

Miscellaneous HCPCS (A9999 and E1399)
- Last updated
- Save as PDF
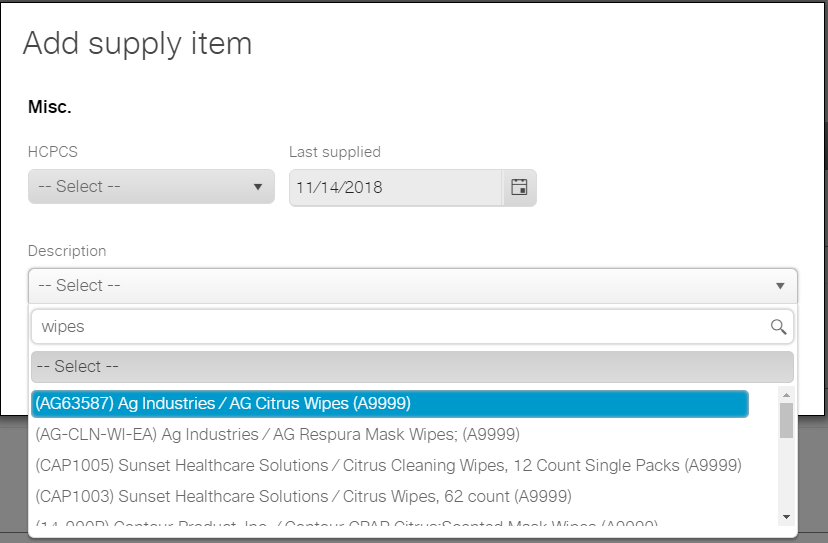
You can use the following codes to request miscellaneous CPAP-related supplies:
- A9999 for accessories
- E1399 for device-related supplies
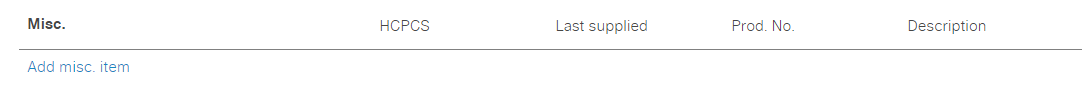
Client services representatives and Faith (the interactive voice response system) don't typically ask patients if they require miscellaneous supplies during outreach. However, these codes allow you to offer other supplies to the patient to maximize the supply request and maintain all details within ResMed ReSupply for better reporting.
Examples of miscellaneous items include:
If you're unsure which HCPCS code applies to the miscellaneous supply item, begin to type the description in the Description field. The appropriate code displays and then you can select it.

Sleep Comfortably. Sleep Peacefully. Sleep Restfully.
Cpap, oxygen equipment & supplies at low prices, 1-866-923-2727.

- Inogen One G5
- Inogen One G4
- Respironics SimplyGo Mini
- Respironics SimplyGo
- Inogen One G3
- ResMed Mobi Portable Concentrator
- Sequal Eclipse 5
- Oxlife Independence
- FreeStyle Comfort Portables
- Invacare Platinum Mobile
- All Portable Concentrators
- Stationary Oxygen Concentrators
- Oxygen Supplies
- Pulse Oximeters
- Air Travel with Concentrators
- Portable Oxygen Comparison Chart
- Stationary Oxygen Comparison Chart
- Print Pulse Dose POC Chart
- Print Continuous Flow POC Chart
- Print Stationary Comparison Chart
- Philips Respironics
- Fisher & Paykel
- Braes Z2 Travel CPAP
- Transcend miniCPAP
- Resvent and Apex
- BiPAP & VPAP Machines
- Heated Humidifiers
- Travel CPAP Machines
- APAP Machines
- CPAP Machines
- CPAP Comparison Chart
- BiPAP Comparison Chart
- Print Auto PAP Comparison Chart
- Print CPAP Comparison Chart
- Print BiPAP Comparison Chart
- Nasal Pillow Mask
- Full Face Mask
- Bleep DreamPort
- SleepWeaver
- InnoMed Technologies
- ResMed Build A Mask Kit (No Rx)
- Fisher Paykel Build A Mask Kit (No Rx)
- Mask Headgear
- Mask Comparison Chart
- AirFit/AirTouch N20
- AirFit/AirTouch F20
- AirFit N30i and P30i
- AirFit F30i
- Quattro Air
- Swift FX Nano
- Mirage Activa LT
- Mirage Quattro
- Ultra Mirage Full
- Mirage Micro
- Mirage Liberty
- Ultra Mirage II
- Mirage Activa
- Mirage SoftGel
- Wisp Nasal Mask
- DreamWisp Nasal Mask
- DreamWear Nasal/Pillow
- DreamWear Full Face
- ComfortGel Blue
- ComfortGel Blue Full
- FlexiFit 432
- FlexiFit 407
- FlexiFit 406
- FlexiFit 405
- AirMini Parts and Supplies
- ResMed Machine Parts
- ResMed Humidifier Parts
- DreamStation Parts
- DreamStation Go Parts and Supplies
- Respironics Machine Parts
- Respironics Humidifier Parts
- F & P Parts & Accessories
- Breas Z1 and Z2 Parts
- Transcend Parts & Accessories
- Respironics
- Z1 (HDM) and Braes
- 3B Products
- Apex XT, ZZZ-PAP & Puresom
- Mask Liners and Pads
- CPAP Cleaning & Moisturizing
- CPAP Sanitizers and Parts
- Chin Straps
- Tubing & Adapters
- Tube Covers
- CPAP Pillows
- Hose Management
- CPAP Travel Accessories
- Protector Mat
- Medistrom Pilot 24 and Pilot 12 Battery
- BPS Freedom CPAP Battery
- ResMed Power Solutions
- Respironics Power Solutions
- Transcend Power Solutions
- CPAP Comparison
- BiPAP Comparison
- Mask Comparison
- Portable Oxygen Comparison
- Stationary Oxygen Comparison
- ResMed Products & Downloads
- Respironics Products & Downloads
- Fisher & Paykel Products & Downloads
- Invacare Concentrators Downloads
- DeVilbiss User Guides
- Oxygen Concentrator Brochures
- Contact Info & FAQ
- Prescriptions
- Medicare & Insurance
- Warranty Info
- CPAP Cleaning Instructions
- Shipping Information
- Customer Comments
- Notice of Privacy Practices

Common hcpcs codes for sleep therapy and oxygen equipment & supplies
Although Sleep Restfully, Inc does not file claims with your insurance company for reimbursement many insurance companies will consider claims filed directly by the insured party. These claims must contain the appropriate HCPCS code in order to be considered. In an effort to assist out customers in filing a claim we are providing a list of the most common HCPCS codes used for sleep therapy and oxygen therapy equipment and supplies.
CPAP/BiLevel Michine HCPCS Codes:
E0601 Continuous airway pressure device (CPAP/APAP)
E0470 Respiratory assist device, bi-level pressure capability, without backup rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pressure device)
E0471 Respiratory assist device, bi-level pressure capability, with back-up rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pressure device)
E0472 Respiratory assist device, bi-level pressure capability, with backup rate feature, used with invasive interface, e.g., tracheostomy tube (intermittent assist device with continuous positive airway pressure device)
E0571 Humidifier, non-heated, used with positive airway pressure device
E0562 Humidifier, heated, used with positive airway pressure device
CPAP/Bi-Level Mask HCPCS Codes
A7030 Full face mask used with positive airway pressure device, each
A7034 Nasal interface (mask or cannula type) used with positive airway pressure device, with or without head strap
A7044 Oral interface used with positive airway pressure device
A7027 Combination oral/nasal mask, used with continuous positive airway pressure device, each
CPAP & Bi-Level Parts and Accessories
A4604 Heated Tube used with Positive airway pressure device
A7028 Oral cushion for combination oral/nasal mask, replacement only, each
A7029 Nasal pillows for combination oral/nasal mask, replacement only, pair
A7031 Face mask interface, replacement for full face mask, each
A7032 Cushion for use on nasal mask interface, replacement only, each
A7033 Pillow for use on nasal cannula type interface, replacement only, pair
A7035 Headgear used with positive airway pressure device
A7036 Chinstrap used with positive airway pressure device
A7037 Tubing used with positive airway pressure device
A7038 Filter, disposable, used with positive airway pressure device
A7039 Filter, non disposable, used with positive airway pressure device
A7045 Exhalation port with or without swivel used with accessories for positive airway devices, replacement only
A7046 Water chamber for humidifier, used with positive airway pressure device, replacement, each
Oxygen Concentrators & Supplies
A4615 Oxygen Nasal Cannula
A4616 Oxygen Supply Tubing
E0445 Oximeter device for measuring blood oxygen levels non-invasively
E1356 Oxygen accessory, battery pack/cartridge for portable concentrator, any type, replacement only, each
E1357 Oxygen accessory, battery charger for portable concentrator, any type, replacement only, each
E1358 Oxygen accessory, dc power adapter for portable concentrator, any type, replacement only, each
E1390 Oxygen concentrator, single delivery port, capable of delivering 85 percent or greater oxygen concentration at the prescribed flow rate
E1392 Portable oxygen concentrator
Miscellaneous Medical Equipment
E1399 Durable medical equipment, miscellaneous

