
- Introduction
- Palp/Percus
- Auscultation

Palpation/Percussion
Thoracic expansion:.
- Is used to evaluate the symmetry and extent of thoracic movement during inspiration.
- Is usually symmetrical and is at least 2.5 centimeters between full expiration and full inspiration.
- Can be symmetrically diminished in ankylosing spondylitis .
- Can be unilaterally diminished in chronic fibrotic lung disease , extensive lobar pneumonia, large pleural effusions, bronchial obstruction and other disease states.
Percussion:
Percussion is the act of tapping on a surface, thereby setting the underlying structures in motion, creating a sound and palpable vibration. Percussion is used to determine whether underlying structures are fluid-filled, gas-filled, or solid. Percussion:
- Penetrates 5 - 6 centimeters into the chest cavity.
- May be impeded by a very thick chest wall.
- Produces a low-pitched, resonant note of high amplitude over normal gas-filled lungs.
- Produces a dull, short note whenever fluid or solid tissue replaces air filled lung (for example lobar pneumonia or mass) or when there is fluid in the pleural space (for example serous fluid, blood or pus).
- Produces a hyperresonant note over hyperinflated lungs (e.g. COPD ).
- Produces a tympanitic note over no lung tissue (e.g. pneumothorax ).
Diaphragmatic excursion:
- Can be evaluated via percussion.
- Is 4-6 centimeters between full inspiration and full expiration.
- May be abnormal with hyperinflation , atelectasis , the presence of a pleural effusion , diaphragmatic paralysis, or at times with intra-abdominal pathology.

- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created Craig Hacking had no recorded disclosures.
At the time the article was last revised Craig Hacking had the following disclosures:
- Philips Australia, Paid speaker at Philips Spectral CT events (ongoing)
These were assessed during peer review and were determined to not be relevant to the changes that were made.
- Diaphragm fluoroscopy
The fluoroscopic sniff test , also known as diaphragm fluoroscopy , is a quick and easy real time fluoroscopic assessment of diaphragmatic motor function (excursion). It is used most often to confirm absence of muscular contraction of the diaphragm during inspiration in patients with phrenic nerve palsy or breathing difficulties following stroke . Chest radiograph demonstrating a newly elevated hemidiaphragm often precedes a sniff test.
In critically unwell patients who can not attend the fluoroscopy unit in the radiology department, bedside US assessment can be used to demonstrate appropriate diaphragmatic movement with normal respiration and when asked to sniff (see case 5).
The following technique is suggested:
ask the patient to practice sniffing before the study
with the patient either standing (preferred) or supine, perform frontal fluoroscopy of the diaphragm at rest, breathing quietly through an open mouth
ask the patient to take a few quick short breaths in with a closed mouth ('sniffs') causing rapid inspiration
occasionally, repeating (3) in the lateral projection is required to evaluate the posterior hemidiaphragms
In normal diaphragmatic motion:
the diaphragm contracts during inspiration: moves downwards
the diaphragm relaxes during expiration: moves upwards
both hemidiaphragms move together
in healthy patients 1-2.5 cm of excursion is normal in quiet breathing 2
3.6-9.2 cm of excursion is normal in deep breathing 2
up to 9 cm can be seen in young or athletic individuals in deep inspiration 2
excursion in women is slightly less than men 2
In abnormal diaphragmatic motion:
the affected hemidiaphragm does not move downwards during inspiration
paradoxical motion can occur
Interpretation
Absence of diaphragmatic movement confirms phrenic nerve palsy in the appropriate clinical setting. A mass anywhere along the course of the phrenic nerve requires further workup, usually with neck and chest CT. A hilar mass due to lung cancer is the most common finding on CT and a classic exam case.
Normal diaphragmatic excursion can also be impaired in patients with:
previous diaphragmatic trauma or surgery
neuromuscular disorders
previous stroke
- 1. Nason LK, Walker CM, McNeeley MF et-al. Imaging of the diaphragm: anatomy and function. Radiographics. 2012;32 (2): E51-70. doi:10.1148/rg.322115127 - Pubmed citation
- 2. Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values. Chest. 2009;135 (2): 391-400. doi:10.1378/chest.08-1541 - Pubmed citation
- Nason L, Walker C, McNeeley M, Burivong W, Fligner C, Godwin J. Imaging of the Diaphragm: Anatomy and Function. RadioGraphics. 2012;32(2):E51-70. doi:10.1148/rg.322115127 - Pubmed
Incoming Links
- Diaphragmatic paralysis
- Phrenic nerve palsy
- Ultrasound diaphragmatic sniff test
- Left hilar mass causing phrenic nerve palsy
- Large right diaphragmatic hernia
- Hemidiaphragmatic paralysis
- Abnormal sniff test
- Normal sniff test
- Phrenic nerve palsy with positive sniff test
Promoted articles (advertising)
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Sonographic evaluation of diaphragmatic thickness and excursion as a predictor for successful extubation in mechanically ventilated preterm infants
- Original Article
- Published: 28 September 2020
- Volume 180 , pages 899–908, ( 2021 )
Cite this article
- Eslam Bahgat 1 ,
- Hanan El-Halaby 2 ,
- Ashraf Abdelrahman 3 ,
- Nehad Nasef ORCID: orcid.org/0000-0001-7650-123X 1 , 2 , 4 &
- Hesham Abdel-Hady 1 , 2
3224 Accesses
18 Citations
7 Altmetric
Explore all metrics
A Correspondence to this article was published on 12 November 2020
Sonographic assessment of diaphragmatic thickness and excursion has been found to be an accurate tool in predicting successful extubation of adult patients from invasive mechanical ventilation. We aimed to evaluate the accuracy of sonographic assessment of diaphragmatic thickness and excursion in predicting successful extubation of preterm infants from invasive conventional mechanical ventilation. Preterm infants less than 32 weeks gestation who required invasive conventional mechanical ventilation were evaluated by diaphragmatic sonography within 1 h of their planned extubation. Infants were classified into successful or failed extubation groups based on their ability to stay off invasive mechanical ventilation for 72 h after extubation. Inspiratory and expiratory thickness plus excursion of the right and left hemidiaphragm as well as diaphragmatic thickening fraction (DTF) measures were compared between groups. We included 43 eligible infants, of whom 34 infants succeeded and 9 infants failed extubation. Infants in the successful extubation group had a significantly higher expiratory thickness of the right and left hemidiaphragm, excursion of the right and left hemidiaphragm, inspiratory thickness of the left hemidiaphragm, and DTF of the left hemidiaphragm compared with infants who failed extubation. The receiver-operating characteristic curves showed that excursion of the right and left hemidiaphragm has the highest significant accuracy in predicting successful extubation of preterm infants among all diaphragmatic parameters (AUC is 0.98 and 0.96, respectively; p value < 0.001 for both).
Conclusion : We conclude that diaphragmatic excursion is a useful indicator for successful extubation of preterm infants from mechanical ventilation.
Similar content being viewed by others

Diaphragmatic ultrasound as a predictor of successful extubation from mechanical ventilation: thickness, displacement, or both?
Ayman I. Baess, Tamer H. Abdallah, … Maged Hassan
Change in Diaphragmatic Thickness During the Respiratory Cycle Predicts Extubation Success at Various Levels of Pressure Support Ventilation
Scott Blumhof, David Wheeler, … Jorge Mora

Diaphragmatic parameters by ultrasonography for predicting weaning outcomes
Pongdhep Theerawit, Dararat Eksombatchai, … Sumalee Kiatboonsri
Avoid common mistakes on your manuscript.
Introduction
The decision to extubate preterm infants from mechanical ventilators is mainly based on clinical assessment, blood gases, and ventilator settings [ 7 ]. Researchers attempted to evaluate different parameters as predictors for successful extubation of preterm infants from mechanical ventilation [ 26 , 28 ]. However, up to 30% of preterm infants who are extubated based on the clinical assessment require re-intubation indicating a poor correlation with infants’ readiness for extubation [ 3 , 28 ].
The diaphragm represents the main respiratory muscle in infancy. It contributes to generation of an estimated three-fourths of the infant's tidal volume during resting inspiration in the supine position [ 23 ]. Continuous positive airway pressure (CPAP) affects the crura of diaphragm by shortening the muscle and decreasing excursion through maintaining end expiratory lung volume [ 21 ]. Moreover, prolonged mechanical ventilation triggers myofibrillar contractile dysfunction and myofilament protein loss of the diaphragmatic muscles which later results in loss of diaphragmatic force-generating capacity, poor activity, and unloading of the diaphragm [ 10 ]. This phenomenon of ventilator-induced diaphragmatic dysfunction (VIDD) has raised the attention of investigators to the correlation between duration of mechanical ventilation and failure to extubate preterm infants from mechanical ventilation [ 27 ]. However, the diagnosis of this diaphragmatic dysfunction can be hindered by the lack of appropriate quantitative assessments of neonatal diaphragm function [ 1 ].
Accurate assessment of diaphragm function in the neonate could aid to the diagnosis of respiratory distress, evaluation of therapeutic interventions, and identification of infants ready to wean from mechanical ventilation [ 20 ]. Monitoring the electrical activity of the diaphragm in infants and children has shown that higher diaphragmatic activity in relation to tidal volume indicates a better preserved diaphragmatic function and a better chance of passing the extubation readiness test [ 29 ]. However, the tools needed for monitoring the electrical activity of the diaphragm are invasive, expensive, and require trained personnel for proper interpretation. Sonographic evaluation of the diaphragm is ubiquitous in medical facilities, requires no radiation, can be used at the infant’s bedside, and useful in assessing diaphragmatic mobility and excursion [ 13 ].
We hypothesized that assessment of diaphragmatic dimensions and excursion, before planned extubation, may be helpful in predicting successful extubation of preterm infants from mechanical ventilation. We aimed to study sonographic assessment of the diaphragmatic dimensions and excursion for mechanically ventilated preterm infants as a predictor for success of extubation.
The present study was placed at the Neonatal Intensive Care Unit (NICU) of Mansoura University Children’s Hospital, Mansoura, Egypt, between January 2017 and November 2019. The study was approved by the Institutional Review Board, Mansoura Faculty of Medicine, and a fully informed written consent was obtained from the parent or infant's guardian before enrolment in the study.
Study designs
This was a prospective, observational, cohort study assessing diaphragmatic thickness and excursion for preterm infants prior to planned extubation from invasive conventional mechanical ventilation.
Participants
Preterm infants less than 32 weeks gestation who were supported by invasive conventional mechanical ventilation for a diagnosis of respiratory distress syndrome, as evident by clinical and radiological findings, and planned for extubation were eligible for this study. Preterm infants with chromosomal aberrations, hepatosplenomegaly, pleural effusion, congenital heart or lung disorders, or congenital anomalies related to diaphragm as diaphragmatic hernia and diaphragmatic paralysis were excluded from the study.
Intervention
Eligible preterm infants had sonographic assessment of diaphragmatic thickness and excursion within 1 h of planned extubation from invasive conventional mechanical ventilation to non-invasive respiratory support. Preterm infants were extubated from mechanical ventilation if they fulfilled the following criteria: spontaneous respiratory effort, presence of cough or gag induced by suctioning, acceptable arterial blood gases (pH more than 7.25, PaCO 2 less than 60 mmHg, and base deficit less than 8 mEq/L) on a mean airway pressure less than 8 cm H 2 O and respiratory rate of less than 30/min, saturation more than 90% on fraction of inspired oxygen (FiO 2 ) less than 30% in the preceding 24 h, and the decision of extubation was taken by the attending physician who was blinded to the results of sonographic measurements.
Sonographic diaphragmatic parameters were measured while infants were on spontaneous pressure support ventilation mode with a support pressure of 4 cm H 2 O over an end expiratory pressure of 4 cm H 2 O for 1 h prior to the sonographic assessment as an accommodation. The total duration on pressure support ventilation mode and sonographic diaphragmatic assessment was 2 h at most to avoid infant exhaustion. Sonographic evaluation was performed prior to the time of next feed, while infant’s stomach is empty, to avert any interference of a full stomach on diaphragmatic mobility and measurements. All infants were extubated to nasal CPAP using the Infant Nasal CPAP Assembly system (Fisher & Paykel Healthcare, Auckland, New Zealand) at a pressure of 5 cmH 2 O and FiO 2 between 21% and 30% to keep infant's saturation between 90% and 95%.
Sonographic diaphragmatic assessment technique
Ultrasonographic examinations were performed by one operator, who had ten years of experience in diaphragm sonography, using a portable Doppler ultrasonography (Micro-Maxx; SonoSite, Bothell, WA, USA) with a micro-convex transducer array (10 to 5 MHz). Diaphragmatic sonography was performed while the infant is in supine position after ensuring quiet regular breathing. For visualization of the right hemidiaphragm, the convex probe was placed over the right subcostal and lower intercostal spaces between the anterior axillary and the midclavicular lines with the probe directed cranially, dorsally, and medially so the radial beam came to be perpendicular to the posterior third of the right hemidiaphragm. For visualization of the left hemidiaphragm, the same technique, position, and direction of the probe as the right hemidiaphragm were performed apart from the probe was placed between the left anterior axillary and midaxillary lines.
At first, the two-dimensional mode was screened to detect the appropriate exploration image for each hemidiaphragm in which the diaphragm appeared as a hypoechoic line that was placed between two echogenic lines, the upper one was the reflection of the parietal pleura and the lower was for the peritoneum. After that, the M-mode ultrasonography was screened and the image was frozen after ensuring regular up and down movement of the diaphragmatic line that reflects regular breathing. The thickness of the diaphragmatic line during inspiration (upward slope) and expiration (downward slope) represents the diaphragmatic inspiratory and expiratory thickness, respectively. The perpendicular distance between the most caudal point of this line during inspiration and the most caudal point during expiration represents the diaphragmatic excursion. Diaphragmatic thickness and kinetics measures can be affected by the irregular breathing pattern, high respiratory rate, breath to breath variability, and small diaphragmatic dimensions by using M-mode technique in preterm infants. To overcome this technical limitation, the investigator observed for regular up and down movements of the diaphragmatic line in M-mode and cine for 1 min to ensure an epoch of quiet regular breathing, and then diaphragmatic measurements were obtained [ 2 ]. The technique and measurements were repeated up to 3 respiratory cycles for each hemidiaphragm, and the average one was recorded [ 5 ]. Avoidance of diaphragmatic measurements during infant’s crying or sighing movement was taken in consideration.
The diaphragmatic thickening fraction (DTF) was calculated and recorded using the following formula: DTF = [(inspiratory thickness − expiratory thickness) / expiratory thickness] × 100 [ 8 ].
The intra-observer reproducibility was evaluated by repeated measurements of sonographic diaphragmatic parameters by the same investigator with 30 min in between measurements. Ten clinically stable preterm infants, age and sex cross-matched with the studied group, were randomly selected for this purpose.
Study end point
The primary study end point was successful extubation from invasive mechanical ventilation defined as being off mechanical ventilation with transmission to oxygen therapy or non-invasive respiratory support, for at least 72 h post-extubation [ 12 ]. The indications for re-intubation were specified as follows: more than six episodes of apnea requiring stimulation within 6 h, or more than one significant episode of apnea requiring bag and mask ventilation, respiratory acidosis (PaCO 2 > 65 mmHg and pH < 7.25) or FiO 2 > 60% to maintain saturation in the target range (90–95%) [ 12 ].
Sample size calculation
Sample size calculation was based on the area under the receiver-operating characteristic curve that was 0.79 for predicting successful extubation of mechanical ventilation retrieved from previous research [ 4 ]. Using MedCalc for Windows, version 15.0 (MedCalc Software, Ostend, Belgium), sample size calculation using area under ROC curves with null hypothesis = 0.5, α-error = 0.05, power of the study = 80% ratio of positive to negative cases which will be considered as 3.3. The total calculated sample size will be 43 cases.
