heart bypass surgery is a procedure to improve blood flow to your heart when you have coronary artery disease. A surgeon takes a blood vessel from another part of your body to go around, or bypass ...
Coronary bypass surgery treats blockages or the narrowing of one or more arteries that surround the heart. This operation aims to restore blood supply to the heart muscle. Your doctor will likely ...
Apply lidocaine patches to minimize pain and itching near your incision site. Hold a pillow to your chest. This is especially important when coughing or laughing. Use a heating pad or ice pack ...
You can expect to return to the comfort of your own home within a week. "The first two weeks are the most important period after having open-heart surgery," says Dr. Bhusri. The primary concern at this time is the incision from the surgery. "We have to make sure the incision stays clean and sterile.".
When planning to go on holiday with a child who has a heart condition, speak to your GP or heart specialist before booking a holiday to make sure the child is able to fly or take a long journey. Give yourself time to order enough medicines for the holiday, and to arrange transport options. If you need assistance at the airport terminal or ...
Heart bypass surgery, or CABG, is a major operation that requires careful recovery. In this article, you will find helpful tips on how to manage pain, wound care, diet, exercise, and emotional well-being after the surgery. You will also learn about the possible complications and long-term outcomes of CABG. Read more on Verywell Health, a trusted source of health information.
Bypass Patient on the Road to Recovery. Jim Calio was having an ordinary day until he walked up a flight of stairs and nearly passed out. A trip to the Smidt Heart Institute revealed that two of his arteries were 70 percent blocked and that he would need triple bypass surgery. "I was on track for a massive heart attack if I hadn't taken care of ...
9. You may experience memory loss and/or brain fog. There are a couple of things that can cause memory loss and brain fog after open-heart surgery. If you were put on bypass, it can cause these issues. It is also called "pump head.". Post-operative cognitive dysfunction (POCD) can also cause memory loss.
Triple Bypass 2 years on. RailRover •. 1 year ago • 31 Replies. I sometimes reply to the questions and experiences of others but I don't instigate threads, so this is an exception. Two years ago today, age 64, I was in surgery for triple CABG following a heart attack and one stent in 2019, and a return of some symptoms such as pressure in ...
Your surgeon took a vein or artery from another part of your body to create a detour, or bypass, around an artery that was blocked and could not bring enough blood to your heart muscle. Your surgery was done through an incision (cut) in your chest. If the surgeon went through your breastbone, the surgeon repaired it with wire and a metal plate ...
Generally, you should wait to fly until after you have had your first postoperative visit with your surgeon.Remember that in the airport terminal, you may not have the stamina to walk as fast or far as you did before the surgery.Also remember that you cannot carry anything heavier than 10 pounds for the first six weeks after the surgery, so you'll have to arrange for your
Triple bypass surgery is a major surgery that takes between three to six hours. It requires general anesthesia, meaning you'll be unconscious while it's happening. On average, you'll remain in the hospital for up to seven days. By understanding what happens before, during, and after triple bypass surgery, you can increase your chances of success.
Two and a half weeks after her triple bypass. She was tired and sore but we made it home without complications. Thank you all for your advice and sharing your stories...it really helped us. Original Post: My mom just had triple bypass, it's been 8 days and she has been doing better everyday.
The bypass surgery had to be delayed a few days. Linda's triple bypass surgery was a success, but days later, while in recovery, she had a stroke. Doctors were able to remove the clot that caused ...
In a 2021 study, researchers found that the operative mortality of coronary artery bypass surgery was 2.2%, meaning that 2.2% of people passed away within 30 days of getting the surgery. Preparing ...
She needed a triple bypass to restore normal blood flow through her heart. While doctors were examining her, Linda's heart stopped. It took three shocks from a defibrillator to restore a rhythm. The bypass surgery had to be delayed a few days. Linda's triple bypass surgery was a success, but days later, while in recovery, she had a stroke.