Sleep Restfully, Inc. 3100 Weslayan Street, Suite 373 Houston, TX 77027 (866) 923-2727 (281) 840-4504 Fax:(800) 540-5078 (281) 501-7969
Sign up to our mailing list
Customer Services
- How to Contact Us & FAQ
- Returns Policy & Terms
- Warranty Information
- Insurance Information
- Insurance Billing Codes
- Privacy Information
- Prescriptions Policy
- SleepRestfully Blog
- Make a Payment
Quick Links
- ResMed CPAP
- Philips Respironics CPAP
- ResMed CPAP Mask
- Philips Respironics CPAP Mask
- SimplyGo Mini and SimplyGo
- Build-A-Mask Program/
- CPAP Mask Comparison Chart
- CPAP Machine Comparison Chart
- BiPAP & VPAP Comparison Chart
- Portable Oxygen Concentrator Comparison Chart
- Oxygen Concentrator Comparison Chart
- CPAP Machines & Supplies
- Portable Oxygen Concentrators & Supplies
Sleep Restfully, Inc. 3100 Weslayan Street, Suite 373 Houston, TX 77027 Toll Free: (866) 923-2727 International: (281) 840-4504 Toll Free Fax: (800) 540-5078 International Fax: (281) 501-7969

Financing Available
Get the Equipment you want now and pay over time with Bread*
Affordable Monthly Payments
Pay over 24 months at competive rates, or pay over 6 months at a low 0% APR**. No prepayment penalties.
Fast and Easy Online Application
Click on "Apply With Bread" to go to Bread's web page.
***Subject to approval of credit application. Rates range from 0% to 29.99% APR, resulting in, for example, 24 monthly payments of $46.14 at 9.99% APR, per $1,000 borrowed. APRs will vary depending on credit qualifications, loan amount, and term. Bread® pay-over-time plans are loans made by Comenity Capital Bank

What Are HCPCS Codes For CPAP?
Jan 16, 2023
Share this article
Every medical supply or management services has an associated billing code or HCPCS code. HCPCS (Healthcare Common Procedure Coding System), which is essentially the same as CPT (Current Procedural Terminology) codes, are used by government healthcare providers. “billing codes” are often used to describe the CPT or HCPCS codes.
Health insurers in the US handle more than 5 billion claims for payment each year. Standardized coding methods are necessary for Medicare and other health insurance plans to guarantee that these claims are handled orderly and uniformly. One of the standard code sets is the HCPCS Code Set.
Discover below the specific HCPCS codes we created for the goods and services provided in health care delivery.
HCPCS Reference Codes For CPAP And Respiratory Equipment
HCPCS reference codes serve to identify medical services and supplies for billing. The usage of CPAP (Continuous Positive Airway Pressure) and respiratory-related equipment is associated with unique codes known as HCPCS reference codes for CPAP and respiratory equipment. These codes are used to charge for the CPAP for obstructive sleep apnea and other sleep disorders and respiratory treatment-related equipment, services, and supplies.
When filing claims to insurance companies for payment of services and supplies associated with the use of these therapies, medical professionals utilize them. For timely and correct invoicing of services and supplies related to CPAP and respiratory treatments, HCPCS reference codes for CPAP and respiratory equipment are required.
HCPCS Codes For BiPAP/CPAP Machine Coverage
Below is the list of HCPCS codes For BiPAP/ CPAP Machine Coverage
HCPCS CODE: E0601
Equipment for continuous airway pressure (APAP/CPAP)
HCPCS CODE: E0470
Bi-level positive airway pressure (BiPAP) capable respiratory assist device, without backup rate feature, utilized with a non-invasive interface, such as a nasal or facial mask (intermittent assist device with continuous positive airway pressure (CPAP) device)
HCPCS CODE: E0471
Intermittent support equipment with continuous positive airway pressure devices, respiratory assist device with bi-level positive airway pressure (BiPAP) capacity, WITH backup rate function, utilized with a noninvasive interface, such as a nasal or facial mask
HCPCS CODE: E0472
When utilized with an invasive interface, such as a tracheostomy tube, a respiratory aid device with bi-level positive airway pressure (BiPAP) capabilities, WITH a backup rate function, is employed.
HCPCS CODE: E0561
When used with positive airway pressure (CPAP, BiPAP, APAP) equipment, a non-heated humidifier
HCPCS CODE: E0562
A heated humidifier is employed with positive airway pressure (BiPAP, APAP, CPAP) equipment.
HCPCS Codes For BiPAP/CPAP Mask Coverage
Below are the list of HCPCS codes For BiPAP/ CPAP Mask Coverage
HCPCS CODE: A7030
Positive Airway Pressure (BiPAP, APAP, CPAP) equipment with a Full Face Mask
HCPCS CODE: A7034
With or without a head strap, a nasal interface (mask or cannula type) is used with positive airway pressure (CPAP/BiPAP/APAP) equipment.
HCPCS CODE: A7044
Oral interface for positive airway pressure (CPAP, BiPAP, APAP) equipment
HCPCS CODE: A7027
Combining oral/nasal mask used in conjunction with continuous positive airway pressure device.
Part & Accessory Insurance For BiPAP/CPAP (HCPCS) Codes
Below is the list of HCPCS codes For BiPAP/CPAP (HCPCS) Codes
HCPCS CODE: A7028
Oral Cushion Replacement for Oral/Nasal Mask Combination
HCPCS CODE: A7029
Nasal Pillow Cushion Replacement for Oral and Nasal Mask
HCPCS CODE: A7031
An additional cushion for a full-face mask
HCPCS CODE: A7032
Nasal mask cushion replacement
HCPCS CODE: A7033
Replacement Pillows for Cannula Style Mask or Nasal Pillows
HCPCS CODE: A7035
Headgear used with a positive pressure ventilation system
HCPCS CODE: A7036
Chinstraps work in tandem with positive airway pressure apparatus.
HCPCS CODE: A7037
Tubing used in conjunction with a positive airway pressure equipment
HCPCS CODE: A4604
With a positive airway pressure device, heated tubing is utilized.
HCPCS CODE: A7038
Disposable filter used in conjunction with a positive airway pressure equipment
HCPCS CODE: A7039
Filter used in conjunction with a positive airway pressure device that is not disposable
HCPCS CODE: A7045
Positive airway pressure device attachments may include an exhalation port with or without a swivel.
HCPCS CODE: A7046
Use of a humidifier’s water chamber with a positive pressure ventilation system
HCPCS CODE: E1399
Items, Components, and Accessories of Various Durable Medical Equipment
HCPCS Codes For Nebulizer And Compressor Coverage
Below is the list of HCPCS codes For Nebulizer And Compressor Coverage
HCPCS CODE: E0570
Combined compressor and nebulizer
HCPCS CODE: A7005
Non-disposable administration equipment with a small capacity, nonfiltered pneumatic nebulizer
HCPCS CODE: A7004
Disposable small-volume nonfiltered pneumatic nebulizer
HCPCS CODE: A7003
Disposable administration set with a small-volume, nonfiltered pneumatic nebulizer
HCPCS CODE: A7015
Using an aerosol mask with a DME nebulizer
HCPCS CODE: A7014
Non-disposable filter used with an ultrasonic generator or an aerosol compressor
HCPCS CODE: A7013
Disposable filter for use with an ultrasonic generator or an aerosol compressor
HCPCS CODE: A4627
Chamber for use with metered dose inhaler, with or without a mask
HCPCS Codes For Light Therapy Equipment Coverage
Below is the list of HCPCS code For Light Therapy Equipment Coverage
HCPCS CODE: E0203
Device for light treatment
HCPCS Codes For Oxygen Concentrators & Supplies Coverage
Below is the list of HCPCS codes For Oxygen Concentrators & Supplies Coverage
HCPCS CODE: E1356
Battery pack and an oxygen attachment
HCPCS CODE: E1357
Accessory for oxygenation, battery charger
HCPCS CODE: E1358
Accessory for oxygen, DC power adapter
HCPCS CODE: E1390
Single-port oxygen concentrators can supply 85 percent or greater oxygen concentration at the specified flow rate.
HCPCS CODE: E1392
Oxygen concentrator that is accessible
HCPCS CODE: E0445
Oximeter for non-invasively monitoring blood oxygen levels
HCPCS CODE: A4615
Nasal Oxygen Cannula
HCPCS CODE: A4616
Supply tubes for oxygen
These codes are solely for reference; you should confirm their correctness with your insurer. Rules and processes for filing successful claims vary across insurers. Please get in touch with your healthcare provider to determine the steps you need to take to make a successful claim. Visit the Centers for Medicare & Medicaid Services to learn more about HCPCS codes. If you want to learn about ICD codes, you can visit the World Health Organization.
What did you learn in today`s article? Share your thoughts below!
Featured Posts

CPAP Distilled Water: Breakdown of Cost When Buying Online
Distilled Water , Featured
You will consider several key factors when shopping for CPAP distilled water online. One of the most important considerations is the shipping fee. As Amazon is one of the world’s largest online retailers, we will use it as our example in this article of the...