Statistical analysis
Statistical analysis was performed using SPSS statistical software (version 21; IBM Corporation, Armonk, NY, USA). Student’s t test was used to compare continuous parametric variables. Mann–Whitney U test was used for continuous non-parametric variables. Chi-square test or Fisher’s exact test was used for categorical variables when appropriate. Shapiro–Wilk test was done to examine the distribution of data. Pearson's correlation coefficient test was used to correlate between duration of invasive mechanical ventilation and different diaphragmatic measures. The accuracy of different diaphragmatic measurements for predicting successful extubation from invasive mechanical ventilation was evaluated using receiver-operating characteristic (ROC) curves. A p value of < 0.05 is considered to be statistically significant. Data are expressed as mean ± standard deviation, median (inter-quartile range), or number (percentage) unless otherwise stated. Reproducibility of the diaphragmatic measurements was assessed by Bland–Altman analysis and Pearson’s correlation coefficient.
Of the 164 preterm infants who were at less than 32 weeks gestation admitted to our NICU during the study period, 62 infants required invasive conventional mechanical ventilation, 43 were included in the study, and 19 were excluded due to various causes (Fig. 1 ). A total of 34 infants succeeded and 9 infants failed extubation. Infants in the failed extubation group had significantly higher postnatal age at extubation, longer duration of invasive mechanical ventilation, higher pre-extubation mean airway pressure, and higher pre-extubation FIO 2 compared with infants in the successful extubation group (Table 1 ). Of the 9 infants who failed extubation, 6 infants were reintubated for increased work of breathing in association with hypoxia, two infants were reintubated for increased work of breathing in association with hypercapnia, and one infant was reintubated for apnea which was preceded by increased work of breathing. The mean time for reintubation was 43.5 ± 13.5 h with a minimum of 29 and a maximum of 66 h, respectively. Measurements were highly reproducible with a high degree of agreement between diaphragmatic dimensions as assessed by Pearson’s correlation coefficient and Bland–Altman analysis. Pearson’s correlation coefficient values were above 0.9, and p values were < 0.001 for all measured diaphragmatic indices.
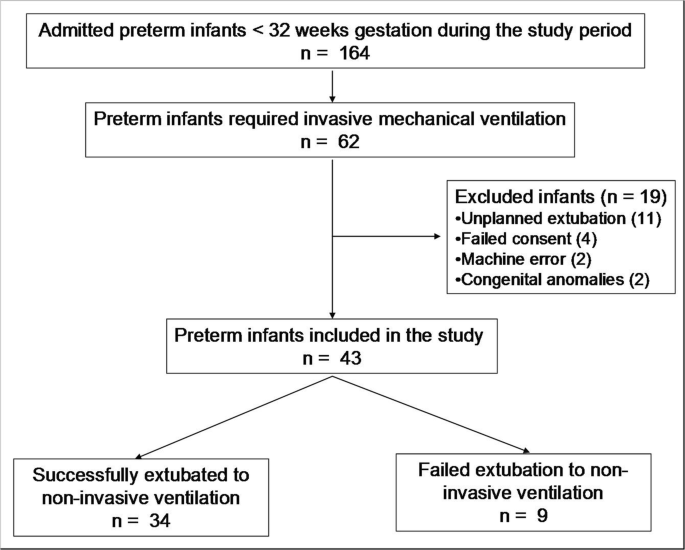
Diagram showing the flow of participants in the study
Infants in the successful extubation group had a significantly higher expiratory thickness of the right and left hemidiaphragm, excursion of the right and left hemidiaphragm, inspiratory thickness of the left hemidiaphragm, and DTF of the left hemidiaphragm compared with infants who failed extubation to nasal CPAP (Table 2 ) (Fig. 2 ). The duration of invasive mechanical ventilation had a significant negative correlation with inspiratory and expiratory thickness of the right and left hemidiaphragm, excursion of the right hemidiaphragm, and DTF of the right and left hemidiaphragm (Table 3 ).
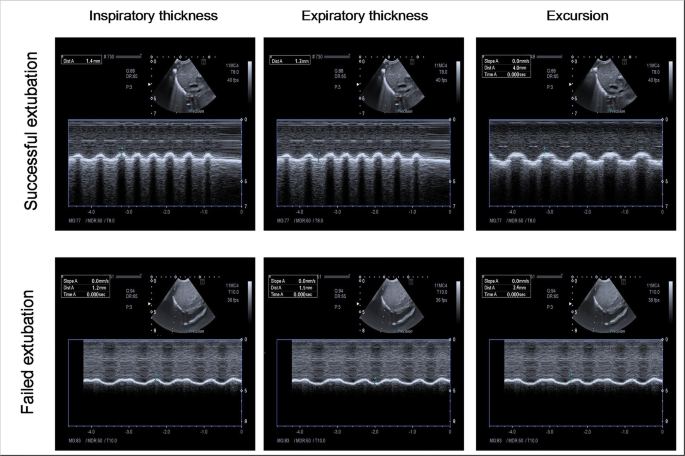
Sonographic images showing M-mode measurements of inspiratory thickness, expiratory thickness, and excursion of the right hemidiaphragm in an infant (case number 5) from the successful extubation group and an infant (case number 11) from the failed extubation group
The ROC curves showed that expiratory thickness of the right and left hemidiaphragm, excursion of the right and left hemidiaphragm, inspiratory thickness of the left hemidiaphragm, and DTF of the left hemidiaphragm had significant accuracies in predicting successful extubation of preterm infants (Fig. 3 ). Excursion of the right and left hemidiaphragm showed the highest accuracy among all diaphragmatic parameters. A right hemidiaphragmatic excursion of 2.75 mm was associated with 94% sensitivity and 89% specificity in predicting successful extubation. A left hemidiaphragmatic excursion of 2.45 mm was associated with 94% sensitivity and 89% specificity in predicting successful extubation.
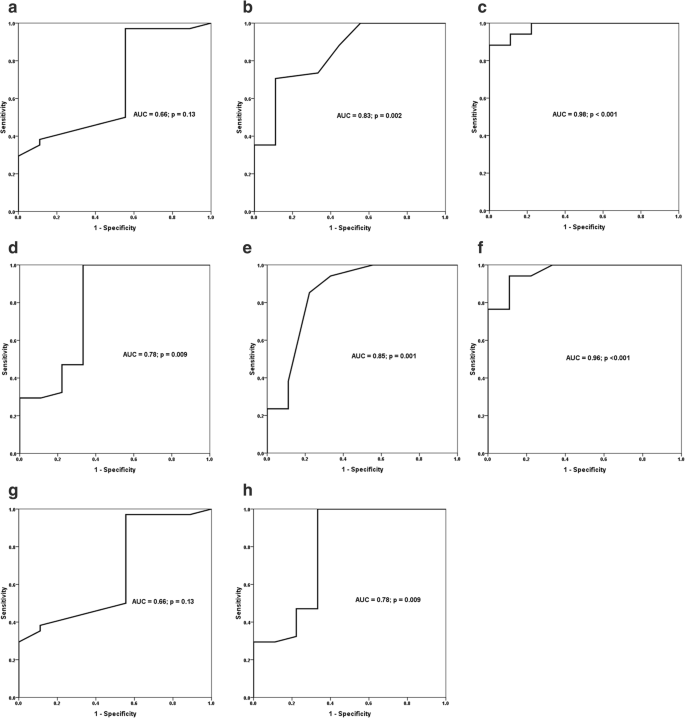
Receiver-operating characteristic curves show area under the curve (AUC) and p value of significance for inspiratory thickness of the right hemidiaphragm ( a ), expiratory thickness of the right hemidiaphragm ( b ), excursion of the right hemidiaphragm ( c ), inspiratory thickness of the left hemidiaphragm ( d ), expiratory thickness of the left hemidiaphragm ( e ), excursion of the left hemidiaphragm ( f ), and diaphragm thickening fraction (DTF) of the right hemidiaphragm ( g ) and the left hemidiaphragm ( h ) in predicting successful extubation of preterm infants from mechanical ventilation
Sonographic assessment of the lungs and diaphragm has gained the interest of neonatologists nowadays. Sonographic assessment of the lungs has shown a high sensitivity and specificity in diagnosing various respiratory disorders in neonates [ 24 ]. Ultrasound has been recently used to assess diaphragmatic thickness and excursion of diaphragmatic dome in stable spontaneously breathing infants [ 5 ]. We aimed to assess the accuracy of sonographic assessment of diaphragmatic thickness and excursion as a predictor for successful extubation of preterm infant from invasive conventional mechanical ventilation. The main finding of our study is that excursion of the right and left hemidiaphragm has the highest accuracy in predicting successful extubation of mechanically ventilated preterm infants. Diaphragmatic excursion was significantly higher in preterm infants successfully extubated from invasive conventional mechanical ventilation compared with infants who failed extubation.
Diaphragmatic activity as a predictor for successful extubation was evaluated in pediatric age group through monitoring of diaphragmatic electrical activity. Assessment of diaphragmatic electrical activity has shown that infants and children who generated higher diaphragmatic activity in relation to tidal volume had a better chance of passing the extubation readiness test as opposed to infants and children who generated lower diaphragmatic activity in relation to tidal volume [ 29 ]. Authors in this study stated that diaphragmatic activity in relation to tidal volume indicates a better preserved diaphragmatic function [ 29 ].
To the best of our knowledge, this study is the earliest to report the accuracy of assessing diaphragmatic activity by using diaphragmatic ultrasound in prediction of successful extubation in preterm infants. Over 400 participants between 1 month and 16 years, sonographic assessment of the diaphragm has shown a high accuracy in assessing diaphragmatic thickness and excursion [ 5 ]. Rehan and colleagues reported normal diaphragmatic excursion in 34 preterm infants between 26 and 37 weeks gestation to be 5.5 ± 0.2 mm at 26 to 28 weeks gestation, 4.8 ± 0.2 mm in 29 to 31 weeks gestation, 4.6 ± 0.2 mm in 32 to 34 weeks gestation, and 4.4 ± 0.3 mm in 35 to 37 weeks gestation [ 22 ]. The difference between our measurements and Rehan's study is attributed to their inclusion of clinically stable preterm infants who have no evidence of any acute illness, no culture proven sepsis, not on any oxygen supplementation, and not on CPAP or ventilator support compared with our ventilated infants. Radicioni and colleagues tested the accuracy of a model that consists of the sonographic measurements of right diaphragmatic excursions during inspiration and expiratory phases plus the oxygen saturation/FiO 2 ratio as a predictor for CPAP failure in preterm infants with respiratory distress syndrome. The authors found that integration of both measures in this model has a high accuracy, with AUC 0.95, in predicting CPAP failure [ 19 ].
In mechanically ventilated adults, sonographic assessment of diaphragmatic function showed that diaphragmatic excursion was significantly higher in the successful group compared with those who failed extubation [ 6 ]. Liu and colleagues found that diaphragmatic excursion had a sensitivity of 89.2% and a specificity of 75.0% with an AUC (ROC) of 0.849 in predicting successful extubation in mechanically ventilated adult patients. The cut-off value of diaphragmatic excursion for predicting successful extubation was determined to be 1.14 cm by ROC curve analysis [ 16 ]. Yoo et al. found that diaphragmatic excursion is more accurate than a change in the diaphragm thickness to predict extubation success in mechanically ventilated adults [ 31 ]. In a meta-analysis of 13 studies over 742 adults, Li and colleagues concluded that diaphragmatic excursion and thickness are accurate measures for predicting reintubation within 48 h of extubation despite having a large heterogeneities among the included studies [ 15 ].
In mechanically ventilated adults, McCool and colleagues [ 17 ] showed that the duration of mechanical ventilation was significantly shorter in patients diagnosed with normal diaphragmatic function as assessed by ultrasound measurement of diaphragmatic thickness and excursion. The authors stated that normal diaphragmatic function as assessed by ultrasound shows 90.9% sensitivity, 86.7% specificity, 90.9% positive predictive value, and 86.7% negative predictive value in predicting successful extubation from mechanical ventilation [ 17 ].
The proposed mechanism for diaphragmatic dysfunction in association with invasive mechanical ventilation is the loss of myofilament protein of diaphragmatic muscle which results in what is known as ventilator-induced diaphragmatic dysfunction (VIDD). A previous research revealed that only 18–24 h of invasive mechanical ventilation is sufficient to develop VIDD in both laboratory animals and humans [ 18 ]. In animal models, ventilator-induced diaphragmatic proteolysis and associated diaphragmatic atrophy occur due to increased diaphragmatic protein breakdown and decreased protein synthesis which is mediated by various proteases, such as calpain, caspase-3, autophagy, and the ubiquitin-proteasome system [ 18 ]. We have found that expiratory thickness of the right and left hemidiaphragm and inspiratory thickness of the left hemidiaphragm were significantly lower in infants who failed compared with infants who succeeded extubation from mechanical ventilation. Our results support previous results of ventilator-induced diaphragmatic atrophy which were retrieved by animal studies and human studies [ 11 , 14 ]. This is further supported by our finding of negative correlation between the duration of mechanical ventilation with inspiratory and expiratory thickness of the right and left hemidiaphragm, excursion of the right hemidiaphragm, and DTF of the right and left hemidiaphragm. The possible cause of the absence of significant difference in the inspiratory thickness and thickening fraction of the right hemidiaphragm between successfully and failed extubated preterm infants can be attributed to the supporting effect of the liver to the right hemidiaphragm during inspiration which can mask minimal effects on the muscle mass of the right hemidiaphragm. Another possibility for this non-significant difference may be related to our use of M-mode technique during measurement. Compared with B-mode, M-mode may not obtain reliable measurements of the diaphragmatic thickness, due to the subtlety of the imaging line. However, we compensated for this by obtaining our M-mode measures over the most moving point of the hemidiaphragm on B-mode. Moreover, M-mode technique has been successfully used in previous studies to measure diaphragmatic thickness in excursion in adults and pediatric age groups [ 9 , 30 ].
A potential technical limitation to our study is the use of a micro-convex transducer rather than a high-frequency micro-linear transducer for imaging. The latter has better ability for visualization of the thin muscles and superficial structures, like hemidiaphragm. However, the micro-convex transducer gives a better in-between ribs view and wider angle of image “pie-shaped image” of the whole hemidiaphragm which allows for better identification of the most moving part of the hemidiaphragm in B-mode. We compensated for this technical limitation by taking our M-mode measurements at the most moving part of hemidiaphragm in the B-mode view.
We acknowledge that the study is limited by the relatively small sample size, which is attributed to our adoption of the early administration of non-invasive respiratory support techniques to our preterm infants to minimize ventilator-induced lung injury which decreased the percentage of preterm infants who required invasive mechanical ventilation during the study period. The study is also limited by the lack of physiopathologic proof of respiratory etiology as a cause for extubation failure and the need for reintubation. It is of note that assessment of diaphragmatic function in infants who failed extubation due to non-respiratory causes, such as central apnea or poor respiratory drive, is less valuable. Moreover, our practice of extubation to a nasal CPAP of 5 cm H 2 O represents another limitation given the new guidelines of extubating preterm infants to CPAP pressure of 7–9 cm H 2 O [ 25 ]. Our low level of CPAP support may have resulted to an increased incidence of preterm infants who required reintubation. Future studies should consider evaluation of diaphragmatic thickness and excursion in relation of different modes and parameters of respiratory support to find out the appropriate approach for respiratory support in preterm infants that maintain adequate diaphragmatic stimulation and prevent VIDD.