CPAP Distilled Water: How Much Does It Cost?
What is the cost of CPAP distilled water? If you've been considering purchasing distilled water for your continuous positive airway pressure machine, you're probably wondering how much it will cost. Most people think that distilled water is expensive and that...

What Type of Water Should I Use in My CPAP Machine?
If you suffer from sleep apnea, you probably use a CPAP Machine. It is a wonderful invention to ensure you get a safe, peaceful sleep. Knowing the many types of water available and what you should use with your CPAP machine is essential. When it comes to utilizing...
Recent Posts
Sleep apnea in women: breaking the stereotypes with cpap, balancing asthma and sleep apnea: the role of cpap water, the relationship helper: how cpap can save your sleep and love life, debunking sleep apnea myths: how effective is cpap therapy really, cpap and seasonal allergies: tips for a better night’s sleep.
- Skip to Content
- Skip to Navigation

Welcome Logout
- TRICARE West
- Page Not Found
Sorry, the requested page was not found
You may wish to try one of the following:
- Use the navigation at the top of this page to browse to the page in question.
- Use the search box at the top of this page to search for the page in question.
- Use the links in the boxes on the left of this page to browse to the page in question.
- Use one of the links at the bottom of this page to browse to the page in question.
Error type: 404 (Page not found)
- Go To --Portal-- Beneficiary Provider Government
TRICARE is a registered trademark of the Department of Defense, Defense Health Agency. All rights reserved.

FREE SHIPPING on Orders Over $49!
Insurance Codes
CPAP Network does not bill any insurance, Medicare or Medicaid. We are a free-market provider which allows us to offer the most cost-effective options to people with high deductibles. If you have a high deductible health plan, you are basically self-insured until your deductible is met. This is where smart out-of-pocket purchasing can be the most economical and hassle-free.
If you choose to submit an insurance claim form for reimbursement, CPAP Network will assist by providing a detailed purchase order with all the required data. Below are the HCPCS codes you may need for the claim form:
HCPCS CODES
CPAP/BiPAP MACHINE
E0601 - Continuous airway pressure (CPAP/APAP) device
E0470 - Respiratory assist device, bi-level pressure (BiPAP) capability, WITHOUT backup rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pressure device)
E0471 - Respiratory assist device, bi-level pressure (BiPAP) capability, WITH backup rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pressure device)
E0472 - Respiratory assist device, bi-level pressure (BiPAP) capability, WITH backup rate feature, used with invasive interface, e.g., tracheostomy tube (intermittent assist device with continuous positive airway pressure device)
E0561 - Humidifier, non-heated, used with positive airway pressure (CPAP/BiPAP/APAP) device
E0562 - Humidifier, heated, used with positive airway pressure (CPAP/BiPAP/APAP) device
CPAP/BiPAP MASK
A7030 - Full Face Mask used with Positive Airway Pressure (CPAP/BiPAP/APAP) Device
A7034 - Nasal interface (mask or cannula type) used with positive airway pressure (CPAP/BiPAP/APAP) device , with or without headstrap
A7044 - Oral interface used with positive airway pressure (CPAP/BiPAP/APAP) device
A7027 - Combination oral/nasal mask, used with continuous positive airway pressure device
CPAP/BiPAP PARTS & ACCESSORIES
A7028 - Oral cushion for combination oral/nasal mask
A7029 - Nasal pillows for combination oral/nasal mask
A7031 - Replacement Cushion for Full Face Mask
A7032 - Replacement Cushion for Nasal Mask
A7033 - Replacement Pillows for Nasal Mask
A7035 - Headgear used with positive airway pressure device
A7036 - Chinstrap used with positive airway pressure device
A7037 - Tubing used with positive airway pressure device
A4604 - Heated Tubing used with positive airway pressure device
A7038 - Filter, disposable, used with positive airway pressure device
A7039 - Filter, non-disposable (reusable), used with positive airway presssure device
A7045 - Exhalation port with or without swivel used with accessories for positive airway pressure devices
A7046 - Water chamber for humidifier, used with positive airway pressure device
E1399 - Miscellaneous Durable Medical Equipment Items, Components and Accessories
( CPT is a code set to describe medical, surgical ,and diagnostic services; HCPCS are codes based on the CPT to provide standardized coding when healthcare is delivered)
OTHER INFO:
Provider Diagnosis Code
Diagnosis code for Obstructive Sleep Apnea is G47.33 (contact your provider for your specific diagnosis code) Our Company Information Most frequently requested information: CPAP Network LLC 1437 Egg Harbor Road Sturgeon Bay, WI 54235 Phone: 888.293.4811 Fax: 920.367.0533 Tax ID Number: 82-5030164
(650) 517-9495

CPAP Billing Codes
Sign up to receive product updates and coupons.
Subscribe to receive member-only discounts, special offers, product updates and recall notifications.
If you are a new customer and would
like to pay with cash
to CONTINUE >>
If you are an existing SleepQuest customer
to REORDER SUPPLIES VIA INSURANCE or
click here
to PAY YOUR BILL
You are leaving shop.sleequest.com to go to an independent physician’s website to schedule an appointment for professional medical services. Healthcare regulations prohibit SleepQuest from employing physicians. We only offer this physician referral as a convenience to you. You may use this physician’s service or another of your own choosing.
Age verification
By clicking enter you are verifying that you are old enough to consume alcohol.
Shopping Cart
Your cart is currently empty..

HCPCS Code E0601 | Description & Billing Guidelines
Report E0601 when a provider uses a CPAP (Continuous Positive Airway Pressure) device to maintain airflow through the throat of a patient with obstructive sleep apnea.
What Is E0601?
HCPCS code E0601 represents the continuous positive airway pressure supply or CPAP device.
This machine maintains pressurized air flowing through the airways of the throat to keep it open in a patient with
This device that a provider most commonly uses for the treatment of a patient with sleep apnea, a sleep disorder where the walls of the patient’s throat relax and narrow, and the tongue falls back against the soft palate during sleep causing cessation of breathing.
The patient wears a face or nasal mask during sleep. This mask connects to a pump that delivers a positive current of air through the nose to maintain an open airway.
Description
E0601 is officially described by HCPCS. The description of this code can be found below.
Short Description: “Cont airway pressure device.”
Long Description: “Continuous positive airway pressure (CPAP) device.”
Pricing Indicator: 36
Code Added: January 01, 1988
Last Changed : January 01, 2014
Billing Guidelines
Special coverage instructions may apply for E0601.
Similar Posts
How to use hcpcs code g9497.
HCPCS code G9497 describes the instruction received from the anesthesiologist or proxy prior to the day of surgery to abstain from smoking on the day of surgery. This code is used to indicate that the patient has been advised to refrain from smoking on the day of their surgical procedure. 1. What is HCPCS G9497?…
How To Use HCPCS Code C9082
HCPCS code C9082 describes the injection of dostarlimab-gxly, 100 mg. This code is used to identify the administration of this specific medication in a parenteral form. In this article, we will explore the details of HCPCS code C9082, including its official description, procedure, when to use it, billing guidelines, historical information, Medicare and insurance coverage,…
How To Use HCPCS Code E1036
HCPCS code E1036 describes a multi-positional patient transfer system that is extra-wide and includes an integrated seat. This system is operated by a caregiver and has a patient weight capacity greater than 300 lbs. It falls under the category of enteral supplies not otherwise classified. 1. What is HCPCS E1036? HCPCS code E1036 is used…
How To Use HCPCS Code G8810
HCPCS code G8810 describes the use of Rh-immunoglobulin (RhoGAM) not being ordered for reasons documented by the clinician. This code is used when a patient has a documented receipt of RhoGAM within the past 12 weeks or when the patient refuses to receive the medication. It is important for medical coders to understand the specific…

How To Use HCPCS Code G0457
HCPCS code G0457 describes the procedure of negative pressure wound therapy using a mechanically-powered device, not durable medical equipment, for wounds with a total surface area greater than 50 square centimeters. This code includes the provision of cartridge and dressing(s), topical application(s), wound assessment, and instructions for ongoing care, per session. In this article, we…
How To Use HCPCS Code E0730
HCPCS code E0730 describes a transcutaneous electrical nerve stimulation (TENS) device with four or more leads, specifically designed for multiple nerve stimulation. This code is used to identify and bill for the use of this device in medical procedures and treatments. In this article, we will explore the details of HCPCS code E0730, including its…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
The page could not be loaded. The CMS.gov Web site currently does not fully support browsers with "JavaScript" disabled. Please enable "JavaScript" and revisit this page or proceed with browsing CMS.gov with "JavaScript" disabled. Instructions for enabling "JavaScript" can be found here. Please note that if you choose to continue without enabling "JavaScript" certain functionalities on this website may not be available.

An official website of the United States government
Here's how you know
The .gov means it's official.
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure.
The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Tracking Sheet
Positive airway pressure (pap) devices for the treatment of obstructive sleep apnea, document note, note history, contractor information, lcd information, document information.
CPT codes, descriptions and other data only are copyright 2023 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.
Current Dental Terminology © 2023 American Dental Association. All rights reserved.
Copyright © 2023 , the American Hospital Association, Chicago, Illinois. Reproduced with permission. No portion of the American Hospital Association (AHA) copyrighted materials contained within this publication may be copied without the express written consent of the AHA. AHA copyrighted materials including the UB‐04 codes and descriptions may not be removed, copied, or utilized within any software, product, service, solution or derivative work without the written consent of the AHA. If an entity wishes to utilize any AHA materials, please contact the AHA at 312‐893‐6816.
Making copies or utilizing the content of the UB‐04 Manual, including the codes and/or descriptions, for internal purposes, resale and/or to be used in any product or publication; creating any modified or derivative work of the UB‐04 Manual and/or codes and descriptions; and/or making any commercial use of UB‐04 Manual or any portion thereof, including the codes and/or descriptions, is only authorized with an express license from the American Hospital Association. The American Hospital Association (the "AHA") has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
The LCD is revised to align refill requirements with CMS Final Rule CMS-1780-F. This revision allows contact with the beneficiary regarding refills to take place no sooner than 30 calendar days prior to the end of the current supply and to document an affirmative response.
No proposed LCD issued.
CMS National Coverage Policy
CMS Pub. 100.03 (Medicare National Coverage Determination Manual), Chapter 1, Section 240.4
Coverage Guidance
For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements. The purpose of a Local Coverage Determination (LCD) is to provide information regarding “reasonable and necessary” criteria based on Social Security Act § 1862(a)(1)(A) provisions. In addition to the “reasonable and necessary” criteria contained in this LCD there are other payment rules, which are discussed in the following documents, that must also be met prior to Medicare reimbursement:
The LCD-related Standard Documentation Requirements Article, located at the bottom of this policy under the Related Local Coverage Documents section.
The LCD-related Policy Article, located at the bottom of this policy under the Related Local Coverage Documents section.
Refer to the Supplier Manual for additional information on documentation requirements.
Refer to the DME MAC web sites for additional bulletin articles and other publications related to this LCD.
For the items addressed in this LCD, the “reasonable and necessary” criteria, based on Social Security Act § 1862(a)(1)(A) provisions, are defined by the following coverage indications, limitations and/or medical necessity. DEFINITIONS: Apnea is defined as the cessation of airflow for at least 10 seconds. Hypopnea is defined as an abnormal respiratory event lasting at least 10 seconds associated with at least a 30% reduction in thoracoabdominal movement or airflow as compared to baseline, and with at least a 4% decrease in oxygen saturation. The apnea-hypopnea index (AHI) is defined as the average number of episodes of apnea and hypopnea per hour of sleep without the use of a positive airway pressure device. For purposes of this policy, respiratory effort related arousals (RERAs) are not included in the calculation of the AHI. Sleep time can only be measured in a Type I (facility based polysomnogram) or Type II sleep study (see descriptions below). The respiratory disturbance index (RDI) is defined as the average number of apneas plus hypopneas per hour of recording without the use of a positive airway pressure device. For purposes of this policy, respiratory effort related arousals (RERAs) are not included in the calculation of the RDI. The RDI is reported in Type III, Type IV, and other home sleep studies. If the AHI or RDI is calculated based on less than 2 hours of sleep or recording time, the total number of recorded events used to calculate the AHI or RDI (respectively) must be at least the number of events that would have been required in a 2 hour period (i.e., must reach ≥30 events without symptoms or ≥10 events with symptoms). INITIAL COVERAGE:
In this policy, the term PAP (positive airway pressure) device will refer to both a single-level continuous positive airway pressure device (E0601) and a bi-level respiratory assist device without back-up rate (E0470) when it is used in the treatment of obstructive sleep apnea.
- An E0601 device is covered for the treatment of obstructive sleep apnea (OSA) if criteria A – C are met:
- The beneficiary has an in-person clinical evaluation by the treating practitioner prior to the sleep test to assess the beneficiary for obstructive sleep apnea.
- The beneficiary has a sleep test (as defined below) that meets either of the following criteria (1 or 2):
- The apnea-hypopnea index (AHI) or Respiratory Disturbance Index (RDI) is greater than or equal to 15 events per hour with a minimum of 30 events; or,
- The AHI or RDI is greater than or equal to 5 and less than or equal to 14 events per hour with a minimum of 10 events and documentation of:
- Excessive daytime sleepiness, impaired cognition, mood disorders, or insomnia; or,
- Hypertension, ischemic heart disease, or history of stroke.
- The beneficiary and/or their caregiver has received instruction from the supplier of the device in the proper use and care of the equipment.
If a claim for an E0601 is submitted and all of the criteria above have not been met, it will be denied as not reasonable and necessary.
- An E0470 device is covered for those beneficiaries with OSA who meet criteria A-C above, in addition to criterion D:
- An E0601 has been tried and proven ineffective based on a therapeutic trial conducted in either a facility or in a home setting.
Ineffective is defined as documented failure to meet therapeutic goals using an E0601 during the titration portion of a facility-based study or during home use despite optimal therapy (i.e., proper mask selection and fitting and appropriate pressure settings). If E0470 is billed for a beneficiary with OSA and criteria A-D are not met, it will be denied as not reasonable and necessary. A bi-level positive airway pressure device with back-up rate (E0471) is not reasonable and necessary if the primary diagnosis is OSA. If an E0471 is billed with a diagnosis of OSA, it will be denied as not reasonable and necessary. If an E0601 device is tried and found ineffective during the initial facility-based titration or home trial, substitution of an E0470 does not require a new initial in-person clinical evaluation or a new sleep test. If an E0601 device has been used for more than 3 months and the beneficiary is switched to an E0470, a new initial in-person clinical evaluation is required, but a new sleep test is not required. A new 3 month trial would begin for use of the E0470. Coverage, coding and documentation requirements for the use of E0470 and E0471 for diagnoses other than OSA are addressed in the Respiratory Assist Devices (RAD) Local Coverage Determination (LCD) and related Policy Article (PA). Sleep Tests
Coverage and Payment rules for diagnostic sleep tests may be found in the CMS National Coverage Determination (NCD) 240.4.1 (CMS Pub.100-03, Chapter 1, Part 4), the applicable A/B MAC LCDs and Billing and Coding articles. The sleep test must be either a polysomnogram performed in a facility-based laboratory (Type I study) or an inpatient hospital-based or home-based sleep test (HST) (Types II, III, IV, Other).
Coverage of a PAP device for the treatment of OSA is limited to claims where the diagnosis of OSA is based upon all of the following:
A sleep test (Type I, II, III, IV, Other) that meets the Medicare requirements for a valid sleep test as outlined in NCD 240.4.1 and the applicable A/B MAC LCD and Billing and Coding article; and,
A sleep test that is approved by the Food and Drug Administration (FDA) as a diagnostic device; and,
The sleep test results meet the coverage criteria in effect for the date of service of the claim for the PAP device; and,
The sleep test is ordered by the beneficiary’s treating practitioner; and,
- The sleep test is conducted by an entity that qualifies as a Medicare provider of sleep tests and is in compliance with all applicable state regulatory requirements.
CONTINUED COVERAGE BEYOND THE FIRST THREE MONTHS OF THERAPY:
Continued coverage of a PAP device (E0470 or E0601) beyond the first three months of therapy requires that, no sooner than the 31st day but no later than the 91st day after initiating therapy, the treating practitioner must conduct a clinical re-evaluation and document that the beneficiary is benefiting from PAP therapy.
For PAP devices with initial dates of service on or after November 1, 2008, documentation of clinical benefit is demonstrated by:
1. In-person clinical re-evaluation by the treating practitioner with documentation that symptoms of obstructive sleep apnea are improved; and,
2. Objective evidence of adherence to use of the PAP device, reviewed by the treating practitioner.
Adherence to therapy is defined as use of PAP ≥4 hours per night on 70% of nights during a consecutive thirty (30) day period anytime during the first three (3) months of initial usage. If the above criteria are not met, continued coverage of a PAP device and related accessories will be denied as not reasonable and necessary. If the treating practitioner re-evaluation does not occur until after the 91st day but the evaluation demonstrates that the beneficiary is benefiting from PAP therapy as defined in criteria 1 and 2 above, continued coverage of the PAP device will commence with the date of that re-evaluation.
Beneficiaries who fail the initial 12 week trial are eligible to re-qualify for a PAP device but must have both:
- In-person clinical re-evaluation by the treating practitioner to determine the etiology of the failure to respond to PAP therapy; and,
- Repeat sleep test in a facility-based setting (Type 1 study). This may be a repeat diagnostic, titration or split-night study.
If an E0601 device is tried and found ineffective during the initial facility-based titration or home trial, substitution of an E0470 does not change the length of the trial unless there is less than 30 days remaining in the trial period. If more than 30 days remain in the trial period, the clinical re-evaluation would still occur between the 31st and 91st day following the initiation of an E0601 and objective documentation of adherence on the E0470 would need to occur prior to the 91st day following initiation of the E0601. If less than 30 days remain in the trial period, the clinical re-evaluation and objective documentation of adherence must occur before the 120th day following the initiation of the E0601.