In conclusion, sonographic assessment of diaphragmatic thickness and excursion represents a promising sensitive and specific easily applicable tool to predict successful extubation of preterm infants from invasive conventional mechanical ventilation.
Abbreviations
Area under the curve
Continuous positive airway pressure
Diaphragmatic thickening fraction
Neonatal intensive care unit
Ventilator induced diaphragmatic dysfunction
Fraction of inspired oxygen
Bhat RY, Greenough A, Rafferty GF, Patel S, Chandler C (2004) Assessment of diaphragm function in lumbocostovertebral syndrome. Eur J Pediatr 163:694–695
PubMed Google Scholar
Buonsenso D, Musolino A (2018) Point of care diaphragm ultrasound in infants with bronchiolitis. Pediatr Pulmonol 53:1597
Article Google Scholar
Dimitriou G, Greenough A, Endo A, Cherian S, Rafferty GF (2002) Prediction of extubation failure in preterm infants. Arch Dis Child Fetal Neonatal Ed 86:F32–F35
Article CAS Google Scholar
DiNino E, Gartman EJ, Sethi JM, McCool FD (2013) Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax 69:423–427
El-Halaby H, Abdel-Hady H, Alsawah G, Abdelrahman A, El-Tahan H (2016) Sonographic evaluation of diaphragmatic excursion and thickness in healthy infants and children. J Ultrasound Med 35:167–175
Farghaly S, Hasan AA (2017) Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care 30:37–43
Fox WW, Schwartz JG, Shaffer TH (1981) Successful extubation of neonates: clinical and physiological factors. Crit Care Med 9:823–826
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D, Brochard LJ, Bolz SS, Rubenfeld GD, Kavanagh BP, Ferguson ND (2015) Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med 41:734
Huang D, Ma H, Zhong W, Wang X, Wu Y, Qin T, Wang S, Tan N (2017) Using M-mode ultrasonography to assess diaphragm dysfunction and predict the success of mechanical ventilation weaning in elderly patients. J Thorac Dis 9:3177–3186
Hussain SN, Cornachione AS, Guichon C, Al Khunaizi A, Leite Fde S, Petrof BJ, Mofarrahi M, Moroz N, de Varennes B, Goldberg P, Rassier DE (2016) Prolonged controlled mechanical ventilation in humans triggers myofibrillar contractile dysfunction and myofilament protein loss in the diaphragm. Thorax 71:436–445
Jaber S, Jung B, Matecki S, Petrof BJ (2011) Clinical review: ventilator-induced diaphragmatic dysfunction—human studies confirm animal model findings! Crit Care 15:206
Kamlin CO, Davis PG, Morley CJ (2006) Predicting successful extubation of very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 91:F180–F183
Kantarci F, Mihmanli I, Demirel MK, Harmanci K, Akman C, Aydogan F, Mihmanli A, Uysal O (2004) Normal diaphragmatic motion and the effects of body composition: determination with M-mode sonography. J Ultrasound Med 23:255–260
Lee EP, Hsia SH, Hsiao HF, Chen MC, Lin JJ, Chan OW, Lin CY, Yang MC, Liao SL, Lai SH (2017) Evaluation of diaphragmatic function in mechanically ventilated children: an ultrasound study. PLoS One 12:e0183560
Li C, Li X, Han H, Cui H, Wang G, Wang Z (2018) Diaphragmatic ultrasonography for predicting ventilator weaning: a meta-analysis. Medicine (Baltimore) 97:e10968
Liu LX, Su D, Hu ZJ (2017) The value of the excursion of diaphragm tested by ultrosonography to predict weaning from mechanical ventilation in ICU patients. Zhonghua Nei Ke Za Zhi 56:495–499
CAS PubMed Google Scholar
McCool FD, Oyieng'o DO, Koo P (2020) The utility of diaphragm ultrasound in reducing time to extubation. Lung 198:499–505
Powers SK, Wiggs MP, Sollanek KJ, Smuder AJ (2013) Ventilator-induced diaphragm dysfunction: cause and effect. Am J Physiol Regul Integr Comp Physiol 305:R464–R477
Radicioni M, Leonardi A, Lanciotti L, Rinaldi VE, Bini V, Camerini PG (2020) How to improve CPAP failure prediction in preterm infants with RDS: a pilot study. Eur J Pediatr: [published online ahead of print, 2020 Jun 19]. Eur J Pediatr. https://doi.org/10.1007/s00431-020-03700-w
Rafferty GF, Greenough A, Dimitriou G, Kavadia V, Laubscher B, Polkey MI, Harris ML, Moxham J (2000) Assessment of neonatal diaphragm function using magnetic stimulation of the phrenic nerves. Am J Respir Crit Care Med 162:2337–2340
Rehan VK, Laiprasert J, Nakashima JM, Wallach M, McCool FD (2001) Effects of continuous positive airway pressure on diaphragm dimensions in preterm infants. J Perinatol 21:521–524
Rehan VK, Laiprasert J, Wallach M, Rubin LP, McCool FD (2001) Diaphragm dimensions of the healthy preterm infant. Pediatrics 108:E91
Shaffer TH, Wolfson MR, Bhutani VK (1981) Respiratory muscle function, assessment, and training. Phys Ther 61:1711–1723
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, Sanchez-de-Toledo J, Brierley J, Colunga JM, Raffaj D, Da Cruz E, Durand P, Kenderessy P, Lang HJ, Nishisaki A, Kneyber MC, Tissieres P, Conlon TW, De Luca D (2020) International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24:65
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, Plavka R, Roehr CC, Saugstad OD, Simeoni U, Speer CP, Vento M, Visser GHA, Halliday HL (2019) European consensus guidelines on the management of respiratory distress syndrome—2019 update. Neonatology 115:432–450
Tapia-Rombo CA, Galindo-Alvarado AM, Saucedo-Zavala VJ, Cuevas-Uriostegui ML (2007) Predictive factors of failure extubation among preterm infants. Gac Med Mex 143:101–108
Vassilakopoulos T, Petrof BJ (2004) Ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med 169:336–341
von Merkel J, Gebauer C, Blaser A, Pulzer F, Thome U, Knupfer M (2012) Prediction of extubation failure in ELBW preterm infants. Klin Padiatr 224:324–330
Wolf GK, Walsh BK, Green ML, Arnold JH (2011) Electrical activity of the diaphragm during extubation readiness testing in critically ill children. Pediatr Crit Care Med 12:e220–e224
Xue Y, Zhang Z, Sheng CQ, Li YM, Jia FY (2019) The predictive value of diaphragm ultrasound for weaning outcomes in critically ill children. BMC Pulm Med 19:270
Yoo JW, Lee SJ, Lee JD, Kim HC (2018) Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success. Korean J Intern Med 33:331–339
Download references
Author information
Authors and affiliations.
Neonatal Intensive Care Unit, Mansoura University Children’s Hospital, Mansoura, Egypt
Eslam Bahgat, Nehad Nasef & Hesham Abdel-Hady
Department of Pediatrics, Faculty of Medicine, University of Mansoura, Mansoura, Egypt
Hanan El-Halaby, Nehad Nasef & Hesham Abdel-Hady
Department of Diagnostic Radiology, Mansoura University Children’s Hospital, Mansoura, Egypt
Ashraf Abdelrahman
Department of Pediatrics, Mansoura University Children’s Hospital, Gomhoria Street, Mansoura, 35516, Egypt
Nehad Nasef
You can also search for this author in PubMed Google Scholar
Contributions
Eslam Bahgat and Hanan El-Halaby participated in the design of the study, data collection, and writing the manuscript. Ashraf Abdelrahman participated in sonographic assessment of the diaphragm and manuscript writing. Nehad Nasef and Hesham Abdel-Hady participated in formulating the hypothesis, design of the study, data collection, data interpretation, statistical analysis, and writing of the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Correspondence to Nehad Nasef .
Ethics declarations
Conflict of interests.
The authors declare that they have no conflict of interest.
Ethical approval
This article has been approved by the Institutional Review Board (IRB), Mansoura Faculty of Medicine, Mansoura, Egypt.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Bahgat, E., El-Halaby, H., Abdelrahman, A. et al. Sonographic evaluation of diaphragmatic thickness and excursion as a predictor for successful extubation in mechanically ventilated preterm infants. Eur J Pediatr 180 , 899–908 (2021). https://doi.org/10.1007/s00431-020-03805-2
Download citation
Received : 05 July 2020
Revised : 22 August 2020
Accepted : 08 September 2020
Published : 28 September 2020
Issue Date : March 2021
DOI : https://doi.org/10.1007/s00431-020-03805-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Preterm infant
- Mechanical ventilation
- Extubation predictor
- Ultrasound waves
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 22 October 2021
Diaphragmatic excursion is correlated with the improvement in exercise tolerance after pulmonary rehabilitation in patients with chronic obstructive pulmonary disease
- Masashi Shiraishi ORCID: orcid.org/0000-0001-5410-1331 1 , 2 ,
- Yuji Higashimoto 1 ,
- Ryuji Sugiya 1 ,
- Hiroki Mizusawa 1 ,
- Yu Takeda 1 ,
- Shuhei Fujita 1 ,
- Osamu Nishiyama 2 ,
- Shintarou Kudo 3 ,
- Tamotsu Kimura 1 ,
- Yasutaka Chiba 4 ,
- Kanji Fukuda 1 ,
- Yuji Tohda 2 &
- Hisako Matsumoto 2
Respiratory Research volume 22 , Article number: 271 ( 2021 ) Cite this article
4447 Accesses
8 Citations
4 Altmetric
Metrics details
In patients with chronic obstructive pulmonary disease (COPD), the maximum level of diaphragm excursion (DE max ) is correlated with dynamic lung hyperinflation and exercise tolerance. This study aimed to elucidate the utility of DE max to predict the improvement in exercise tolerance after pulmonary rehabilitation (PR) in patients with COPD.
This was a prospective cohort study. Of the 62 patients with stable COPD who participated in the outpatient PR programme from April 2018 to February 2021, 50 completed the programme. Six-minute walk distance (6MWD) was performed to evaluate exercise tolerance, and ultrasonography was performed to measure DE max . Responders to PR in exercise capacity were defined as patients who demonstrated an increase of > 30 m in 6MWD. The receiver operating characteristic (ROC) curve was used to determine the cut-off point of DE max to predict responses to PR.
Baseline levels of forced expiratory volume in 1 s, 6MWD, maximum inspiratory pressure, DE max and quadriceps muscle strength were significantly higher, and peak dyspnoea of modified Borg (mBorg) scale score was lower in responders (n = 30) than in non-responders (n = 20) to PR (p < 0.01). In multivariate analysis, DE max was significantly correlated with an increase of > 30 m in 6MWD. The area under the ROC curve of DE max to predict responders was 0.915, with a sensitivity and specificity of 83% and 95%, respectively, at a cut-off value of 44.9 mm of DE max .
DE max could adequately predict the improvement in exercise tolerance after PR in patients with COPD.
Chronic obstructive pulmonary disease (COPD) is a progressive disease characterised by minimally reversible airflow limitation [ 1 ]. The main feature of COPD is the inability of patients to cope with their activities of daily life due to shortness of breath. Although the pathophysiological mechanisms involved in the development of dyspnoea and poor exercise tolerance in patients with COPD are complex, dynamic lung hyperinflation (DLH) plays a central role [ 2 ] by increasing ventilatory workload and decreasing the pressure-generating capacity of the inspiratory muscles.
Pulmonary rehabilitation (PR) is a non-pharmacological intervention and has been reported to improve dyspnoea, exercise capacity and quality of life of patients with COPD [ 3 ]. Owing to a body of evidence, PR is now established as the standard of care for patients with COPD [ 4 ]. However, not all patients with COPD benefit from PR to the same extent. Therefore, identifying patients who are likely to achieve maximum benefit from the PR programme is crucial. So far, several studies have shown that severe airflow limitation or poor exercise tolerance at baseline may predict a better response to PR [ 5 , 6 ], but another study has reported inconsistent findings [ 7 ]. Furthermore, one study reported that patients with severe dyspnoea did not respond well to PR and patients with milder dyspnoea responded well [ 8 ].
Considering the role of DLH in the development of dyspnoea and poor exercise tolerance in patients with COPD, objective measures that reflect the degree of DLH may help in identifying good responders to PR. Previously, we reported that there was an association between increased dyspnoea due to DLH on exercise and decreased exercise capacity in patients with COPD and reduced mobility of the diaphragm, which was assessed by the maximum level of diaphragm excursion (DE max ) using ultrasonography [ 9 ]. Other research groups reported the utility of ultrasonographic assessment of diaphragmatic mobility in COPD in understanding its association with 6-min walk distance (6MWD), dyspnoea [ 10 ] and increased mortality [ 11 ].
However, there have been no reports on the association between diaphragmatic mobility and the effect of PR to improve exercise tolerance. The primary aim of this study is to clarify the role of DE max to predict the improvement in exercise tolerance after PR in patients with COPD.
Materials and methods
Study design and subjects.
This was a single-centre, observational, prospective cohort study. The study included 62 patients with clinically stable COPD who visited the Department of Respiratory Medicine and Allergology, Kindai University Hospital, between April 2018 and February 2021. The exclusion criteria included unstable medical conditions that could cause or contribute to breathlessness, such as metabolic, cardiovascular or other respiratory diseases, or any other disorders that could interfere with exercise testing, such as neuromuscular diseases or musculoskeletal problems. This study was approved by the Ethics Committee of Kindai University School of Medicine. Written informed consent was obtained from all participants.
Measurements
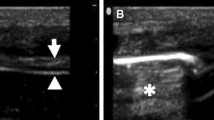
All participants underwent ultrasonography (Xario 200, Toshiba, Tokyo, Japan) for the assessment of their DE max . Using the liver as an acoustic window (Fig. 1 A), a convex 3.5 MHz probe was used to measure the excursions of the right hemidiaphragm according to the techniques mentioned in previous studies [ 9 , 12 , 13 ]. The M-mode cursor was rotated and placed on the axis of diaphragmatic displacement on the stored image, and displacement measurements were performed. Measurements were performed during each of the three deep breaths, and DE max was measured (Fig. 1 B). The maximum value obtained for the three deep breaths was used. 6MWD was performed to evaluate walking capacity according to the American Thoracic Society (ATS)/European Respiratory Society (ERS) statement [ 14 , 15 , 16 ]. All participants performed the 6MWD test before and after the PR programme, and the magnitude of their perceived breathlessness and their leg fatigue was rated using a 1–10-point Borg scale. Responders to PR in exercise capacity were defined as those who demonstrated more than 30 m increase in 6MWD after the PR programme, which was the definition of minimal clinically important difference (MCID) for 6MWD [ 17 ].