If an E0601 device was used for more than 3 months and the beneficiary was then switched to an E0470, the clinical re-evaluation must occur between the 31st and 91st day following the initiation of the E0470. There would also need to be documentation of adherence to therapy during the 3 month trial with the E0470. If there is discontinuation of usage of a PAP device at any time, the supplier is expected to ascertain this and stop billing for the equipment and related accessories and supplies. For a PAP device dispensed prior to November 1, 2008, if the initial Medicare coverage criteria in effect at the time were met and the criteria for coverage after the first 3 months that were in effect at the time were met, the device will continue to be covered for dates of service on or after November 1, 2008 as long as the beneficiary continues to use the device. CONCURRENT USE OF OXYGEN WITH PAP THERAPY: Some beneficiaries may require the simultaneous use of home oxygen therapy and oxygen equipment with a PAP device. To be considered for simultaneous coverage, all requirements in the "Coverage Indications, Limitations and/or Medical Necessity" sections of both the Oxygen and Oxygen Equipment and Positive Airway Pressure (PAP) Devices for the Treatment of Obstructive Sleep Apnea LCDs must be met. Consequently, in addition to this LCD, suppliers should refer to the Oxygen and Oxygen Equipment LCD and related Policy Article for additional coverage, coding and documentation requirements. For beneficiaries with OSA to be considered for oxygen therapy and oxygen equipment, the OSA must be sufficiently treated such that the underlying condition resulting in hypoxemia is unmasked. This must be demonstrated before oxygen saturation results obtained during polysomnography are considered qualifying for oxygen therapy and oxygen equipment.
For beneficiaries with OSA, a qualifying oxygen saturation test for the purposes of Medicare home oxygen and oxygen equipment reimbursement may only occur during a titration polysomnographic study (either split-night or stand-alone). The titration PSG is one in which all of the following criteria are met:
1. The titration is conducted over a minimum of two (2) hours; and,
2. During titration:
A. The AHI/RDI is reduced to less than or equal to an average of ten (10) events per hour; or,
B. If the initial AHI/RDI was less than an average of ten (10) events per hour, the titration demonstrates further reduction in the AHI/RDI; and,
- Nocturnal oximetry conducted for the purpose of oxygen and oxygen equipment reimbursement qualification may only be performed after optimal PAP settings have been determined and the beneficiary is using the PAP device at those settings; and,
- The nocturnal oximetry conducted during the PSG demonstrates an oxygen saturation of ≤ 88%.
To be eligible for Medicare coverage and payment for home oxygen therapy and oxygen equipment for concurrent use with PAP therapy, the beneficiary must meet all other coverage requirements for oxygen therapy and oxygen equipment. Beneficiaries that qualify for oxygen therapy based on testing conducted only during the course of a sleep test are eligible only for reimbursement of stationary equipment.
Overnight oximetry performed as part of home sleep testing or as part of any other home testing is not considered as eligible to be used for qualification for reimbursement of home oxygen and oxygen equipment (see the "Overnight Oximetry Studies" section of the Oxygen and Oxygen Equipment LCD for additional information).
REPLACEMENT: This section applies to PAP devices initially provided and covered while the beneficiary was in Medicare fee-for-service (FFS). If a PAP device is replaced during the 5 year reasonable useful lifetime (RUL) because of loss, theft, or irreparable damage due to a specific incident, there is no requirement for a new clinical evaluation, sleep test, or trial period. If a PAP device is replaced following the 5 year RUL, there must be an in-person evaluation by their treating practitioner that documents that the beneficiary continues to use and benefit from the PAP device. There is no requirement for a new sleep test or trial period.
BENEFICIARIES ENTERING MEDICARE:
For beneficiaries who received a PAP device prior to enrollment in fee for service (FFS) Medicare and are seeking Medicare coverage of either rental of the device, a replacement PAP device and/or accessories, both of the following coverage requirements must be met:
- Sleep test - There must be documentation that the beneficiary had a sleep test, prior to FFS Medicare enrollment, that meets the Medicare AHI/RDI coverage criteria in effect at the time that the beneficiary seeks Medicare coverage of a replacement PAP device and/or accessories; and,
- Clinical Evaluation - Following enrollment in FFS Medicare, the beneficiary must have an in-person evaluation by their treating practitioner who documents in the beneficiary’s medical record that:
A. The beneficiary has a diagnosis of obstructive sleep apnea; and,
B. The beneficiary continues to use the PAP device.
If either criteria 1 or 2 above are not met, the claim will be denied as not reasonable and necessary. In these situations, there is no requirement for a clinical re-evaluation or for objective documentation of adherence to use of the device.
ACCESSORIES: Accessories used with a PAP device are covered when the coverage criteria for the device are met. If the coverage criteria are not met, the accessories will be denied as not reasonable and necessary. The following table represents the usual maximum amount of accessories expected to be reasonable and necessary:
Quantities of supplies greater than those described in the policy as the usual maximum amounts will be denied as not reasonable and necessary. GENERAL
A Standard Written Order (SWO) must be communicated to the supplier before a claim is submitted. If the supplier bills for an item addressed in this policy without first receiving a completed SWO, the claim shall be denied as not reasonable and necessary.
For Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) base items that require a Written Order Prior to Delivery (WOPD), the supplier must have received a signed SWO before the DMEPOS item is delivered to a beneficiary. If a supplier delivers a DMEPOS item without first receiving a WOPD, the claim shall be denied as not reasonable and necessary. Refer to the LCD-related Policy Article, located at the bottom of this policy under the Related Local Coverage Documents section.
For DMEPOS base items that require a WOPD, and also require separately billed associated options, accessories, and/or supplies, the supplier must have received a WOPD which lists the base item and which may list all the associated options, accessories, and/or supplies that are separately billed prior to the delivery of the items. In this scenario, if the supplier separately bills for associated options, accessories, and/or supplies without first receiving a completed and signed WOPD of the base item prior to delivery, the claim(s) shall be denied as not reasonable and necessary.
An item/service is correctly coded when it meets all the coding guidelines listed in CMS HCPCS guidelines, LCDs, LCD-related Policy Articles, or DME MAC articles. Claims that do not meet coding guidelines shall be denied as not reasonable and necessary/incorrectly coded.
Proof of delivery (POD) is a Supplier Standard and DMEPOS suppliers are required to maintain POD documentation in their files. Proof of delivery documentation must be made available to the Medicare contractor upon request. All services that do not have appropriate proof of delivery from the supplier shall be denied as not reasonable and necessary.
REFILL REQUIREMENTS For DMEPOS items and supplies provided on a recurring basis, billing must be based on prospective, not retrospective use. For DMEPOS products (A4604, A7027 , A7028, A7029, A7030, A7031, A7032, A7033, A7034, A7035, A7036, A7037, A7038, A7039, A7044, A7045, A7046) that are supplied as refills to the original order, suppliers must contact the beneficiary , and document an affirmative response, prior to dispensing the refill and not automatically ship on a pre-determined basis, even if authorized by the beneficiary. This shall be done to ensure that the refilled item remains reasonable and necessary, existing supplies are expected to end, and to confirm any changes or modifications to the order. Contact with the beneficiary or designee regarding refills must take place no sooner than 30 calendar days prior to the expected end of the current supply. For delivery of refills, the supplier must deliver the DMEPOS product no sooner than 10 calendar days prior to the expected end of the current supply. This is regardless of which delivery method is utilized. For all DMEPOS items that are provided on a recurring basis, suppliers are required to have contact with the beneficiary or caregiver/designee and document an affirmative response, prior to dispensing a new supply of items. Suppliers must not deliver refills without a refill request and an affirmative response from a beneficiary. Items delivered without a valid, documented refill request will be denied as not reasonable and necessary. Suppliers must not dispense a quantity of supplies exceeding a beneficiary's expected utilization. Suppliers must stay attuned to changed or atypical utilization patterns on the part of their clients. Suppliers must verify with the treating practitioners that any changed or atypical utilization is warranted. Regardless of utilization, a supplier must not dispense more than a three (3) - month quantity at a time. Either a non-heated (E0561) or heated (E0562) humidifier is covered when ordered by the treating practitioner for use with a covered PAP (E0470 or E0601) device.
Proposed Process Information
Coding information, bill type codes, revenue codes, cpt/hcpcs codes.
The appearance of a code in this section does not necessarily indicate coverage. HCPCS MODIFIERS: EY - No physician or other licensed health care provider order for this item or service GA - Waiver of liability statement issued as required by payer policy, individual case GZ - Item or service expected to be denied as not reasonable and necessary KX - Requirements specified in the medical policy have been met HCPCS CODES: EQUIPMENT:
ACCESSORIES
ICD-10-CM Codes that Support Medical Necessity
Icd-10-cm codes that do not support medical necessity, additional icd-10 information, general information.
DOCUMENTATION REQUIREMENTS Section 1833(e) of the Social Security Act precludes payment to any provider of services unless "there has been furnished such information as may be necessary in order to determine the amounts due such provider". It is expected that the beneficiary's medical records will reflect the need for the care provided. The beneficiary's medical records include the treating practitioner's office records, hospital records, nursing home records, home health agency records, records from other healthcare professionals and test reports. This documentation must be available upon request. GENERAL DOCUMENTATION REQUIREMENTS
In order to justify payment for DMEPOS items, suppliers must meet the following requirements:
Medical Record Information (including continued need/use if applicable)
Correct Coding
Proof of Delivery
Refill Documentation
Refer to the LCD-related Standard Documentation Requirements article, located at the bottom of this policy under the Related Local Coverage Documents section for additional information regarding these requirements. Refer to the Supplier Manual for additional information on documentation requirements. Refer to the DME MAC web sites for additional bulletin articles and other publications related to this LCD. POLICY SPECIFIC DOCUMENTATION REQUIREMENTS Items covered in this LCD have additional policy-specific requirements that must be met prior to Medicare reimbursement. Refer to the LCD-related Policy article, located at the bottom of this policy under the Related Local Coverage Documents section for additional information. Miscellaneous Appendices APPENDIX A: EPWORTH SLEEPINESS SCALE How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? This refers to your usual way of life in recent times. Even if you have not done some of these things recently try to work out how they would have affected you. Use the following scale to choose the most appropriate number for each situation: 0 = would never doze or sleep. 1 = slight chance of dozing or sleeping 2 = moderate chance of dozing or sleeping 3 = high chance of dozing or sleeping
0-9 – Average score, normal population Epworth Sleepiness Scale reprinted with permission of the Associated Professional Sleep Societies ( Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-545 ). Utilization Guidelines Refer to Coverage Indications, Limitations, and/or Medical Necessity
Revision History Information
Associated documents.
Read the LCD Disclaimer
Email this document to yourself or someone else
An asterisk ( * ) indicates a required field. This email will be sent from you to the recipient email address(es) you enter. Please do not use this feature to contact CMS. To submit a comment or question to CMS, please use the Feedback/Ask a Question link available at the bottom of every MCD page.
Contractor Detail
Lcd disclaimer, license agreements.
Please review and accept the agreements in order to view Medicare Coverage documents, which may include licensed information and codes.
LICENSE FOR USE OF PHYSICIANS' CURRENT PROCEDURAL TERMINOLOGY, FOURTH EDITION ("CPT")
End User Point and Click Amendment: CPT codes, descriptions and other data only are copyright 2023 American Medical Association. All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the American Medical Association (AMA).
You, your employees and agents are authorized to use CPT only as agreed upon with the AMA internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the AMA, CPT Intellectual Property Services, AMA Plaza 330 N. Wabash Ave., Suite 39300, Chicago, IL 60611-5885. Applications are available at the AMA Web site, http://www.ama-assn.org/go/cpt .
Applicable FARS\DFARS Restrictions Apply to Government Use.
AMA Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
CMS Disclaimer
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT should be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material. Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled "I Accept".
LICENSE FOR USE OF CURRENT DENTAL TERMINOLOGY (CDT TM )
End User License Agreement: These materials contain Current Dental Terminology (CDT TM ), copyright© 2023 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. By clicking below on the button labeled "I accept", you hereby acknowledge that you have read, understood and agreed to all terms and conditions set forth in this agreement.
If you do not agree with all terms and conditions set forth herein, click below on the button labeled "I do not accept" and exit from this computer screen.
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, "you" and "your" refer to you and any organization on behalf of which you are acting.
- Subject to the terms and conditions contained in this Agreement, you, your employees and agents are authorized to use CDT only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
- Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CDT for resale and/or license, transferring copies of CDT to any party not bound by this agreement, creating any modified or derivative work of CDT, or making any commercial use of CDT. License to use CDT for any use not authorized herein must be obtained through the American Dental Association, 211 East Chicago Avenue, Chicago, IL 60611. Applications are available at the American Dental Association web site, http://www.ADA.org .
- Applicable Federal Acquisition Regulation Clauses (FARS)/Department of Defense Federal Acquisition Regulation supplement (DFARS) Restrictions Apply to Government Use. U.S. Government Rights Provisions.
- Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
- ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for software, including any CDT and other content contained therein, is with CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT should be addressed to the ADA. End Users do not act for or on behalf of the CMS. CMS disclaims responsibility for any liability attributable to end user use of the CDT. CMS will not be liable for any claims attributable to any errors, omissions, or other inaccuracies in the information or material covered by this license. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material. The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. If the foregoing terms and conditions are acceptable to you, please indicate your agreement by clicking below on the button labeled "I Accept". If you do not agree to the terms and conditions, you may not access or use software. Instead you must click below on the button labeled "I Do Not Accept" and exit from this computer screen.
LICENSE FOR NATIONAL UNIFORM BILLING COMMITTEE (NUBC)
American hospital association disclaimer.
The American Hospital Association ("the AHA") has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
Page Help for LCD - Positive Airway Pressure (PAP) Devices for the Treatment of Obstructive Sleep Apnea (L33718)
Introduction.
This page displays your requested Local Coverage Determination (LCD). The document is broken into multiple sections. You can use the Contents side panel to help navigate the various sections. A Local Coverage Determination (LCD) is a decision made by a Medicare Administrative Contractor (MAC) on whether a particular service or item is reasonable and necessary, and therefore covered by Medicare within the specific jurisdiction that the MAC oversees. Please note that codes (CPT/HCPCS and ICD-10) have moved from LCDs to Billing & Coding Articles.
More information
MACs are Medicare contractors that develop LCDs and process Medicare claims. MACs develop an LCD when there is no national coverage determination (NCD) or when there is a need to further define an NCD for the specific jurisdiction. LCDs outline how the contractor will review claims to ensure that the services provided meet Medicare coverage requirements. Before an LCD becomes final, the MAC publishes Proposed LCDs, which include a public comment period. LCD document IDs begin with the letter "L" (e.g., L12345). Proposed LCD document IDs begin with the letters "DL" (e.g., DL12345). The guidelines for LCD development are provided in Chapter 13 of the Medicare Program Integrity Manual. The Social Security Act, Sections 1869(f)(2)(B) and 1862(l)(5)(D) define LCDs and provide information on the process
The LCD Tracking Sheet is a pop-up modal that is displayed on top of any Proposed LCD that began to appear on the MCD on or after 1/1/2022. The Tracking Sheet provides key details about the Proposed LCD, including a summary of the issue, who requested the new/updated policy, links to key documents, important process-related dates, who to contact with questions about the policy, and the history of previous policy considerations. The information displayed in the Tracking Sheet is pulled from the accompanying Proposed LCD and its correlating Final LCD and will be updated as new data becomes available. The Tracking Sheet modal can be closed and re-opened when viewing a Proposed LCD.
Printing a Document to PDF
Frequently Asked Questions (FAQs)
Are you a provider and have a question about billing or coding.
Please contact your Medicare Administrative Contractor (MAC). MACs can be found in the MAC Contacts Report .
Do you have questions related to the content of a specific Local Coverage Determination (LCD) or an Article?
Are you a beneficiary and have questions about your coverage, are you looking for codes (e.g., cpt/hcpcs, icd-10), local coverage.
For the most part, codes are no longer included in the LCD (policy). You will find them in the Billing & Coding Articles. Try using the MCD Search to find what you're looking for. Enter the code you're looking for in the "Enter keyword, code, or document ID" box. The list of results will include documents which contain the code you entered.
Please Note: For Durable Medical Equipment (DME) MACs only, CPT/HCPCS codes remain located in LCDs. All other Codes (ICD-10, Bill Type, and Revenue) have moved to Articles for DME MACs, as they have for the other Local Coverage MAC types.
National Coverage
NCDs do not contain claims processing information like diagnosis or procedure codes nor do they give instructions to the provider on how to bill Medicare for the service or item. For this supplementary claims processing information we rely on other CMS publications, namely Change Requests (CR) Transmittals and inclusions in the Medicare Fee-For-Service Claims Processing Manual (CPM).
In order for CMS to change billing and claims processing systems to accommodate the coverage conditions within the NCD, we instruct contractors and system maintainers to modify the claims processing systems at the national or local level through CR Transmittals. CRs are not policy, rather CRs are used to relay instructions regarding the edits of the various claims processing systems in very descriptive, technical language usually employing the codes or code combinations likely to be encountered with claims subject to the policy in question. As clinical or administrative codes change or system or policy requirements dictate, CR instructions are updated to ensure the systems are applying the most appropriate claims processing instructions applicable to the policy.
How do I find out if a specific CPT code is covered in my state?
Enter the CPT/HCPCS code in the MCD Search and select your state from the drop down. (You may have to accept the AMA License Agreement.) Look for a Billing and Coding Article in the results and open it. (Or, for DME MACs only, look for an LCD.) Review the article, in particular the Coding Information section.
If you need more information on coverage, contact the Medicare Administrative Contractor (MAC) who published the document. The contractor information can be found at the top of the document in the Contractor Information section (expand the section to see the details).
If you don’t find the Article you are looking for, contact your MAC .
Did you receive a Medicare coverage denial?
Was your Medicare claim denied? Here are some hints to help you find more information:
1) Check out the Beneficiary card on the MCD Search page.
2) Try using the MCD Search and enter your information in the "Enter keyword, code, or document ID" box. Your information could include a keyword or topic you're interested in; a Local Coverage Determination (LCD) policy or Article ID; or a CPT/HCPCS procedure/billing code or an ICD-10-CM diagnosis code. Try entering any of this type of information provided in your denial letter.
3) Contact your MAC .
4) Visit Medicare.gov or call 1-800-Medicare.
It is Thursday and the weekly MCD data isn’t refreshed?
Are you having technical issues with the medicare coverage database (mcd), mcd session expiration warning.
Your MCD session is currently set to expire in 5 minutes due to inactivity. If your session expires, you will lose all items in your basket and any active searches. If you would like to extend your session, you may select the Continue Button.
Reset MCD Search Data
If you are experiencing any technical issues related to the search, selecting the 'OK' button to reset the search data should resolve your issues.
Enjoy Free Shipping Today
- Cellphone icon CALL US: 866.992.7279
- Account icon Log in
- Nasal Masks
- Nasal Pillow Masks
- Full Face Masks
- Hybrid Masks
- Cloth Masks
- Total Face Masks
- Masks Without Headgear
- Cushions & Pillows
- Headgear & Clips
- Swivels & Elbows
- Other Mask Parts
- Philips Respironics
- Fisher & Paykel
- Circadiance
Find Your Perfect Mask
- Hoses & Tubing
- Humidifier Chambers & Parts
- Batteries & Power
- Travel Bags
AirSense 10 Adjusts to Your Sleep
- Bags & Cases
- Cleaners & Moisturizers
- Tubing Covers & Wraps
- Aromatherapy
SoClean 2 - The Number 1 Sanitizer
- » Stationary & Home
- » Portable & Travel
- » Filters
- » Cannulas
- » Tubing
- » Comfort Accessories
- Compressor Kits
- Parts & Supplies
AirMini AutoSet Travel Auto-CPAP Machine Package
Contact us for information & alternatives.
One of the smallest CPAPs in the world is also one of the most advanced. AirMini brings ResMed's proven AutoSet Auto-CPAP algorithms, industry leading EPR comfort technologies, and unmatched design and quality to a truly portable Auto-CPAP. It's quiet and small and weighs just 10.6 ounces!
content or image
Content html.
Small & Portable: Great for Home & Travel: Resmed's AirMini is more than just an ultra portable Auto-CPAP machine, it's a turn-key solution for sleep therapy at home or on the go. AirMini Auto includes ResMed's advanced Autoset and AutoSet For Her breathing algorithms that provide effective therapy at the lowest pressure levels all night long. The AutoSet algorithm monitors your breathing and, when it detects flow limitations, it gently increases pressure until the event has cleared. After an event AutoSet decreases pressure again to improve overall sleep comfort.