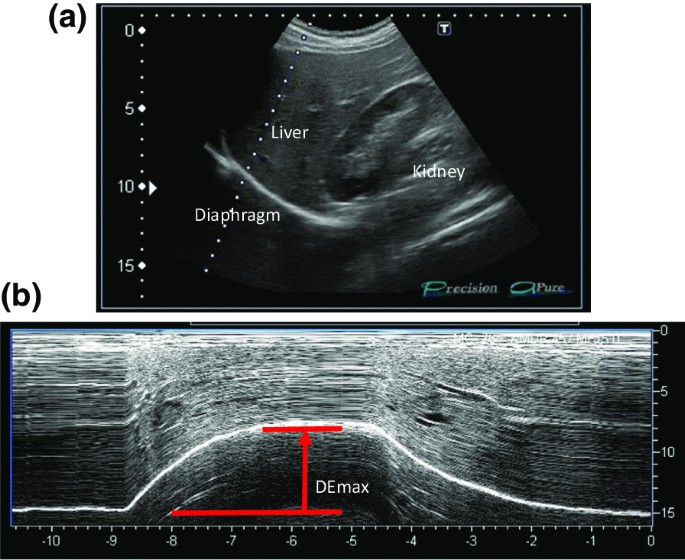
Representative image of the right diaphragm. The probe was positioned below the right costal margin between the midclavicular and anterior axillary lines. A Two-dimensional ultrasonographic image of the right hemidiaphragm (B-mode). Diaphragmatic movements were recorded in M-mode during deep breathing (DE max ) ( B )
Spirometry (CHESTAC-800, Chest, Tokyo, Japan) was performed following the 2005 ATS/ERS recommendations [ 18 ] for measuring forced vital capacity (FVC), forced expiratory volume in 1 s (FEV 1 ) and inspiratory capacity. Respiratory muscle strength was assessed by measuring the maximum inspiratory pressure (PI max ) generated against an occluded airway at residual volume [ 19 ] (SP-370, Fukuda Denshi, Tokyo, Japan). A hand-held dynamometer (μTasF-1, Anima Corp., Tokyo) was used to measure quadriceps muscle strength (QMS). The impact of COPD on health status was assessed using the COPD assessment test (CAT), a patient-completed questionnaire on eight items, namely, cough, phlegm, chest tightness, breathlessness, limited activities, confidence leaving home, sleeplessness and energy. The scores for each of the items range from 0 to 5 points, resulting in a CAT total score ranging from 0 to 40 points [ 20 ], and MCID of CAT is 2 points [ 21 ]. In all patients with COPD, emphysema was evaluated by computed tomography of the chest. A SYNAPSE VINCENT volume analyser (FUJIFILM Medical, Tokyo, Japan) was used to measure the low attenuation area (%LAA).
Rehabilitation programme
The outpatient PR programme was conducted twice a week for 12 weeks (24 sessions), including aerobic exercise training (ergometer and walking exercise) at 60–70% of peak workload for 20–40 min and upper- and lower-limb muscle strength training for 10–20 min.
Sample size
The sample size was estimated using R software. The analysis based on 6MWD data from the PR programme revealed that 40 subjects were required if the expected area under the curve (AUC) below the receiver operating characteristic (ROC) curve was 0.80, the power was 90%, and the significance level was 0.01. Furthermore, we anticipated a dropout from the PR programme. Thus, we set the sample size to 50 participants.
Statistical analysis
Responders and non-responders were compared using t -test, the Wilcoxon rank-sum test or χ 2 test, as appropriate. The paired t -test or the Wilcoxon signed-rank test was used to evaluate the changes in the parameters before and after the PR programme. The Pearson correlation coefficient was used to analyse the relationship between changes in 6MWD and independent variables because changes in 6MWD were normally distributed. Additionally, multivariate logistic regression models were used to assess the ability of variables to predict a response to PR. The ROC curve method was used to assess the ability of DE max to predict a response to PR. All statistical analyses were performed using the JMP software programme (JMP®, Version 14; SAS Institute Inc., Cary, NC, USA).
Out of the 62 patients included in the study, 50 completed the PR programme (Fig. 2 ). Two patients dropped out because of severe exacerbation of COPD, and 10 patients discontinued the PR owing to the coronavirus pandemic. Table 1 presents the baseline characteristics of the participants. After the PR programme, scores for CAT, 6MWD, peak dyspnoea and leg fatigue of the modified Borg (mBorg) scale, and QMS improved significantly (Table 2 ). Thirty patients showed an increase of > 30 m in 6MWD after PR (responders: 60%), and 20 patients (40%) were defined as non-responders. Baseline levels of %FEV 1 , 6MWD, PI max , DE max and QMS were significantly higher and those of CAT score and peak dyspnoea of mBorg scale were significantly lower in responders than in non-responders (Table 1 ). Changes in 6MWD were significantly correlated with baseline levels of CAT, %FEV 1 , peak dyspnoea of mBorg scale, PI max , DE max (Fig. 3 ) and QMS and marginally correlated with baseline levels of 6MWD (Table 3 ).
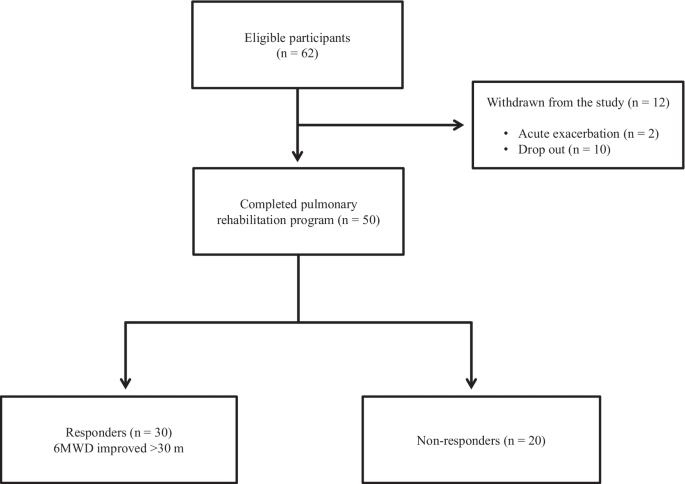
Study flow diagram. COPD chronic obstructive pulmonary disease, PR pulmonary rehabilitation, 6MWD 6-min walk distance
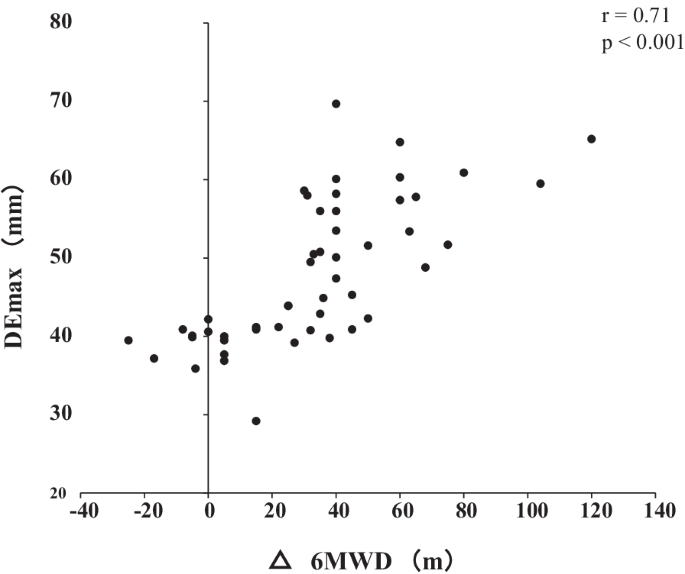
Relationship between DE max and the changes in 6MWD after pulmonary rehabilitation. Changes in 6MWD were significantly positively correlated with DE max (r = 0.72; p < 0.001). DE max maximum diaphragmatic excursion, 6MWD 6-min walk distance
In multivariate analysis, DE max alone significantly contributed to the prediction of responders (Table 4 , Model 1). When using PI max instead of DE max because PI max and DE max showed a strong association (r = 0.73), both PI max and %FEV 1 contributed to the prediction (Table 4 , Model 2). The area under the ROC curve of DE max to predict the responders was 0.915, with a sensitivity of 83% and a specificity of 95% at a cut-off value of 44.9 mm of DE max (Fig. 4 ). The significance of DE max in the predictability of responders remained even when the analysis was confined to severe patients (%FEV 1 < 50%, n = 23; AUC = 0.88, sensitivity = 70% and specificity = 100% at a cut-off value of 44.9 mm).
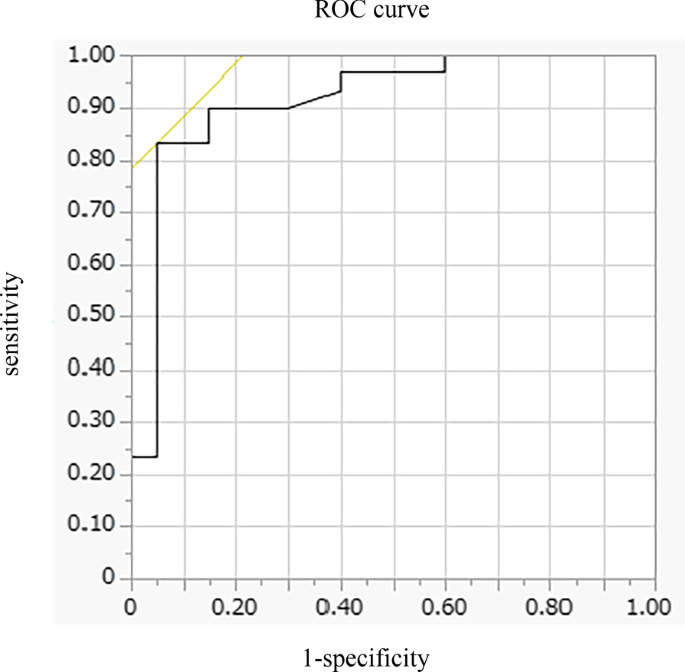
Receiver operating characteristic (ROC) curve for baseline DE max in relation to the response to pulmonary rehabilitation. ROC curve estimates the ability of DE max to predict a clinically important improvement in 6MWD (> 30 m) after pulmonary rehabilitation (AUC = 0.915, sensitivity = 83% and specificity = 95% at a cut-off point of 44.9 mm of DE max ). AUC area under the curve, 6MWD 6-min walk distance, DE max maximum diaphragmatic excursion
This is the first study to demonstrate the utility of DE max to predict the responsiveness of patients with COPD to 12-week PR. In this study, multivariate analysis revealed that greater baseline DE max was the only factor that predicted the responsiveness to PR, independent of baseline %FEV 1 . Additionally, the model using DE max had better prediction performance than that using PI max . The AUC of DE max to predict the 30 m or more improvement in 6MWD after the PR was 0.915, with a sensitivity of 83% and a specificity of 95% at 44.9 mm.
PR is beneficial to patients with chronic respiratory disease, including COPD [ 3 ], and generally improves exercise performance, health-related quality of life and dyspnoea [ 22 ], which was confirmed in this study. Ideally, PR was proven to be effective in all patients, but the response to PR varies considerably between individual patients [ 8 , 23 , 24 , 25 ]. Indeed, in this study, the improvement in 6MWD was less than that in MCID in 40% of the patients regardless of the degree of severity of COPD. Therefore, identifying predictors of a response is crucial in ensuring better PR efficacy and personalisation of PR programmes for patients with COPD.
In this study, the baseline values of %FEV 1 , PI max , DE max , QMS and 6MWD were positively associated with Δ6MWD in univariate analysis, suggesting that a better baseline condition was associated with a higher proportion of patients who achieved MCID after PR. These findings are consistent with those of previous studies that showed that patients with higher levels of %FEV 1 or FEV 1 /VC achieved greater improvement in 6MWD after PR [ 7 , 26 , 27 ] and a study in which patients with milder mMRC scores could achieve MCID of 6MWD after PR [ 8 ], but not for those with worst mMRC score, although others studies showed contradictory results [ 5 , 6 , 28 , 29 , 30 ] or found no significant baseline characteristics to predict a response to PR [ 31 ]. The discrepancy between the findings cannot be fully explained, but it might be due to the differences in the studied population and strength or length of PR. In this study, the mean %FEV 1 of the participants was 56.0%, which was relatively higher than that of other studies (mean %FEV 1 of 40–50% in most studies) [ 5 , 6 , 28 ], despite similar inclusion criteria throughout the studies, i.e., not limited to severe COPD in most studies. Thus, no ceiling effect with a PR programme that included high-intensity load exercise training for 20–40 min was observed in our population.
In this study, an important finding is that greater DE max at baseline was the only factor that predicted the responders in 6MWD after PR. In addition, the model using DE max had better prediction performance than that using PI max . The high predictability of DE max may be because of its strong association with DLH and dyspnoea during exercise, as reported previously [ 9 ]. DLH is involved in the development of dyspnoea, and both are important factors to determine the improvement in 6MWD in patients with COPD. Therefore, DE max that reflects the degree of DLH and dyspnoea during exercise was superior to other physiological indices to predict responders.
Furthermore, the virtuous cycle observed in our PR programme that included high-intensity load exercise training might be a result of the improvement in ventilation pattern. Improving the ventilation pattern would be easier with greater DE max , as shown in studies of mechanically ventilated patients [ 32 ], which may have reduced dyspnoea during exercise after 12 weeks of PR and improved exercise tolerance. Exercise therapy is a central component of PR, which significantly reduces blood lactate levels during exercise, reduces minute ventilation and improves exercise tolerance [ 33 ]. The high-intensity load exercise training, which is performed at 60–80% of the maximum oxygen uptake, has a higher physiological effect than low exercise load. Patients with greater DE max may be able to perform higher load training, which resulted in effective PR.
Diaphragm ultrasonography has been widely and successfully used to identify diaphragmatic dysfunction by showing its association with 6MWD, dyspnoea [ 10 ], extubation failure in mechanically ventilated patients [ 32 ], and increased mortality [ 11 ]. Recently, Lewinska and Shahnazzaryan proposed its use in pulmonary physiotherapy of patients with COPD [ 34 ]. In most previous studies, diaphragm ultrasonography was used to assess DE max , i.e., the measurement of the excursion of the right hemidiaphragm, as used in this study, and diaphragm thickness that assessed the length and thickness of the zone of apposition of the diaphragm against the rib cage [ 35 , 36 ]. However, it is difficult to measure diaphragm thickness in patients with severe COPD because the length of the zone of apposition is shorter in patients with COPD than that in control subjects [ 37 ], whereas it is easy to measure DE max, which shows high intra- and inter-observer reliability [ 38 ]. Bhatt et al. showed that improvement in 6MWD was associated with that in DE max during forced expiration when the effectiveness of pursed lips breathing was assessed in the PR of patients with COPD [ 39 ]. Corbellini et al. demonstrated greater improvement in DE max during inspiration after PR, which was associated with an increase in the inspiratory capacity [ 40 ]. The normal and cut-off values of DE max during normal respiration, forced respiration, and voluntary sniffing have been described for each gender [ 38 ]. Thus, DE max would be a useful and reliable measure for incorporation into the PR assessment. Furthermore, in clinical settings, this objective measure of DE max has additional advantages as it requires minimum effort in patients and can be applied to the PR programme at home if portable ultrasonography is used. However, the assessment of DE max has a limitation. The procedures pertaining to positioning of patients, breathing patterns, and the selected hemidiaphragm are not standardised at present, which may hamper the routine use of DE max at this moment. Standardisation of these parameters would further facilitate the use of DE max in clinical settings and for research purpose.
There are some limitations to this study. This was a single-centre study involving a relatively small number of participants, and their baseline condition might have been relatively preserved. Nonetheless, 46% of the participants showed FEV 1 < 50%, and the utility of DE max was also observed in these patients with severe airflow limitation. Furthermore, in this study, few patients discontinued the PR programme, except for patients who discontinued during the coronavirus pandemic, which indicates that there was no severe mismatch between the PR programme and the patients’ ability to successfully complete this programme. As another limitation, we did not evaluate any malnutrition factors, which could be an important determinant of diaphragmatic mobility. Nonetheless, DE max was a stronger predictor of the effectiveness of PR than other parameters, including QMS or lung function using multivariate analysis. Further studies with a large number of patients are required, and the utility of DE max should be examined in patients with the most severe form of COPD with a low-intensity load exercise programme.
In conclusion, DE max , which is a reliable and easy to perform measurement, could adequately predict the improvement in exercise tolerance after PR in patients with COPD. Assessment of DE max could aid in making medical decisions associated with therapeutic strategies.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Chronic obstructive pulmonary disease
Dynamic lung hyperinflation
- Pulmonary rehabilitation
6-Min walk distance
Minimal clinically important difference
Forced vital capacity
Forced expiratory volume in 1 s
Maximum inspiratory pressure
Quadriceps muscle strength
COPD assessment test
Low attenuation area
Area under the curve
Receiver operating characteristic
Modified Borg
Global initiative for chronic obstructive lung disease (gold). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2020 report. . https://goldcopd.org/gold-reports/ last accessed: 20 Jan 2020.