HumidX Effective Waterless Humidification: Leave your distilled water at home and still get the benefits of humidification! AirMini’s HumidX & HumidX Plus Heat Moisture Exchanging (HME) Humidifying Filters provide the comfort of humidification without the bulk hassle of your typical water based humidifier systems. The HumidX Humidifying Filters work by capturing the moisture from exhaled heat and stores it in the HME prior to reaching your masks vents. When you inhale the HumidX HME releases the humidity back into your therapy stream for portable, waterless and effective humidification.
- HumidX HME Humidifiers are exclusively compatible with the following AirMini Mask Setup Packs: AirFit and AirTouch N20 & N30 Nasal, F20 Full Face, and P10 Nasal Pillow.
- HumidX: Use standard HumidX HMEs for most climates and sleep environments.
- HumidX Plus: Use HumidX Plus for dry and high altitude environments, like aircraft, where humidity is low.

Enhanced Compliance with Bluetooth & the AirMini App: Manage your sleep therapy and comfort settings with ease when you download the free AirMini App for iOS and Android. You can also track your therapy progress directly on your phone or tablet! With a simple push of a button the sophisticated AirMini App syncs data wirelessly, via a Bluetooth connection, so you can review your score each morning as well as access the previous 30 days of sleep data too. Using the AirMini App is a great way to stay on top of your sleep therapy!
SmartStart & Auto Stop Convenience: The AirMini’s SmartStart function starts your sleep apnea therapy as soon as you breathe into your mask. If you remove your mask, the therapy will stop after just a few seconds. You also have the option to stop your therapy on your own if you prefer, AirMini lets you do that with just a touch of a button.
Expiratory Pressure Relief: ResMed's Expiratory Pressure Relief feature will reduce the work of breathing during exhalation and provide a gentle pressure that naturally adapts to your breathing cycle throughout the night. You can turn off the Expiratory Pressure Relief or choose levels from 1 to 3, 1 being the minimum pressure relief and 3 being the maximum.
AutoRamp with Sleep Onset Detection: AirMini’s AutoRamp feature with sleep onset detection helps make your sleep therapy comfortable from the moment you turn on your device. The AutoRamp feature works by delivering a lower pressure setting to help you fall asleep easier. Once the device detects that you’re asleep, it comfortable ramps up the pressure to ensure the device is delivering your prescribed pressure setting. If you prefer a set ramp time or want the auto ramp turned off all together, you can simply do that too. Comfort settings are easy with the AirMini App!
FAA Approved for Use on Commercial Flights: The AirMini is great for home, but it is FAA approved and built for travel as well. You can slide it into your overnight bag and head out the door, or better yet upgrade with a custom fit AirMini Premium Travel Bag for added protection and convenience.
Popular Together