Gagnon P, Guenette JA, Langer D, Laviolette L, Mainguy V, Maltais F, Ribeiro F, Saey D. Pathogenesis of hyperinflation in chronic obstructive pulmonary disease. Int J COPD. 2014;9:187–201.
Google Scholar
Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188:e13-64.
Article PubMed Google Scholar
Dong J, Li Z, Luo L, Xie H. Efficacy of pulmonary rehabilitation in improving the quality of life for patients with chronic obstructive pulmonary disease: evidence based on nineteen randomized controlled trials. Int J Surg. 2020;73:78–86.
Boutou AK, Tanner RJ, Lord VM, Hogg L, Nolan J, Jefford H, Corner EJ, Falzon C, Lee C, Garrod R, et al. An evaluation of factors associated with completion and benefit from pulmonary rehabilitation in COPD. BMJ Open Respir Res. 2014;1:e000051.
Article PubMed PubMed Central Google Scholar
Costi S, Crisafulli E, Trianni L, Beghe B, Faverzani S, Scopelliti G, Chetta A, Clini E. Baseline exercise tolerance and perceived dyspnea to identify the ideal candidate to pulmonary rehabilitation: a risk chart in COPD patients. Int J Chron Obstruct Pulmon Dis. 2019;14:3017–23.
van Ranst D, Otten H, Meijer JW, van’t Hul AJ. Outcome of pulmonary rehabilitation in COPD patients with severely impaired health status. Int J Chron Obstruct Pulmon Dis. 2011;6:647–57.
Garrod R, Marshall J, Barley E, Jones PW. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J. 2006;27:788–94.
Article CAS PubMed Google Scholar
Shiraishi M, Higashimoto Y, Sugiya R, Mizusawa H, Takeda Y, Fujita S, Nishiyama O, Kudo S, Kimura T, Chiba Y, et al. Diaphragmatic excursion correlates with exercise capacity and dynamic hyperinflation in COPD patients. ERJ Open Res 2020, 6.
Paulin E, Yamaguti WPS, Chammas MC, Shibao S, Stelmach R, Cukier A, Carvalho CRF. Influence of diaphragmatic mobility on exercise tolerance and dyspnea in patients with COPD. Respir Med. 2007;101:2113–8.
Yamaguti WPdS, Paulin E, Salge JM, Chammas MC, Cukier A, de Carvalho CRF. Diaphragmatic dysfunction and mortality in patients with COPD. J Bras Pneumol. 2009;35:1174–81.
Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values. Chest. 2009;135:391–400.
Testa A, Soldati G, Giannuzzi R, Berardi S, Portale G, Gentiloni Silveri N. Ultrasound M-Mode assessment of diaphragmatic kinetics by anterior transverse scanning in healthy subjects. Ultrasound Med Biol. 2011;37:44–52.
Laboratories ATSCoPSfCPF. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Article Google Scholar
Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, McCormack MC, Carlin BW, Sciurba FC, Pitta F, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1428–46.
Singh SJ, Puhan MA, Andrianopoulos V, Hernandes NA, Mitchell KE, Hill CJ, Lee AL, Camillo CA, Troosters T, Spruit MA, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014;44:1447–78.
Polkey MI, Spruit MA, Edwards LD, Watkins ML, Pinto-Plata V, Vestbo J, Calverley PMA, Tal-Singer R, Agustí A, Bakke PS, et al. Six-minute-walk test in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187:382–6.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38.
Lisboa C, Munoz V, Beroiza T, Leiva A, Cruz E. Inspiratory muscle training in chronic airflow limitation: comparison of two different training loads with a threshold device. Eur Respir J. 1994;7:1266–74.
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–54.
Kon SSC, Canavan JL, Jones SE, Nolan CM, Clark AL, Dickson MJ, Haselden BM, Polkey MI, Man WDC. Minimum clinically important difference for the COPD Assessment Test: a prospective analysis. Lancet Respir Med. 2014;2:195–203.
Lacasse Y, Goldstein R, Lasserson TJ, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006:CD003793.
Spruit MA, Gosselink R, Troosters T, Kasran A, Van Vliet M, Decramer M. Low-grade systemic inflammation and the response to exercise training in patients with advanced COPD. Chest. 2005;128:3183–90.
de Torres JP, Pinto-Plata V, Ingenito E, Bagley P, Gray A, Berger R, Celli B. Power of outcome measurements to detect clinically significant changes in pulmonary rehabilitation of patients with COPD. Chest. 2002;121:1092–8.
Troosters T, Gosselink R, Decramer M. Exercise training in COPD: how to distinguish responders from nonresponders. J Cardiopulm Rehabil. 2001;21:10–7.
Vagaggini B, Costa F, Antonelli S, De Simone C, De Cusatis G, Martino F, Santerini S, Paggiaro P. Clinical predictors of the efficacy of a pulmonary rehabilitation programme in patients with COPD. Respir Med. 2009;103:1224–30.
Scott AS, Baltzan MA, Fox J, Wolkove N. Success in pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Can Respir J. 2010;17:219–23.
Crisafulli E, Gorgone P, Vagaggini B, Pagani M, Rossi G, Costa F, Guarriello V, Paggiaro P, Chetta A, de Blasio F, et al. Efficacy of standard rehabilitation in COPD outpatients with comorbidities. Eur Respir J. 2010;36:1042–8.
Zanini A, Chetta A, Gumiero F, Della Patrona S, Casale S, Zampogna E, Aiello M, Spanevello A. Six-minute walking distance improvement after pulmonary rehabilitation is associated with baseline lung function in complex COPD patients: a retrospective study. Biomed Res Int. 2013;2013:1–6.
Ragaselvi S, Janmeja AK, Aggarwal D, Sidana A, Sood P. Predictors of response to pulmonary rehabilitation in stable chronic obstructive pulmonary disease patients: a prospective cohort study. J Postgrad Med. 2019;65:101–6.
CAS PubMed PubMed Central Google Scholar
Selzler A-M, Simmonds L, Rodgers WM, Wong EYL, Stickland MK. Pulmonary rehabilitation in chronic obstructive pulmonary disease: predictors of program completion and success. COPD J Chronic Obstr Pulm Dis. 2012;9:538–45.
Li C, Li X, Han H, Cui H, Wang G, Wang Z. Diaphragmatic ultrasonography for predicting ventilator weaning: a meta-analysis. Medicine (Baltimore). 2018;97:e10968.
Rabinovich RA, Ardite E, Troosters T, Carbo N, Alonso J, Gonzalezde Suso JM, Vilaro J, Barbera JA, Polo MF, Argiles JM, et al. Reduced muscle redox capacity after endurance training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164:1114–8.
Lewinska A, Shahnazaryan K. The use of diaphragm ultrasonography in pulmonary physiotherapy of COPD patients: a literature review. J Clin Med 2020; 9.
Gibson GJ, Whitelaw W, Siafakas N, Supinski GS, Fitting JW, Bellemare F, Loring SH, Troyer AD, Grassino AE. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166:518–624.
Summerhill EM, El-Sameed YA, Glidden TJ, McCool FD. Monitoring recovery from diaphragm paralysis with ultrasound. Chest. 2008;133:737–43.
McKenzie DK, Butler JE, Gandevia SC. Respiratory muscle function and activation in chronic obstructive pulmonary disease. J Appl Physiol. 2009;107:621–9.
Laveneziana P, Albuquerque A, Aliverti A, Babb T, Barreiro E, Dres M, Dubé BP, Fauroux B, Gea J, Guenette JA, et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J 2019; 53.
Bhatt SP, Luqman-Arafath TK, Gupta AK, Mohan A, Stoltzfus JC, Dey T, Nanda S, Guleria R. Volitional pursed lips breathing in patients with stable chronic obstructive pulmonary disease improves exercise capacity. Chron Respir Dis. 2013;10:5–10.
Corbellini C, Boussuges A, Villafane JH, Zocchi L. Diaphragmatic mobility loss in subjects with moderate to very severe COPD may improve after in-patient pulmonary rehabilitation. Respir Care. 2018;63:1271–80.
Download references

Acknowledgements
Not applicable.
This work was supported by Grants-in-Aid for Scientific Research (21K11325).
Author information
Authors and affiliations.
Department of Rehabilitation Medicine, Kindai University School of Medicine, 377-2 Onohigashi, Osakasayama, Osaka, 5898511, Japan
Masashi Shiraishi, Yuji Higashimoto, Ryuji Sugiya, Hiroki Mizusawa, Yu Takeda, Shuhei Fujita, Tamotsu Kimura & Kanji Fukuda
Department of Respiratory Medicine and Allergology, Kindai University School of Medicine, Osaka, Japan
Masashi Shiraishi, Osamu Nishiyama, Yuji Tohda & Hisako Matsumoto
Inclusive Medical Science Research Institute, Morinomiya University of Medical Sciences, Osaka, Japan
Shintarou Kudo
Division of Biostatistics, Clinical Research Center, Kindai University School of Medicine, Osaka, Japan
Yasutaka Chiba
You can also search for this author in PubMed Google Scholar
Contributions
MS, YH, and YC made substantial contributions to the conception and design of the work. MS, YH, and RS made substantial contributions to the data acquisition. MS and HM made substantial contributions to the analysis. All of the listed authors designed the study and were involved in the interpretation of the data. MS and HM drafted the work. YH, MS, TK, YC, ON, KS, KF, YT, and HM revised the report critically for important intellectual content. All authors approved the final version to be published and agreed to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Masashi Shiraishi .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of Kindai University School of Medicine (31-086). Written informed consent was obtained from all participants.
Consent for publication
If the manuscript is accepted, we approve it for publication in Respiratory Research.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shiraishi, M., Higashimoto, Y., Sugiya, R. et al. Diaphragmatic excursion is correlated with the improvement in exercise tolerance after pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Respir Res 22 , 271 (2021). https://doi.org/10.1186/s12931-021-01870-1
Download citation
Received : 09 July 2021
Accepted : 15 October 2021
Published : 22 October 2021
DOI : https://doi.org/10.1186/s12931-021-01870-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diaphragmatic excursion
- Six-minute walk distance (6MWD)
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
- Open access
- Published: 28 February 2019
A narrative review of diaphragm ultrasound to predict weaning from mechanical ventilation: where are we and where are we heading?
- Peter Turton ORCID: orcid.org/0000-0001-7974-3031 1 , 2 ,
- Sondus ALAidarous 1 , 3 &
- Ingeborg Welters 1 , 2
The Ultrasound Journal volume 11 , Article number: 2 ( 2019 ) Cite this article
17k Accesses
29 Citations
53 Altmetric
Metrics details
The use of ultrasound to visualize the diaphragm is well established. Over the last 15 years, certain indices of diaphragm function, namely diaphragm thickness, thickening fraction and excursion have been established for mechanically ventilated patients to track changes in diaphragm size and function over time, to assess and diagnose diaphragmatic dysfunction, and to evaluate if these indices can predict successful liberation from mechanical ventilation. In the last 2 years, three meta-analyses and a systematic review have assessed the usability of diaphragmatic ultrasound to predict successful weaning. Since then, further data have been published on the topic.
Conclusions
The aim of this narrative review is to briefly describe the common methods of diaphragmatic function assessment using ultrasound techniques, before summarizing the major points raised by the recent reviews. A narrative summary of the most recent data will be presented, before concluding with a brief discussion of future research directions in this field.
There has been much interest in the use of diaphragm ultrasound as a tool of measuring and tracking atrophy, in particular to identify patients who will wean from mechanical ventilation, and who will remain free of ventilatory support afterwards. Two meta-analyses and a systematic review have been published on the topic in the last 2 years, and more work is being produced. The aim of this narrative review is briefly re-iterate what is being measured with diaphragm ultrasound, to summarize the most recent findings from these reviews and meta-analyses, and to provide an update of current work produced after these reviews.
The diaphragm in critical care: what do we know?
The effects of atrophy of the diaphragm secondary to mechanical ventilation have been recently described; Goligher found that the development of diaphragm atrophy was associated with prolonged duration of mechanical ventilation, increased ICU length of stay, and a higher rate of complications [ 1 ]. Interestingly, patients who showed an increase in diaphragmatic thickness during their critical illness were also at higher risk of prolonged mechanical ventilation, with excessive respiratory effort as a possible underlying trigger. The authors did acknowledge that tissue oedema from fluid resuscitation may also contribute to this thickening. Diaphragmatic thickness has been shown to reduce by 6% [ 2 ] or 7.5% [ 3 ] per day in mechanically ventilated patients. However, a further study demonstrated that although nearly half of the patients in their study did suffer atrophy, the same proportion experienced no loss, and a further 10% actually had increases in diaphragmatic thickness [ 4 ]. A recent study in mechanically ventilated children suggested that diaphragmatic atrophy occurs at an average rate of 3.4% per day and is worsened by the use of neuromuscular blockade [ 5 ]. However, two papers failed to demonstrate diaphragmatic atrophy using ultrasound [ 6 , 7 ]. However, one of these studies was in extubated survivors of sepsis (82% of which had either severe sepsis or septic shock) who were approached after a period of at least 5 days of mechanical ventilation, compared to controls. However, the authors concede that these results were based on a single measurement at a point in the patients’ recovery from sepsis rather than during the acute episode.
Ultrasound and the diaphragm
Visualization of the diaphragm with ultrasound has been possible for well over 40 years [ 8 ]. However, only recently diaphragmatic ultrasound has been used to assess diaphragm function and size during mechanical ventilation. There are two commonly used measurements derived from ultrasound: diaphragm excursion and diaphragm thickness [ 9 ]. Diaphragm excursion is usually measured using a phased array probe, with the probe positioned in the subcostal margin in the mid-clavicular line, with the aim of imaging the posterior third of the diaphragm (Fig. 1 ). Although some studies have used B-mode imaging to determine diaphragmatic excursion [ 10 ], the use of M-mode produces images that visualize the movement of the diaphragm over time and allows accurate measurement of diaphragmatic displacement over a respiratory cycle (Figs. 2 and 3 ) [ 11 ]. In healthy volunteers, diaphragmatic excursion is known to vary with sex and height and can be reliably performed in a recumbent or supine position [ 12 ]. Excursion is known to positively correlate with lung inspiratory volumes [ 13 , 14 ], and is higher during forced inspiratory breathing [ 10 ].
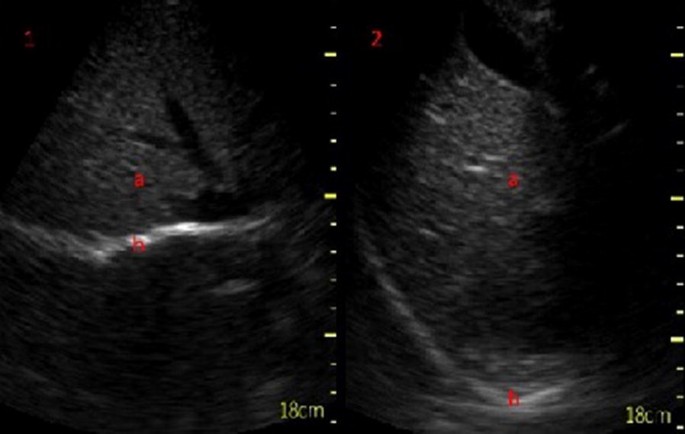
Subcostal view of the diaphragm (b) in B-mode at end inspiration (1) and at expiration (2) seen below the liver (a)
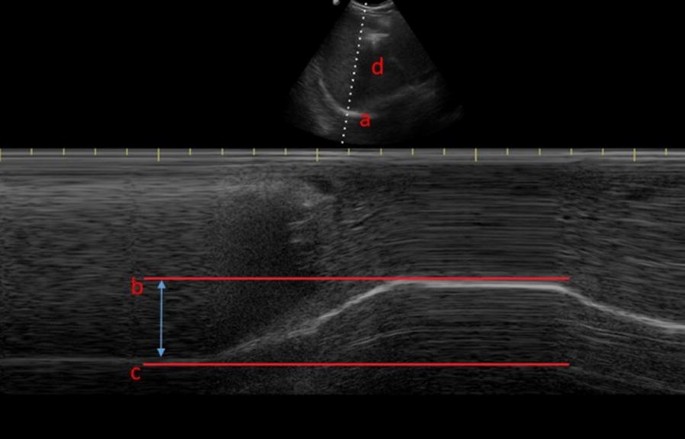
Diaphragm excursion as assessed via M-mode ultrasonography, where a is the diaphragm, b is at the end of a deep inspiratory effort, c is at end expiration and d is the liver

M-mode ultrasonography demonstrating three tidal inspiratory efforts ( a ) and a deep inspiratory effort ( b )
Diaphragm thickness is measured in the zone of apposition, using a higher-frequency (> 10 MHz) linear probe, to view the diaphragm as a three-layered structure, sandwiched between the two echogenic layers of the pleura and the peritoneum (Fig. 4 ) [ 15 ]. Both B- and M-mode techniques can be used to measure thickness [ 16 ]. Diaphragm thickness has been previously correlated with the strength of the diaphragm [ 17 ], but not the endurance or fatigability [ 18 ]. It appears to be thicker in an upright position, compared to supine posture [ 19 ], can be measured at expiration or end inspiration, and in both tidal and maximal breathing. Comparing expiratory with inspiratory thickness gives the thickening fraction, which is usually denoted as [(End Inspiratory Thickness − End Expiratory Thickness)/End Expiratory Thickness] [ 20 ] and is an indicator of the work of breathing [ 21 ]. These measurements can be used to form a definition of diaphragm dysfunction, although there is variation in this definition: It has been defined as a thickening fraction of less than 20% or a tidal excursion of less than 10 mm [ 22 ], based on the presence of paradoxical movement in the case of the paralyzed diaphragm [ 9 ], or using non-ultrasound methods such as measurement of twitch pressures [ 23 ]. Regardless, ultrasound techniques have been shown to outperform traditional techniques such as fluoroscopy in diagnosing diaphragm dysfunction [ 24 ].
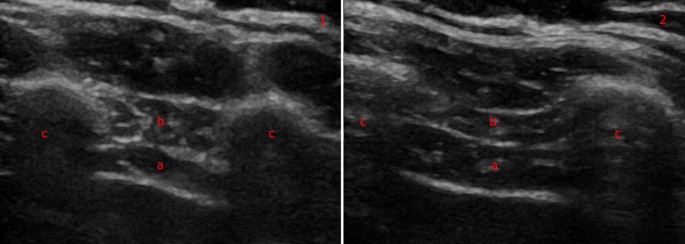
Diaphragm thickness in B-mode thoracic view at end expiration (1) and inspiration (2) in a heathy volunteer. The diaphragm can be seen between two echogenic layers (a) with the intercostal compartment above (b). The two muscle layers sit between two ribs ( c )
Summary of current literature
In 2017, a systematic review [ 25 ] and a meta-analysis [ 26 ] have been performed, assessing the evidence on diaphragm ultrasound and its ability to predict successful weaning from mechanical ventilation. Two further meta-analyses have been published in 2018 [ 27 , 28 ], and together these reviews assessed the combined work of more than 30 individual papers (excluding further 3 papers that looked exclusively at lung rather than diaphragm ultrasound).
The systematic review [ 25 ] focused on the use of diaphragmatic ultrasound in four key areas: to diagnose diaphragmatic dysfunction, to predict successful weaning from mechanical ventilation, to determine if ultrasound can assess muscular workload against other known measurements such as transdiaphragmatic pressure [ 29 ], and to describe variations in diaphragm atrophy across studies.
With respect to weaning from mechanical ventilation, four studies were analyzed, two of which described diaphragm excursion either by M-mode ultrasound [ 30 ] or by measuring organ displacement [ 31 ]. The two remaining studies assessed diaphragmatic thickening fraction [ 32 , 33 ]. All four studies concluded that their respective measurements can predict successful extubation or weaning failure, with cut-off values of 11–14 mm in excursion and 30–36% in thickening fraction being most sensitive and specific.
The three meta-analyses are broadly similar in their aims and results. A possible reason may lie in the slight differences to the selection criteria; Li et al. reviewed only publications in English and defined weaning failure as the requirement for re-intubation within 48 h, whereas Llamas-Álverez et al. included publications in all languages and had a much broader definition of weaning failure to include death, unscheduled non-invasive ventilation, tracheostomy formation or the failure of a spontaneous breathing trial within 72 h, and Qian defined weaning failure more broadly as a failed spontaneous breathing trial, re-intubation, the use of non-invasive ventilation, or death. Li and Llamas-Álverez found similar AUC characteristics for the use of diaphragm thickening fraction (0.83 versus 0.87). Llamas-Álverez et al. concluded that thickening fraction may help to predict weaning failure, and Li et al. concluded that the either measurement is suitable to predict successful extubation. Qian found that pooled specificity for predicting weaning success was similar to the work of Llamas-Álverez, and also found that weaning failure was higher in the presence of diaphragmatic dysfunction, and that both excursion and thickening fraction were higher in patients who were successfully weaned.
All papers acknowledge the heterogeneity in the studies analyzed. The definition of weaning failure varied amongst individual studies, with re-intubation limits set at either 48 or 72 h, and some studies included the use of non-invasive ventilation to define weaning failure. Inclusion criteria are different for each of the studies; while some studies recruited patients during their first spontaneous breathing trial [ 32 ], another study included only patients who had already had a failed trial [ 33 ]. Further differences arise from the ultrasonic technique chosen; in Li’s meta-analysis, 4 of the studies were conducted with the patient in a supine position, while patients were semi-recumbent in the remaining 9 studies. Although probe position was consistent in all studies, probe frequency and ultrasound machine manufacturer varied considerably, with 12 different types of ultrasound machines being used, covering a range of frequencies from 3.5 to 10 MHz. There is also variation in the patient populations, particularly with respect to age and sex. It is known that age negatively correlates with excursion in deep breathing, and that females have less diaphragmatic excursion [ 12 ]. Many of the studies included both left and right sides of the diaphragm, but some reported measurements of the right side only, probably because there is greater difficulty in imaging the left diaphragm due to the lung obscuring the view [ 13 ]. Finally, there is variation regarding the time point during a spontaneous breathing trial at which measurements are taken, with ultrasound images being obtained at the start or end of spontaneous breathing; some investigators assessed diaphragmatic function after extubation, others during mechanically ventilation with further variation in the ventilatory mode used. It has been suggested that pre-extubation is the best time to perform diaphragm ultrasound to assess the diaphragm at a time point when it may be fatigued. A protocol for a new study performing ultrasounds at regular intervals throughout 2 h of spontaneous breathing has been published, but the results are not yet available [ 34 ].
Where are we now?
Since the publication of the systematic reviews, several studies have reported diaphragmatic ultrasound parameters as a means of predicting extubation success. Our search strategy used MEDLINE only; we searched for papers published after 1st January 2017 until to the current date of writing (August 2018). Using the search string (Ultraso* AND Diaphagm* AND (critical* OR intensive OR sepsis OR mechanical * OR ventilat*) yielded 89 results. After having excluded papers that already appeared in the four systematic reviews and papers covering different topics as assessed on title and/or abstract), we identified 18 new papers since 2017 that have not been part of a systematic review.
Newer studies
Newly identified studies can be divided into three categories. In the first, there are studies in which diaphragm thickening or excursion are used alone to predict successful weaning. In the second, diaphragm ultrasound is compared to another technique; and in the third, these techniques are combined to see if they increase predictive accuracy.
A recent study describes cut-offs for diaphragm thickening to predict successful weaning prior to a spontaneous breathing trial [ 35 ]. Its results are in keeping with previously established cut-offs for patients weaning from pressure support [ 36 ]. However, there are also conflicting results. For example, a study evaluating diaphragm excursion using spleen and liver displacement found that displacement of the organs by 1.2 cm was the best cut-off for predicting successful extubation [ 37 ]. However, poor agreement between solid organ movement and diaphragm excursion has been described before [ 38 ]. Another recent study found that diaphragmatic excursion, and not thickening fraction, was the best predictor of extubation failure in patients undergoing their first spontaneous breathing trial [ 39 ]. The most recent reliability study has established values of inter- (0.987) and intra-observer variability (0.986) that are within the higher range of Intra Class Correlation (ICC) coefficients established in the systematic review [ 40 ].
Newer studies—comparative approaches
Dres and colleagues compared the performance of diaphragm ultrasound against tracheal pressure measurements obtained during supra-maximal phrenic nerve stimulation during a spontaneous breathing trial [ 23 ]. They not only found that a lower stimulated pressure than previously accepted was associated with optimum sensitivity and specificity for liberation from mechanical ventilation [ 41 ], but also described that a thickening fraction of greater than 25.8% gave equivalent accuracy of prediction in comparison to phrenic nerve stimulation, with AUC–ROC values of 0.80 and 0.82 for phrenic nerve stimulation and diaphragm thickening fraction, respectively.
Newer studies—combined approaches
Combining diaphragmatic ultrasound with echocardiography may be a promising route for prediction of successful weaning, particularly in view of potential cardiac causes for a failed respiratory wean [ 42 ]. The ratio of mitral Doppler inflow velocity (E) to annular tissue Doppler wave velocity (Ea, E /Ea ratio) has been measured with transthoracic echocardiography alongside diaphragmatic excursion in patients who were extubated after a successful spontaneous breathing trial (SBT) [ 43 ]. The authors found that respiratory failure within 48 h of extubation could be predicted from both E /Ea and left ventricular ejection fraction values, but that reintubation within a week of extubation was more accurately predicted by diaphragmatic excursion.
Another study combined echocardiography with lung ultrasound and assessment of diaphragmatic excursion to assess if all three combined could predict extubation failure in patients undergoing a trial of pressure support ventilation [ 44 ]. The results were confirmed in a smaller sub-study of patients breathing via a T-tube, although out of the three modalities, diaphragm ultrasound contributed least predicting successful weaning. Furthermore, a recent small observational study has combined echocardiography and lung ultrasound for assessment of aeration with diaphragmatic ultrasound, and reported that lung aeration and markers of diastolic dysfunction were the only strong predictors of successful extubation [ 45 ].
Another combined approach combined diaphragm thickening fraction with the Rapid Shallow Breathing Index (RSBI). First described in 1991 [ 46 ], RSBI is defined as the ratio of the respiratory frequency to the tidal volume [ 47 ], with a cut-off value of 100–105 breaths/min/liter being associated with successful extubation [ 46 , 48 ]. A recent study found that RSBI alone, in comparison to measurements derived from diaphragm ultrasound, was most accurate in predicting success of extubation, with an ROC–AUC of 0.96 and a sensitivity and specificity of 100% [ 49 ]. This supports earlier work that the sensitivity, specificity and positive predictive value of a thickening fraction cut-off 36% were comparable to RSBI, but ultimately lower than it [ 33 ]. However, the combination of RSBI with diaphragm thickening fraction of greater than 26% was a more accurate predictor of successful weaning from mechanical ventilation than RSBI alone [ 50 ]. The authors concluded that thickening fraction of the right diaphragm alone was as accurate as this combined approach, and suggested that thickening fraction could replace RSBI as the most commonly used weaning parameter in the future.
Future directions
As ultrasound technology progresses, it may be possible for clinicians to estimate diaphragm thickness and excursion using portable, hand-held devices. A recent study used both linear and phased arrays probes of a hand-held ultrasound device to assess diaphragmatic thickness and excursion, respectively, compared to a standard ultrasound device [ 22 ]. Good agreement was noted between the two devices, with ICCs of greater than 0.9 noted in all indices of measurement except for maximal excursion. Based on a definition of diaphragmatic dysfunction as tidal excursion of less than 10 mm, the detection of dysfunction was comparable between the two devices, and good inter-rater reliability was also seen. Stronger agreement between the two devices was seen in the measurement of diaphragm thickness compared to measurement of excursion, possibly because of the hand-held device lacking an M-mode for accurate measurement of excursion.
A third measurement, the contraction velocity, has also been evaluated recently. Contraction velocity is an extension of diaphragm excursion, dividing excursion by the time to reach maximal excursion [ 9 ]. None of the systematic reviews assessed contraction velocity in the prediction of successful weaning. A study of elderly ventilated patients found that right-sided contraction velocity had a similar AUC as right-sided excursion (labeled in the study as diaphragmatic motion), and that both of these were more predictive for successful weaning from mechanical ventilation than RSBI [ 51 ]. Contraction velocity has been shown to have high sensitivity and specificity, and only performed slightly worse than RSBI in a study of younger patients [ 49 ]. A more recent study, however, found that there was no difference in contraction velocity between patients who were successfully extubated, compared to those who were re-intubated [ 52 ]. It is not clear why there is such variation in results, and further research on conduction velocity is required, along with standardization whether velocity is measured over tidal or maximal inspiratory efforts. The same authors found that multiplying the diaphragmatic excursion ( E ) by the inspiratory time ( I ) to give a diaphragmatic excursion-time index gave values that were significantly higher in patients who had been successfully extubated compared to those who failed extubation [ 53 ]. The differences were still significant regardless as to whether the measurements were performed during spontaneous breathing or after extubation. However, significance was lost during pressure-assist ventilation modes.
Speckle tracking can detect tissue motion and distortion [ 54 ]. In healthy volunteers, it has been used to successfully assess diaphragmatic strain under pressure support ventilation [ 55 ] and was weakly but significantly associated with caudal diaphragm displacement [ 56 ]. This technique may provide useful information about the diaphragm during controlled mechanical ventilation, but as yet, there are no studies examining speckle tracking in the critical care population. Similarly, an “area method” [ 57 ] assessing diaphragm motion in two dimensions, correlates with lung volume using both B and M-mode ultrasound in healthy volunteers, and can be performed on both sides of the chest.
Further research focuses on the prediction of successful extubation in particular patient groups. For example, a recent study demonstrated that diaphragm thickness measured before anesthetic induction correlates with time to extubation in patients undergoing liver transplants. Time to extubation after the procedure was higher in patients with pre-operative end expiratory diaphragm thickness of less than 2 mm [ 58 ].
In patients with Chronic Obstructive Pulmonary Disease (COPD), diaphragmatic ultrasound may predict successful weaning on one side, but could also serve to predict success of non-invasive ventilation. In this context, it has been reported that COPD patients with diaphragm dysfunction (diagnosed by a thickening fraction of less than 20%), who require non-invasive ventilation, were 4.4 times more likely to need intubation, more often proceeded to tracheostomies, and had increased length of stay in ICU and hospital mortality [ 59 ]. These results were in line with an earlier smaller study that also described an association of diaphragm dysfunction with Non-Invasive Ventilation (NIV) failure and increased mortality [ 60 ]. However, reduced diaphragmatic thickening itself is not a risk factor for acute exacerbation of COPD [ 61 ].