AirMini HumidX (Standard) HME Humidifier Filters for AirFit & AirTouch N20, N30 & P10 Masks (3 Pack)

ResMed Disposable Fine Filter for AirMini CPAP Machines

Premium Travel Bag for AirMini CPAP Machines
Teaser Trailer For The AirMini Travel Auto-CPAP
Introduction To Your AirMini Travel Auto-CPAP
Setup Your AirMini Travel Auto-CPAP
Humidification Options For Your AirMini Travel Auto-CPAP
- AirMini Auto-CPAP Brochure PDF
- AirMini Information Guide PDF
- AirMini User Manual PDF
- AirMini iOs App User Manual PDF
- AirMini Android App User Manual PDF
Checkmark icon Added to your cart:
- Newsletters

Working from home?
Keep your critical coding and billing tools with you no matter where you work.
Create your Find-A-Code account today!
AHA Coding Clinic ® for HCPCS - 2017 Issue 4; Ask the Editor
Home automatic positive airway pressure (apap).
A patient was seen in our sleep lab for sleep study, which resulted in a diagnosis of sleep apnea and an order for a home Automatic Positive Airway Pressure (APAP) Titration Study in order to determine the appropriate CPAP pressure. The patient returned to the sleep lab and an APAP machine was provided with instructions for home use. Five days later, they brought the APAP machine back as instructed. Data was downloaded from the APAP machine and the physician documented an interpretation and subsequently ordered a home CPAP machine from our durable medical equipment (DME) provider to be set at the established pressure and delivered to the patient for ongoing home CPAP therapy. What CPT/HCPCS code(s) should the sleep lab use for the home APAP Titration Study? Many of our coders feel that CPT 94660, Continuous positive airway pressure ventilation (cap), initiation and management, is the most appropriate code as this study is an inherent part of initiating CPAP therapy. However, some of our coders feel that 94660 is not appropriate and recommend reporting this work with a facility E/M code. ...
To read the full article, sign in and subscribe to the AHA Coding Clinic ® for HCPCS.
Thank you for choosing Find-A-Code, please Sign In to remove ads.


IMAGES
VIDEO
COMMENTS
CPAP/BiPAP Machine Insurance (HCPCS) Codes. E0601: Continuous airway pressure (CPAP/APAP) device: E0470: Respiratory assist device, bi-level pressure (BiPAP) capability, WITHOUT backup rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pressure device)
Every medical product or service has a CPT (Current Procedural Terminology) code assigned to it. Government healthcare providers use HCPCS (Healthcare Common Procedure Coding System) which are generally the same as the CPT codes. Frequently the CPT or HCPCS codes are referred to a "billing codes".
You can usually find the ICD10 (or the older ICD9) code for your condition listed on prescriptions or medical records. Below are common ICD-10 codes for diagnoses treated by products sold on this site. COMMON SLEEP & OXYGEN THERAPY DIAGNOSIS CODES (ICD10) G47.30. Sleep Apnea (Unspecified) G47.31.
CPAP patients who use ResMed ClimateLineAir heated ... HCPCS codes Air11 Travel Bag 39221 Air11 Filter, STD 1 pack 39300 A7038 Air11 Filter, ... HCPCS codes AirSense 11 AutoSet USA CO 39000 E0601 + E0562 + A7037 + A9279 AirSense 11 AutoSet USA TRI 39001 E0601 + E0562 + A4604 + A9279
You can use the following codes to request miscellaneous CPAP-related supplies: A9999 for accessories. E1399 for device-related supplies. Client services representatives and Faith (the interactive voice response system) don't typically ask patients if they require miscellaneous supplies during outreach. However, these codes allow you to offer ...
Thus, using the HCPCS codes for CPAP (E0601) or bi-level PAP (E0470, E0471) devices for a ventilator (E0465, E0466) used to provide CPAP or bi-level PAP therapy is incorrect coding. Claims for ventilators billed using the CPAP or bi-level PAP device HCPCS codes will be denied as incorrect coding.
Note: Inclusion or exclusion of a code for a specific product or supply does not imply any health insurance coverage or reimbursement policy. All referenced information an d codes were taken from HCPCS. Please refer to DMEPOS Supplier Manual for complete explanations. Customer Service: 1-800-345-6443 • 724-387-4000
In an effort to assist out customers in filing a claim we are providing a list of the most common HCPCS codes used for sleep therapy and oxygen therapy equipment and supplies. CPAP/BiLevel Michine HCPCS Codes: E0601 Continuous airway pressure device (CPAP/APAP) E0470 Respiratory assist device, bi-level pressure capability, without backup rate ...
Below are the list of HCPCS codes For BiPAP/ CPAP Mask Coverage. HCPCS CODE: A7030. Positive Airway Pressure (BiPAP, APAP, CPAP) equipment with a Full Face Mask. HCPCS CODE: A7034. With or without a head strap, a nasal interface (mask or cannula type) is used with positive airway pressure (CPAP/BiPAP/APAP) equipment. HCPCS CODE: A7044.
CPAP, Bi-Level, Bi-PAP MACHINE INSURANCE (HCPCS) CODES. E0601 - Continuous airway pressure (CPAP/APAP) device. E0470 - Respiratory assist device, Bi-Level pressure (Bi-PAP) capability, without backup rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pressure device)
It has since been determined a universal modifier will not be established. Providers should continue to bill using Healthcare Common Procedure Coding System (HCPCS) code E1399 for portable CPAP claims with dates of service on or after May 20, 2020. Learn more about TRICARE's CPAP benefit, including authorization details, on our CPAP details page.
For auto-titrating single-level CPAP devices use HCPCS code E0601. A bi-level respiratory assist device without backup rate (E0470) allows independent setting of inspiratory and expiratory pressures to deliver positive airway pressure within a single respiratory cycle by way of tubing and a noninvasive interface (such as a nasal, oral, or ...
Below are the HCPCS codes you may need for the claim form: HCPCS CODES. CPAP/BiPAP MACHINE. E0601- Continuous airway pressure (CPAP/APAP) device. E0470- Respiratory assist device, bi-level pressure (BiPAP) capability, WITHOUT backup rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with ...
CPAP/Bi-PAP MACHINE INSURANCE (HCPC) CODES E0601 Continuous airway pressure (CPAP/APAP) device E0470 Respiratory assist device, bi-level pressure (Bi-PAP) capability, WITHOUT backup rate feature, used with noninvasive interface, e.g., nasal or facial mask (intermittent assist device with continuous positive airway pres
Below is a detailed list of codes your insurance company may need to quickly process your claim. E0601 - CPAP Machine Purchase. A7034 - CPAP Nasal Mask. A7032 - CPAP Nasal Mask Cushion. A7030 - CPAP Full Face Mask. A7031 - CPAP Full Face Mask Cushion. A7044 - CPAP Full Oral Interface. A7046 - CPAP Humidifier Chamber.
E0601 is officially described by HCPCS. The description of this code can be found below. Short Description: "Cont airway pressure device.". Long Description: "Continuous positive airway pressure (CPAP) device.". Code: D1E. Pricing Indicator: 36. Code Added: January 01, 1988. Last Changed: January 01, 2014.
HCPCS CODES: EQUIPMENT: Group 1 Codes. Code Description; ... (CPAP) DEVICE Group 2 (19 Codes) Group 2 Paragraph. ACCESSORIES. Group 2 Codes. Code Description; A4604 TUBING WITH INTEGRATED HEATING ELEMENT FOR USE WITH POSITIVE AIRWAY PRESSURE DEVICE A7027 COMBINATION ORAL/NASAL MASK, USED WITH CONTINUOUS POSITIVE AIRWAY PRESSURE DEVICE, EACH ...
Codes. HCPCS. HCPCS Codes. Durable Medical Equipment E0100-E8002. Humidifiers and Nebulizers with Related Equipment E0550-E0601. Continuous positive airway pressure (CPAP) device. E0600. E0601. E0602.
Continuous positive airway pressure (cpap) device. Durable Medical Equipment (DME) E0601 is a valid 2024 HCPCS code for Continuous positive airway pressure (cpap) device or just " Cont airway pressure device " for short, used in Rental of DME .
AirMini Auto-CPAP Machine, Drawstring Travel Bag, Universal Power Supply with Cord, Starter Filter, User Manual. Part Number(s) 38113 HCPCS Code: Not Applicable Warranty: 2-Year Manufacturer's Warranty + Exclusive 15-Night Money Back Guarantee! GTIN / UPC Code: 00619498381012
Reimbursement resources - ResMed Healthcare Professional. Find answers to your ResMed reimbursement inquiries, including Centers for Medicare & Medicaid Services (CMS) policies.
Level. 29 dBA. Weighing 10 ounces and with a small 20-watt AC power cord, the ResMed AirMini is a compact device that should easily fit into your travel bag. In addition to use on business trips and camping, this portable CPAP can be used on airplanes since it is FAA-approved for in-flight use.
AHA Coding Clinic ® for HCPCS - 2017 Issue 4; Ask the Editor Home Automatic Positive Airway Pressure (APAP) A patient was seen in our sleep lab for sleep study, which resulted in a diagnosis of sleep apnea and an order for a home Automatic Positive Airway Pressure (APAP) Titration Study in order to determine the appropriate CPAP pressure.