Diaphragmatic ultrasound has been extensively studied as a predictor of successful weaning from mechanical ventilation, and continues to be studied. It remains difficult to draw general conclusions from individual studies due to the marked variation in study design and population. Even, definitions such as a failed breathing trial or failed extubation have not been standardized across studies, rendering comparison between outcome measures impossible. As yet, defined cut-offs for measurements of diaphragmatic ultrasound have been agreed, and there are no randomized control trials available. Although diaphragmatic ultrasound is a promising diagnostic tool, greater standardization of protocols, outcome measures and ventilatory settings is required for further research and clinical application.
Abbreviations
area under the curve
area under the curve (receiver-operator characteristic)
Chronic Obstructive Pulmonary Disease
intra-class correlation coefficient
intensive care unit
non-invasive ventilation
spontaneous breathing trial
Rapid Shallow Breathing Index
Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS et al (2018) Mechanical ventilation–induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med 197:204–213
Article CAS Google Scholar
Grosu HB, Lee YI, Lee J, Eden E, Eikermann M, Rose KM (2012) Diaphragm muscle thinning in patients who are mechanically ventilated. Chest 142:1455–1460
Article Google Scholar
Zambon M, Beccaria P, Matsuno J (2016) Mechanical ventilation and diaphragmatic atrophy in critically ill patients: an ultrasound study. Crit Care Med 43:29–38
Google Scholar
Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brade D et al (2015) Evolution of diaphragm thickness during mechanical ventilation. impact of inspiratory effort. Am J Respir Crit Care Med 192:1080–1088
Glau CL, Conlon TW, Himebauch AS, Yehya N, Weiss SL, Berg RA et al (2018) Progressive diaphragm atrophy in pediatric acute respiratory failure. Pediatr Crit Care Med 19:406–411
Cartwright MS, Kwayisi G, Griffin LP, Sarwal A, Walker FO, Harris JM et al (2013) Quantitative neuromuscular ultrasound in the intensive care unit. Muscle Nerve 47:255–259
Baldwin CE, Bersten AD (2014) Alterations in respiratory and limb muscle strength and size in patients with sepsis who are mechanically ventilated. Phys Ther 94:68–82
Doust BD, Baum JK, Maklad NF, Doust VL (1975) Ultrasonic evaluation of pleural opacities. Radiology 114:135–140
Matamis D, Soilemezi E, Tsagourias M, Akoumianaki E, Dimassi S, Boroli F et al (2013) Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med 39:801–810
Testa A, Soldati G, Giannuzzi R, Berardi S, Portale G, Gentilone Silveri N et al (2011) Ultrasound M-mode assessment of diaphragmatic kinetics by anterior transverse scanning in healthy subjects. Ultrasound Med Biol 37:44–52
Houston JG, Morris AD, Howie CA, Reid JL (1992) Technical report: quantitative assessment of diaphragmatic movement-A reproducible method using ultrasound quantitative assessment of diaphragmatic movement a reproducible method using ultrasound. Clin Radiol 46:405–407
Scarlata S, Mancini D, Laudisio A, Benigni A, Antonellia Incalzi R (2018) Reproducibility and clinical correlates of supine diaphragmatic motion measured by M-mode ultrasonography in healthy volunteers. Respiration 96:259–266
Boussuges A, Gole Y, Blanc P (2009) Diaphragmatic motion studied by M-mode ultrasonography: methods, reproducibility, and normal values. Chest 135:391–400
Houston JG, Angus RM, Cowan MD, McMillan NC, Thomson NC, Houston M et al (1994) Ultrasound assessment of normal hemidiaphragmatic movement: relation to inspiratory volume. Thorax 49:500–503
Haji K, Royse A, Green C, Botha J, Canty D, Royse C (2016) Interpreting diaphragmatic movement with bedside imaging, review article. J Crit Care 34:56–65
Boon AJ, Harper CJ, Ghahfarokhi LS, Strommen JA, Watson JC, Sorenson EJ (2013) Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve 47:884–889
Cardenas LZ, Santana PV, Caruso P, Ribeiro de Carvalho CR, Pereira de Albuquerque AL (2018) Diaphragmatic ultrasound correlates with inspiratory muscle strength and pulmonary function in healthy subjects. Ultrasound Med Biol 44:786–793
Holtzhausen S, Unger M, Lupton-Smith A, Hanekom S (2018) An investigation into the use of ultrasound as a surrogate measure of diaphragm function. Heart Lung 47:418–424
Hellyer NJ, Andreas NM, Bernstetter AS, Cieslak KR, Donahue GF, Steiner EA et al (2017) Comparison of diaphragm thickness measurements among postures via ultrasound imaging. PM&R 9:21–25
Vivier E, Roche-Campo F, Brochard L, Mekontso Dessap A (2017) Determinants of diaphragm thickening fraction during mechanical ventilation: an ancillary study of a randomised trial. Eur Respir J 50:1700783
Vivier E, Dessap AM, Dimassi S, Vargas F, Lyazidid A, Thille AW et al (2012) Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensive Care Med 38:796–803
Gursel G, Inci K, Alasgarova Z (2018) Can diaphragm dysfunction be reliably evaluated with pocket-sized ultrasound devices in intensive care Unit? Crit Care Res Pract. Article ID: 5192647
Dres M, Goligher EC, Dubé B-P, Morawiec E, Dangers L, Reuter D et al (2018) Diaphragm function and weaning from mechanical ventilation: an ultrasound and phrenic nerve stimulation clinical study. Ann Intensive Care 8:53
Houston JG, Fleet M, Cowan MD, McMillan NC (1995) Comparison of ultrasound with fluoroscopy in the assessment of suspected hemidiaphragmatic movement abnormality. Clin Radiol 50:95–98
Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrillo A (2017) Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med 43:29–38
Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J (2017) Diaphragm and lung ultrasound to predict weaning outcome. Chest 152:1140–1150
Li C, Li X, Han H, Cui H, Wang G, Wang Z (2018) Diaphragmatic ultrasonography for predicting ventilator weaning: a meta-analysis. Medicine (Baltimore) 97:e10968
Qian Z, Yang M, Li L, Chen Y (2018) Ultrasound assessment of diaphragmatic dysfunction as a predictor of weaning outcome from mechanical ventilation: a systematic review and meta-analysis. BMJ Open 8:21189
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D et al (2015) Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med 41:642–649
Kim Y, Hee HJ, Suh J, Hong RSB, Koh Y, Lim CM (2011) Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 39:2627–2630
Jiang JR, Tsai TH, Jerng JS, Yu CJ, Wu HD, Yang PC (2004) Ultrasonographic evaluation of liver/spleen movements and extubation outcome. Chest 126:179–185
Dinino E, Gartman EJ, Sethi JM, Mccool D (2014) Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax 69:423–427
Ferrari G, De Filippi G, Fabrizio E, Panero F, Volpicelli G, Apra F (2014) Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation. Crit Ultrasound J 6:8
Zhou P, Zhang Z, Hong Y, Cai H, Zhao H, Xu P et al (2017) The predictive value of serial changes in diaphragm function during the spontaneous breathing trial for weaning outcome: a study protocol. BMJ Open 7:e015043
Samanta S, Singh RK, Baronia AK, Poddar B, Azim A, Gurjar M (2017) Diaphragm thickening fraction to predict weaning—a prospective exploratory study. J Intensive Care 5:62
Blumhof S, Wheeler D, Thomas K, Mccool F, Mora J (2016) Change in diaphragmatic thickness during the respiratory cycle predicts extubation success at various levels of pressure support ventilation. Lung 194:519–525
Hayat A, Khan A, Khalil A, Asghar A (2017) Diaphragmatic excursion: does it predict successful weaning from mechanical ventilation? J Coll Physicians Surg Pak 27:743–746
PubMed Google Scholar
Haji K, Royse A, Tharmaraj D, Haji D, Botha A, Royse C (2015) Diaphragmatic regional displacement assessed by ultrasound and correlated to subphrenic organ movement in the critically ill patients—an observational study. J Crit Care 30:439.e7–439.e13
Yoo J-W, Lee SJ, Lee JD, Kim HC (2018) Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success. Korean J Intern Med 33:331–339
Dhungana A, Khilnani G, Hadda V, Guleria R (2017) Reproducibility of diaphragm thickness measurements by ultrasonography in patients on mechanical ventilation. World J Crit Care Med 6:185–189
Dres M, Dubé B-P, Mayaux J, Delemazure J, Reuted D, Brochard L et al (2017) Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med 195:57–66
Chien JY, Lin MS, Huang YCT, Chien YF, Yu CJ, Yang PC (2008) Changes in B-type natriuretic peptide improve weaning outcome predicted by spontaneous breathing trial. Crit Care Med 36:1421–1426
Luo L, Li Y, Chen X, Sun B, Li W, Gu W et al (2017) Different effects of cardiac and diaphragm function assessed by ultrasound on extubation outcomes in difficult-to-wean patients: a cohort study. BMC Pulm Med 17:161
Silva S, Ait Aissa D, Cocquet P, Hoarau L, Ruiz J, Ferre F et al (2017) Combined thoracic ultrasound assessment during a successful weaning trial predicts postextubation distress. Anesthesiology 127:666–674
Haji K, Haji D, Canty DJ, Royse AG, Green C, Royse CF (2018) The impact of heart, lung and diaphragmatic ultrasound on prediction of failed extubation from mechanical ventilation in critically ill patients: a prospective observational pilot study. Crit Ultrasound J 10:13
Yang KL, Tobin MJ, Presberg KW (1991) A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Eng J Med 324:1445–1450
Karthika M, Al Enezi FA, Pillai LV, Arabi YM (2016) Rapid shallow breathing index. Ann Thorac Med 11:167–176
Epstein SK (1995) Etiology of extubation failure and the predictive value of the rapid shallow breathing index. Am J Respir Crit Care Med 152:545–549
Banerjee A, Mehrotra G (2018) Comparison of lung ultrasound-based weaning indices with rapid shallow breathing index: are they helpful? Indian J Crit Care Med 22:435–440
Pirompanich P, Romsaiyut S (2018) Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J intensive care 6:6
Huang D, Ma H, Zhong W, Wang X, Wu Y, Qin T et al (2017) Using M-mode ultrasonography to assess diaphragm dysfunction and predict the success of mechanical ventilation weaning in elderly patients. J Thorac Dis 9:3177–3186
Palkar A, Mayo P, Singh K, Koenig S, Narasimhan M, Singh A et al (2018) Serial diaphragm ultrasonography to predict successful discontinuation of mechanical ventilation. Lung 196:363–368
Palkar A, Narasimhan M, Greenberg H, Singh K, Koenig S, Mayo P et al (2018) Diaphragm excursion-time index: a new parameter using ultrasonography to predict extubation outcome. Chest 153:1213–1220
Haaksma M, Roel Tuinman P, Heunks L (2017) Ultrasound to assess diaphragmatic function in the critically ill-a critical perspective. Ann Transl Med 5:114
Hatam N, Goetzenich A, Rossaint R et al (2014) A novel application for assessing diaphragmatic function by ultrasonic deformation analysis in noninvasively ventilated healthy young adults. Ultraschall der Medizin Eur J Ultrasound 35:540–546
Orde SR, Boon AJ, Firth DG, Vilarrage HR, Sekiguchi H (2015) Diaphragm assessment by two dimensional speckle tracking imaging in normal subjects. BMC Anesthesiol 16:43
Skaarup SH, Løkke A, Laursen CB (2018) The Area method: a new method for ultrasound assessment of diaphragmatic movement. Crit Ultrasound J 10:15
Sharma A, Karna ST, Tandon M, Pandey CK, Chaturvedi R, Vyas V et al (2018) Use of ultrasound-guided preoperative diaphragmatic thickness as a predictor of postoperative weaning failure in recipients and donors scheduled for living donor liver transplant surgery. Saudi J Anaesth 12:406–411
Marchioni A, Castaniere I, Tonelli R, Fantini R, Fontana M, Tabbi L et al (2018) Ultrasound-assessed diaphragmatic impairment is a predictor of outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease undergoing noninvasive ventilation. Crit Care 22:109
Antenora F, Fantini R, Iattoni A, Castaniere I, Sdanganelli A, Livrieri F et al (2017) Prevalence and outcomes of diaphragmatic dysfunction assessed by ultrasound technology during acute exacerbation of COPD: a pilot study. Respirology 22:338–344
Eryüksel E, Cimşit C, Bekir M, Cimsit C, Karakurt S (2017) diaphragmatic thickness fraction in subjects at high-risk for COPD exacerbations. Respir Care 62:1565–1570
Download references
Authors’ contributions
PT wrote and devised the manuscript. SA provided the ultrasound images for the figures and assisted in the literature search. IW assisted in the editing and writing of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Competing interests.
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Ethical approval and consent to participate, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Critical Care Unit, Royal Liverpool University Hospital, Liverpool, UK
Peter Turton, Sondus ALAidarous & Ingeborg Welters
Institute of Aging and Chronic Disease, University of Liverpool, Liverpool, UK
Peter Turton & Ingeborg Welters
Institute of Infection and Global Health, University of Liverpool, Liverpool, UK
Sondus ALAidarous
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Peter Turton .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Cite this article.
Turton, P., ALAidarous, S. & Welters, I. A narrative review of diaphragm ultrasound to predict weaning from mechanical ventilation: where are we and where are we heading?. Ultrasound J 11 , 2 (2019). https://doi.org/10.1186/s13089-019-0117-8
Download citation
Received : 21 December 2018
Accepted : 08 February 2019
Published : 28 February 2019
DOI : https://doi.org/10.1186/s13089-019-0117-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Muscle atrophy
- Diaphragm ultrasound
- Thickening fraction
Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success
Affiliations.
- 1 Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 2 Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Gyeongsang National University Hospital, Jinju, Korea.
- PMID: 29050461
- PMCID: PMC5840594
- DOI: 10.3904/kjim.2016.152
Background/aims: Both diaphragmatic excursion and change in muscle thickening are measured using ultrasonography (US) to assess diaphragm function and mechanical ventilation weaning outcomes. However, which parameter can better predict successful extubation remains to be determined. The aim of this study was to compare the clinical utility of these two diaphragmatic parameters to predict extubation success.
Methods: This study included patients subjected to extubation trial in the medical or surgical intensive care unit of a university-affiliated hospital from May 2015 through February 2016. Diaphragm excursion and percent of thickening change (Δtdi%) were measured using US within 24 hours before extubation.
Results: Sixty patients were included, and 78.3% (47/60) of these patients were successfully extubated, whereas 21.7% (13/60) were not. The median degree of excursion was greater in patients with extubation success than in those with extubation failure (1.65 cm vs. 0.8 cm, p < 0.001). Patients with extubation success had a greater Δtdi% than those with extubation failure (42.1% vs. 22.5%, p = 0.03). The areas under the receiver operating curve for excursion and Δtdi% were 0.836 (95% confidence interval [CI], 0.717 to 0.919) and 0.698 (95% CI, 0.566 to 0.810), respectively ( p = 0.017).
Conclusions: Diaphragm excursion seems more accurate than a change in the diaphragm thickness to predict extubation success.
Keywords: Diaphragm; Excursion; Extubation; Thickness; Ultrasonography.
Publication types
- Comparative Study
- Airway Extubation* / statistics & numerical data
- Diaphragm / diagnostic imaging*
- Diaphragm / physiopathology
- Middle Aged
- Prospective Studies
- Retrospective Studies
- Ultrasonography
- Ventilator Weaning / statistics & numerical data
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Appl Basic Med Res
- v.10(4); Oct-Dec 2020
Ultrasonographic Assessment of Diaphragmatic Excursion and its Correlation with Spirometry in Chronic Obstructive Pulmonary Disease Patients
Mahvish qaiser.
Department of Rehabilitation Sciences, SNSAH, Jamia Hamdard, India
Abhinav Jain
1 Department of Radiodiagnosis, Hamdard Institute of Medical Sciences and Research, New Delhi, India
Introduction:
Chronic obstructive pulmonary disease (COPD) is a common disease. Spirometry is a standard method of assessment of severity of COPD. We evaluate utility of diaphragmatic excursion using ultrasonography in COPD patients and compare this technique with spirometry.
Twenty-six COPD patients and 18 self-reported healthy controls were included in this study. After taking the sociodemographic data, measurement of diaphragm excursion was done using M-mode and B-mode ultrasound. Lung function was assessed by spirometry.
In the COPD group, diaphragmatic excursion was found to be reduced, and it correlates with forced expiratory volume in 1 s (FEV1)/forced vital capacity, whereas it did not correlate with FEV1.
Conclusion:
Ultrasound assessment of diaphragmatic excursion is an easy, noninvasive, and readily available diagnostic tool and correlates with spirometry in estimation of severity of COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common preventable and treatable disease as per the Global Initiative for Chronic Obstructive Lung Disease (GOLD) and is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.[ 1 ]
According to the GOLD report, COPD is projected to be the third leading cause of death by 2020, and currently, it is the fourth.[ 2 , 3 ] The Global Burden of Disease Study done in 2013 attributed COPD as the cause of death for >3 million people that constitutes 6% of all deaths globally.[ 2 ] A review of the published reports revealed 384 million cases of COPD in 2010 which is 11.7% globally.[ 4 ] This makes COPD a leading cause of morbidity and mortality, thus causing huge economic and social burden on the society.[ 3 , 5 ] As per the WHO estimates, 90% of COPD-related deaths occur in developing countries. India and China alone account for 66% of global COPD mortality which is approximately 33% of the total human population.[ 6 , 7 ]
COPD impairs the function of diaphragm muscle which is the primary muscle of inspiration. Diaphragm provides 75% of the increase in lung volume during quiet inspiration.[ 8 ] Movement of diaphragm during breathing is called diaphragm mobility. Movement of diaphragm from end-expiration to full inspiration is known as diaphragm excursion.
Diaphragmatic mobility has been found to be lower in patients with COPD than in healthy elderly individuals due to hyperinflated chest.[ 9 ] COPD patients with thoracic hyperkyphosis have lower diaphragm mobility than those without it. An increase in kyphosis angle decreases the diaphragmatic mobility.[ 10 ]
Ultrasonography is a cost-effective, radiation-free, widely available, and real-time investigation.[ 11 ] Many studies have proposed the possible use of ultrasonography to measure the diaphragmatic excursion.[ 11 , 12 , 13 , 14 ] Although, the literature is limited. Spirometry is a noninvasive, easy, and valid tool for COPD assessment. There are established criteria based on spirometry, according to which COPD can be classified as mild, moderate, severe, and very severe.[ 1 , 9 ] Our study evaluates the diaphragmatic excursion on the basis of preestablished protocols and compares the outcome with the spirometry results. This study explores a new opportunity of using standard ultrasonography as a tool to establish the diagnosis of COPD and assess the severity of the same.
Materials and Methods
The study was conducted between January and April 2020 at a tertiary care hospital. Forty-four study participants were recruited from chest OPD of our hospital after their due informed consent. Out of these, 26 were COPD patients who were labeled as study group and 18 were non-COPD patients who were labeled as control group. For the COPD group, only those patients who did not require oxygen supplementation and were clinically stable were recruited. Both smokers and nonsmokers were recruited in both the groups.
The exclusion criteria included any patient with recent COPD exacerbation in the last 3 months, patients with comorbidities such as cardiac disease, pulmonary fibrosis, or ankylosing spondylitis, or patients who were unable to understand and perform the test.
All these patients underwent spirometry and ultrasonographic assessment of diaphragmatic excursion on the same day as per the below-mentioned protocol. These patients and controls were randomized so that the spirometry observer and radiologist were blinded for the cases and controls.
All participants underwent a detailed postbronchodilator spirometry examination using a calibrated Spirolab III MIR Spirometer in sitting position. Spirometry was performed thrice by experienced technicians at our pulmonary function laboratory. Patients were asked to take a maximal inspiration and then to forcefully expel air for as long and as quickly as possible. Results were recorded and saved for statistical analyses.[ 15 ]
Ultrasonography
Ultrasound assessment of diaphragmatic excursion was done by experienced ultrasonologists. Diaphragmatic excursion for patients was measured on GE make, Voluson S8 series ultrasound machine. The assessment was done in supine position using M-mode and B-mode techniques in quiet and deep breathing scenarios. For M-mode assessment, the transducer was placed in the subcostal region at the midclavicular line with probe tilted cranially, and for B-mode assessment, patients were scanned by placing the transducer in the subcostal region at the midclavicular line with probe tilted horizontally[ 12 , 13 ] [ Figure 1 ]. Ultrasonologists were blinded about the spirometry results.

Ultrasound images on diaphragm (arrow). (a) M-Mode scan done at the midclavicular line to assess diaphragmatic motility. (b) B-Mode acquisition shown here as a still from cine-loop image obtained to measure diaphragmatic excursion
Sample size calculation
The sample size required for 40+ years of age group COPD in our district is 1,000,000 individuals which was calculated based on the assumption that the lowest prevalence of COPD in our district is about 4.75% with an absolute precision of 5%, CI of 80%, and design effect as 1.[ 6 , 15 , 16 ]
Sample size formula n = (DEFF * N*p*q]/[(d2/Z2 1-α/2* (N-1) +p*q].
Statistical analysis
Data was analyzed using IBM SPSS statistical package for Linux version 16.0. Bangalore, India. Demographic data were analyzed using independent samples t-test. Diaphragmatic excursion and lung function were analyzed by an independent t-test. To analyze the relationship between lung function and diaphragmatic excursion, Karl Pearson's correlation coefficient test was used. The level of significance was <0.05 ( P < 0.05).
Forty-eight participants were included in the study. Out of those, 30 were COPD and 18 were non-COPD. Four COPD patients were dropouts. Therefore, their data were not included in this study. Nineteen were male COPD and 11 were healthy male. The rest of them are females. Table 1 shows the mean and standard deviation of different variables in both the groups.
Mean and standard deviation data of study and control groups
FEV 1 : Forced expiratory volume in 1 s; FVC: Forced vital capacity, DE: Diaphragmatic excursion
Independent t -test between the groups revealed that diaphragmatic mobility and lung function are reduced in COPD patients than healthy controls with level of significance <0.01 ( P < 0.01).
Pearson's correlations between diaphragmatic excursion and lung measurements showed a positive strong correlation between forced expiratory volume in 1 s/forced vital capacity (FEV1/FVC) with M-mode ( r = 0.75) [ Table 2 and Figure 2 ] and B-mode ( r = 0.85) in the study group [ Table 3 and Figure 3 ], but this relationship was not found in control controls. There is a weak correlation between FEV1 and M-mode in the study group. There is a strong correlation between M-mode and FEV1 ( r = − 0.50) in the control group.
Relationship between diaphragmatic excursion (M-mode) and variables in study group
FEV 1 : Forced expiratory volume in 1 s; FVC: Forced vital capacity, SD: Standard deviation

Correlation between forced expiratory volume in 1 s/forced vital capacity and M-mode in study group
Relationship between diaphragmatic excursion (B-mode) and variables in study group

Correlation between forced expiratory volume in 1 s/forced vital capacity and B-mode in experimental group
Finally, we observed that diaphragmatic excursion was significantly reduced in the study group than controls ( P < 0.05). Spirometry measurements showed a significant difference between the groups. FEV1/FVC is significantly reduced in COPD [ Table 1 ].
The study establishes that COPD affects diaphragmatic excursion and lung function. We found that diaphragmatic excursion was reduced in COPD than controls. Decreased diaphragmatic excursion shows that contractile ability of diaphragm is reduced in COPD.
The reason of reduced contractility lies in the pathophysiology of the disease. COPD includes bronchitis and emphysema which cause airway obstruction and air trapping in the lungs. Normally, diaphragm moves caudally during inspiration and cranially during expiration. COPD can cause hyperinflation of the lungs, and therefore, diaphragm shifts caudally. This causes mechanical disadvantage of the diaphragm muscle.[ 1 ] Previous studies revealed that reduced diaphragmatic mobility is associated with increased perception of dyspnea. Structural changes cause flattening of the diaphragm which reduces their ability to move cranially and caudally.[ 9 , 10 , 12 ]
Another important outcome of this study is the correlation between sonographic assessment of diaphragmatic excursion and spirometry results. In the present study, we found that diaphragmatic excursion strongly correlates with FEV1/FVC and weakly correlates with FEV1 in the study group. These findings corroborate those of Rocha et al ., who found that diaphragmatic mobility is related to pulmonary parameters (FEV1, FEV1/FVC, FVC, IC, and MVV).[ 9 ] Progression of the disease causes shortening of diaphragm fibers and decreases resting diaphragm muscle length. This causes a decrease in their ventilator capacity and lung function.
COPD causes inflammation and obstruction of the airways that lead to air trapping in the alveoli. As the severity of the disease increases, lung function decreases. COPD can cause hyperkyphosis in later stage which reduces the expansion of the chest wall. A study proved that diaphragmatic mobility is correlated with kyphotic angle.[ 10 ] Hence we can say COPD affects diaphragmatic mobility and lung function.
The limitation of the present study is that only two Stage 4 COPD patients were involved because most of them came to chest OPD with acute exacerbation. Another limitation is that only right hemidiaphragm was assessed on ultrasonography.
Further studies with larger number of patients, especially with severe COPD (Stage 4), would be required covering wider geographical areas for standardized guidelines on assessment of diaphragmatic excursion in COPD patients.
This study describes the use of ultrasonography for assessing the diaphragmatic excursion. Sonographically determined diaphragmatic excursion strongly correlates with FEV1/FVC. Both the B-mode and M-mode approaches can be used to measure the diaphragmatic excursion, and these correlate well with the severity of COPD.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.

IMAGES
VIDEO
COMMENTS
Diaphragmatic excursion is the movement of the thoracic diaphragm during breathing. Normal diaphragmatic excursion should be 3-5 cm, but can be increased in well-conditioned persons to 7-8 cm. This measures the contraction of the diaphragm.
The mean diaphragmatic excursions of the two hemidiaphragms have been determined for men and women (Table (Table1). 1). Furthermore, in 1995, Houston et al have reported that in healthy volunteers, the right-to-left ratio of hemidiaphragmatic excursion during deep inspiration was in the range of 0.5-1.6. Consequently, this ratio has been ...
Check us out on Facebook for DAILY FREE REVIEW QUESTIONS and updates! (https://www.facebook.com/medschoolmadeeasy) Check out our website for TONS OF FREE REV...
Diaphragmatic excursion values presented in this study can be used as reference values to detect diaphragmatic dysfunction in clinical practice. There is a significant statistical difference between right and left hemidiaphragmatic movement during all types of breathing (quiet, deep and sniffing). ...
Furthermore, diaphragmatic excursion is an index for respiratory muscle fatigue during the SBT. Some authors had reported a lower accuracy for diaphragmatic excursion compared to most of the available data and suggested that this lower accuracy is due to the heterogeneity of the patients included in the meta-analyses , . Therefore, separate ...
Diaphragmatic excursion: Can be evaluated via percussion. Is 4-6 centimeters between full inspiration and full expiration. May be abnormal with hyperinflation, atelectasis, the presence of a pleural effusion, diaphragmatic paralysis, or at times with intra-abdominal pathology.
Diaphragm excursion (motion) can be quantified when looking at the diaphragm subcostally . These measurements provide a well-validated method of assessing diaphragm function. Importantly, interpretation of the result is only possible during unassisted breaths because downward displacement during assisted breaths could be a result of passive ...
3. To measure diaphragmatic excursion, ask your patient to inhale and hold it. Percuss from the lower edge of his right scapula down toward the diaphragm (see Technique for percussion). When the note changes from resonant to dull, you've located your first landmark. Tell him to breathe, then mark the landmark with a skin marker.
This video demonstrates diaphragmatic excursion and forced expiratory timeCheck out our website here: https://stethopedia.ca/ ----Instagram: https://www.ins...
The fluoroscopic sniff test, also known as diaphragm fluoroscopy, is a quick and easy real time fluoroscopic assessment of diaphragmatic motor function (excursion).It is used most often to confirm absence of muscular contraction of the diaphragm during inspiration in patients with phrenic nerve palsy or breathing difficulties following stroke.Chest radiograph demonstrating a newly elevated ...
Diaphragmatic excursion is a quantitative measure of expiratory effort as validated by both lung and tracheal volumes in asthma patients, and may be more accurate than qualitative assessment based on tracheal morphology.
Diaphragmatic thickness (Tdi) is measured by placing a high-frequency linear probe at the level of the zone of apposition, while diaphragmatic excursion is measured by placing a curvilinear probe in the subcostal region and recording diaphragmatic movements in the M-mode.
Diaphragmatic ultrasound can also be used in order to predict the weaning outcome. During spontaneous breathing trials, diaphragmatic excursion cutoff values of < 14 mm 53 , 54 and < 11 mm 13 have both been found to be predictive of weaning failure, as have TF values of < 20%, 43 < 30%, 46 and < 36%. 11.
The perpendicular distance between the most caudal point of this line during inspiration and the most caudal point during expiration represents the diaphragmatic excursion. Diaphragmatic thickness and kinetics measures can be affected by the irregular breathing pattern, high respiratory rate, breath to breath variability, and small ...
The diaphragm is the dome-shaped structure that separates the thoracic and abdominal cavities. ... Decreased diaphragmatic excursion may be detected by percussion of the lower rib cage at end ...
In patients with chronic obstructive pulmonary disease (COPD), the maximum level of diaphragm excursion (DEmax) is correlated with dynamic lung hyperinflation and exercise tolerance. This study aimed to elucidate the utility of DEmax to predict the improvement in exercise tolerance after pulmonary rehabilitation (PR) in patients with COPD. This was a prospective cohort study.
The use of ultrasound to visualize the diaphragm is well established. Over the last 15 years, certain indices of diaphragm function, namely diaphragm thickness, thickening fraction and excursion have been established for mechanically ventilated patients to track changes in diaphragm size and function over time, to assess and diagnose diaphragmatic dysfunction, and to evaluate if these indices ...
Background/aims: Both diaphragmatic excursion and change in muscle thickening are measured using ultrasonography (US) to assess diaphragm function and mechanical ventilation weaning outcomes. However, which parameter can better predict successful extubation remains to be determined. The aim of this study was to compare the clinical utility of these two diaphragmatic parameters to predict ...
Diaphragmatic excursions are sensitive to changes in respiratory patterns , are related to the volume-generating capacity of the diaphragm (measured by VC) following abdominal surgery , and have been used to identify diaphragmatic weakness in the setting of the acute exacerbation of COPD . In this ...
The study establishes that COPD affects diaphragmatic excursion and lung function. We found that diaphragmatic excursion was reduced in COPD than controls. Decreased diaphragmatic excursion shows that contractile ability of diaphragm is reduced in COPD. The reason of reduced contractility lies in the pathophysiology of the disease.
Diaphragmatic excursion measured with ultrasound is increasin-gly useful in the thoracoabdominal assessment of patients. Perhaps the most widely used is in the critically ill patient, to define muscle deconditioning, which is crucial in predicting successful extubation in
In this video, Dr. O'Guin will discuss how to stretch the most important muscle in your body, the diaphragm.Diaphragmatic excursion is important for managing...
diaphragmatic excursion: In respiration, the movement of the diaphragm from its level during full exhalation to its level during full inhalation. Normal diaphragmatic excursion is 5 to 7 cm bilaterally in adults. It may be seen during fluoroscopic or ultrasonographic examinations of the chest, or percussed during physical examination of the ...